Massive Pulmonary Embolism as a Rare Cause of Sudden Infant Death: Medico-legal Implications
Received: 23-Oct-2017 / Accepted Date: 30-Nov-2017 / Published Date: 07-Dec-2017 DOI: 10.4172/2572-4983.1000143
Abstract
Sudden death in infants by pulmonary embolism is rarely reported and is often poorly described in literature.
We report the case of an eight-month infant, without past medical history who was admitted into the Emergency Department of a Peripheral Health Center for dyspnea. The diagnosis of bronchopneumopathy was retained. Few hours later, he presented an exacerbation of dyspnea and a marked cyanosis soon followed by death. The autopsy revealed large, obstructive and adherent emboli were found extending into both pulmonary arteries and an associated supportive bronchopneumopathy.
The aim of this reported case is to highlight how much diagnosis of pulmonary embolism can be misleading especially in infant without any risk factor. We discuss also the doctor’s responsibility.
Introduction
Massive pulmonary embolism (MPE) is defined as an embolus causing an important obstruction to the pulmonary flow leading to hemodynamic instability. Pulmonary embolism in infants is an uncommon pathology. Its estimated overall incidence is 1 per 10000 in children while its 1 per 100 in adults [1]. Acute pulmonary embolism as a cause of sudden and unexpected death in infants is a rare phenomenon [2,3]. However, some cases of sudden unexplained death are probably caused by MPE and the incidence may therefore be underestimated.
In infants the signs of lung embolism are various and non-specific. Diagnosis is often challenging, thus, it may be misleadingly and Doctor’s responsibility may be engaged.
We report the case of a sudden and unexpected death in an infant due to lung embolism, diagnosed at the autopsy and we discuss the physician’s responsibility in case of misdiagnosis.
Case Report
An eight months old infant, without past medical history was admitted into the Emergency Department of a Peripheral Health Center for dyspnea. The diagnosis of bronchopneumopathy was retained. The infant has been set under medical treatment associating antibiotic and physiotherapy.
Few hours later, he presented an exacerbation of dyspnea and a marked cyanosis soon followed by death.
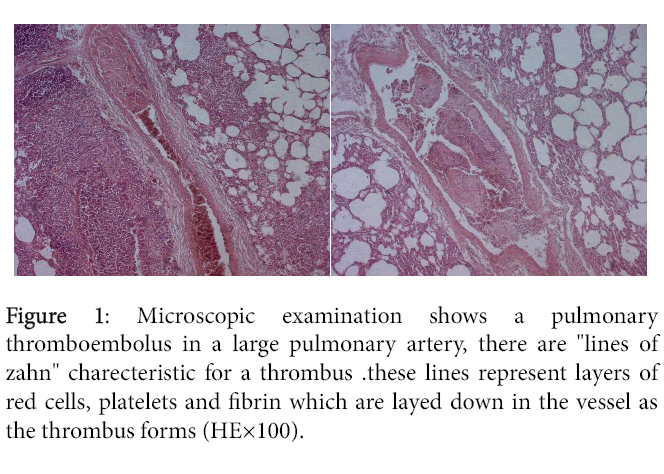
A forensic autopsy was carried out 14 h after the death. External examination showed a baby boy measuring 79 cm and weighing 7400 g. No traumatic injuries were noted on the body and there were a marked facial congestion. At autopsy, the heart weighed 35 g without any evident malformations. The lungs were congestive and edematous. Large, obstructive and adherent emboli were found extending into both pulmonary arteries (Figure 1). No pathological findings were detected in the other organs.
Histological examination confirmed the fibrino-cruoric nature of emboli (Figure 1) and revealed an associated suppurative bronchopneumopathy. Microscopic examination of the other organs didn’t show any pathology.
There were no toxic agents found in toxicological analysis. Death was related to massive pulmonary embolism.
Discussion
The Death by pulmonary embolism remains a very rare cause of death in the infant. A study made over a period of 30 years in the anatomopathology department of Adelarde (country) hospital identified only 3 cases of sudden death by pulmonary embolism in infant [4]. Another study was made in Toronto over a period of 50 years; it only received one case [5].
Risk factors of pulmonary embolism in infant the most reported in the literature are trauma, hydrocephalus, neoplasia, cardiopathy, surgery, dehydration, central venous catheter immobility and local infection [2].
Some others risk factors were reported by other authors. Choi et al. [6] reported in 2016 an unexpected death by pulmonary embolism in an infant. The autopsy showed a vascular malformation which is an aneurysm of the azygos vein.
Ely et al. [7] reported a sudden death by pulmonary embolism in an infant suffering from hereditary occult thrombophilia. Hemophilia and especially thrombopathy is risk factors of pulmonary embolism by inducing the formation of thrombus.
Champ et al. reported three risk factors that would favor the establishment of that pathology which are infection by E. coli , hydrocephalus and idiopathic arterial calcification [4]. In our observation, the local infection seems to be the risk factor having favored installation of this pathology.
Classic symptoms of a pulmonary embolism in infant include dyspnea, chest pain, and hemoptysis [8-10]. However, the presentation of smaller emboli may be inconspicuous and mimic other diseases [2,11]. Furthermore, infant cannot vocalize symptoms such as dyspnea or chest pain, and their excellent cardiopulmonary reserve may understate the hemodynamic effects of a voluminous pulmonary embolism [12,13]. Other signs have been reported in the literature such as unexplained persistent tachypnea, acute right heart failure, cyanosis, dysrhythmia, hypotension, pallor or syncope [12].
Making diagnosis even more difficult the fact that there are no studies determining the sensitivity and specificity of diagnostic tests for pulmonary embolism in infant; The electrocardiogram, chest Xradiography, and arterial blood gas values cannot be relied on to confirm or exclude a diagnosis of PE [14]. Indeed, interpretation of these tests is extrapolated from adult data.
In our case, dyspnea was mistaken as an early sign of bronchopneumopathy and the diagnosis of pulmonary embolism was only made in post-mortem. According to many studies, sudden death represented the most frequent manifestation of pulmonary embolism.
Walden et al. study [15] showed that among 425 autopsies where the diagnosis of pulmonary embolism was retained, only 14% were diagnosed in ante mortem. Another study of Paul Stein et al. [16] was made over 20 years revealed that the diagnosis of pulmonary embolism is unknown before death in 86% of cases.
The reported case showed how much diagnosis of pulmonary embolism can be misleading especially in infant without any risk factor. Previous studies have shown the absence of sensibility or specificity of diagnostic tests. Misdiagnosed cases can lead l professionals to legal suits.
The claims about diagnostic error can be usually subject to trials in both of compensation trial and penal judgment. Doctor can be made responsible in civil law by paying compensation and damages. Also, according to the Tunisian Criminal Code, doctors can be prosecuted under section 225 (involuntary assault by negligence or inattention) which is punishable with imprisonment for a term that may extend to 1 year. They are also being punished for involuntary homicide, if death occurs, under section 217 of the TCC.
In this case, no legal action against the doctor has been started.
Conclusion
The pulmonary embolism in infant is very rare and most often diagnosed in post-mortem during autopsy. The signs of lung embolism are various and non-specific. Also, the diagnostic tests are non-sensible or specific. Thus, diagnosis is often challenging. In case of misdiagnosis Doctor’s responsibility may be engaged.
References
- Lucena J, Rico A, VÃ zquez R, Marin R, Martinez C, et al. (2009) Pulmonary embolism and sudden- unexpected death : Prospective study on 2477 forensic autopsies performed at the Institute of Legal Medicine in Seville. J Forensic Leg Med 16: 196-201.
- Buck JR, Connors RH, Coon WW, Weintraub WH, Wesley JR, et al. (1981) Pulmonary embolism in children. J Pediatr Surg 16: 385-391.
- Jones RH, Sabiston DC (1966) Pulmonary embolism in childhood. Monogr Surg Sci 3: 35-51.
- Champ C, Byard RW (1994) Pulmonary thromboembolism and unexpected death in infancy. J Pediatr, Child Health 30: 550-551.
- Byard RW, Cutz E (1990) Sudden and unexpected death in infancy and childhood due to pulmonary embolism. Arch Patbol Patbol LabMed 114: 142-144.
- Choi J, Song J, Huh J, Kang IS, Ji-Hyuk Y, et al. (2016) Complicated Azygos Vein Anevrysm in an Infant presenting with Acute Pulmonary Thromboembolism. Korean Circ J 46: 264-267.
- Ely SF, Gill JR (2005) Fatal pulmonary thromboembolism and hereditary thrombophilias. J Forensci Sci 50: 411-418.
- Van Ommen CH, Heijboer H, Buller HR, Hirasing RA, Heijmans HAS, et al. (2001) Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr 139: 676-681.
- Kliegman R, Behrman RE, Jenson HB, Stanton BF, (2007) eds. Nelson textbook of pediatrics. Saunders Elsevier. Philadelphia.
- Chan AK, Deveber G, Monagle P, Brooker LA, Massicotte PM (2003) Venous thrombosis in children. J Thromb Haemost 1: 1443–1455.
- David M, Andrew M (1993) Venous thromboembolic complications in children. J Pediatr 123: 337–346.
- Van Ommen CH, Peters M (2006) Acute pulmonary embolism in childhood. Thromb Res 118: 13-25.
- Carson JL, Kelley MA, Duff A (1992) The clinical course of pulmonary embolism. N Engl J Med 326: 1240–1245.
- Dalen JE (2002) Pulmonary embolism: what have we learned since Virchow? Natural history, pathophysiology, and diagnosis. Chest 122: 1440–1456.
- Walden R, Bass A, Modan R, Adar R (1989) Pulmonary embolism in postmortem material with clinical correlation in 425 cases. Int Angiol 4: 469-473.
- Stein PD, Kayali F, Olson RE (2004) Estimated case fatality rate of pulmonary embolism, 1979 to 1998. Am J Cardiol 93: 1197-1199.
Citation: Sahnoun M, Jedidi M, Gorgi M, Guerfala M, Masmoudi T, et al. (2017) Massive Pulmonary Embolism as a Rare Cause of Sudden Infant Death: Medico-legal Implications. Neonat Pediatr Med 3: 143. DOI: 10.4172/2572-4983.1000143
Copyright: © 2017 Sahnoun M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7579
- [From(publication date): 0-2017 - Nov 29, 2025]
- Breakdown by view type
- HTML page views: 6614
- PDF downloads: 965