Case Report Open Access
Multiple Infarctions Due to Vertebral Arterial Occlusion Associated with Atlantoaxial Subluxation in Patients with Rheumatoid Arthritis: A Case Report
Yamada T, Yoshii T*, Egawa S, Hirai T, Inose H and Okawa A
Department of Orthopaedic Surgery, Tokyo Medical and Dental University, Bunkyo-ku, Tokyo, 113-8510, Japan
- *Corresponding Author:
- Toshitaka Yoshii
Department of Orthopaedic Surgery
Graduate School
Tokyo Medical and Dental University
1-5-45 Yushima, Bunkyo-ku
Tokyo, 113-8510, Japan
Tel: +81-3-5803-5272
Fax: +81-3-5803-5281
E-mail: yoshii.orth@tmd.ac.jp
Received Date: May 08, 2017; Accepted Date: May 19, 2017; Published Date: May 25, 2017
Citation: Yamada T, Yoshii T, Egawa S, Hirai T, Inose H, et al. (2017) Multiple Infarctions Due to Vertebral Arterial Occlusion Associated with Atlantoaxial Subluxation in Patients with Rheumatoid Arthritis: A Case Report. OMICS J Radiol S2:003. doi: 10.4172/2167-7964.S2-003
Copyright: © 2017 Yamada T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Rheumatoid Arthritis (RA) is associated with a high incidence of destruction of multiple joints, including Atlantoaxial Subluxation (AAS). Because the Vertebral Arteries (VA) is near the Atlantoaxial (AA) joint, VA occlusion may occur due to AAS. Since the VA supplies blood to the cerebellum and brainstem, serious symptoms can develop if infarction occurs due to VA occlusion. In this case report of a 64-year-old female RA patient, CT angiography demonstrated a dissecting aneurysm and the occlusion of the left VA at the AA joint, attributed to the one-sided destruction of the C1/C2 lateral mass, leading to frequent cerebellum infarctions. Vertigo and neck pain in the extension position disappeared after C1/C2 posterior fixation, and infarctions originating from VA occlusion never recurred after surgery. As the positional occlusion of VA in AAS itself has become relatively uncommon since the use of biological preparations for RA treatment, the authors describe a case in which C1/C2 fixation is effective for preventing neck pain, deterioration of neurological findings and the recurrence of cerebellum infarctions due to positional VA occlusion.
Keywords
Atlantoaxial subluxation; Positional occlusion; Septic emboli
Introduction
Rheumatoid Arthritis (RA) is associated with a high incidence of destruction of multiple joints, including Atlantoaxial Subluxation (AAS). AAS is characterized by excessive movement at the junction between the atlas (C1) and axis (C2) because of either a bony or a ligamentous abnormality. Because the Vertebral Arteries (VA) are near the Atlantoaxial (AA) joint, VA occlusion may occur due to AAS. Since the VA supplies blood to the cerebellum and brainstem, serious symptoms can develop if infarction in these region occurs due to VA occlusion. These types of lesions with a difficult diagnosis have been reported previously, and three-dimensional computed tomography angiography (3D-CTA) of the VA and Doppler ultrasonography were useful for making a definite diagnosis [1,2]. In this case, report of an RA patient, CTA demonstrated a dissecting aneurysm and the occlusion of the left VA at the AA joint, attributed to the one-sided destruction of the C1/C2 lateral mass, leading to frequent occurrence of cerebellum infarctions.
The positional occlusion of VA in AAS itself has become relatively uncommon since the use of biological preparations for RA treatment [3]. Here, we describe a case in which C1/C2 fixation is effective for preventing the recurrence of cerebellum infarctions due to positional VA occlusion.
Case Report
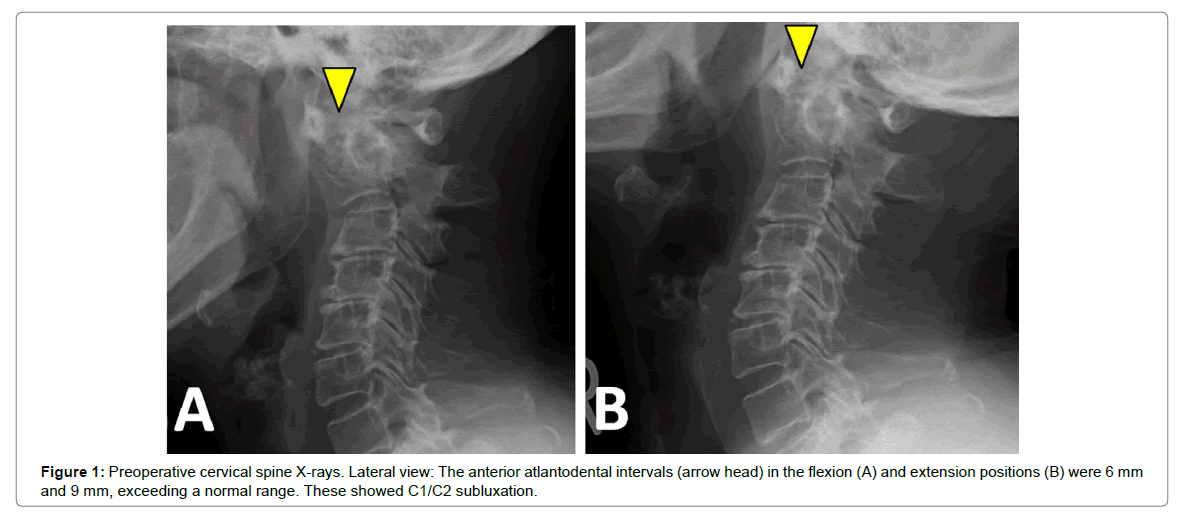
A 64-year-old female with a 34-year history of RA complained of slight neck pain and frequent dizzy spells in the extension position. She had taken predonine (3 mg/day) and methotrexate (10 mg/week), which was followed up by radiographic examinations every six months. The alignment was kyphotic at the C2-5 level. The Anterior Atlantodental Intervals (AADI) in the flexion and extension positions were 6 mm and 9 mm, respectively, in the lateral radiographs (Figures 1A and 1B). Her Ranawat value in the neutral position was 12 mm, indicating AAS with mild vertical subluxation (VS) without neurological deficits. Four years later, she complained of severe rolling vertigo and nausea (Glasgow Coma Scale score = 12).
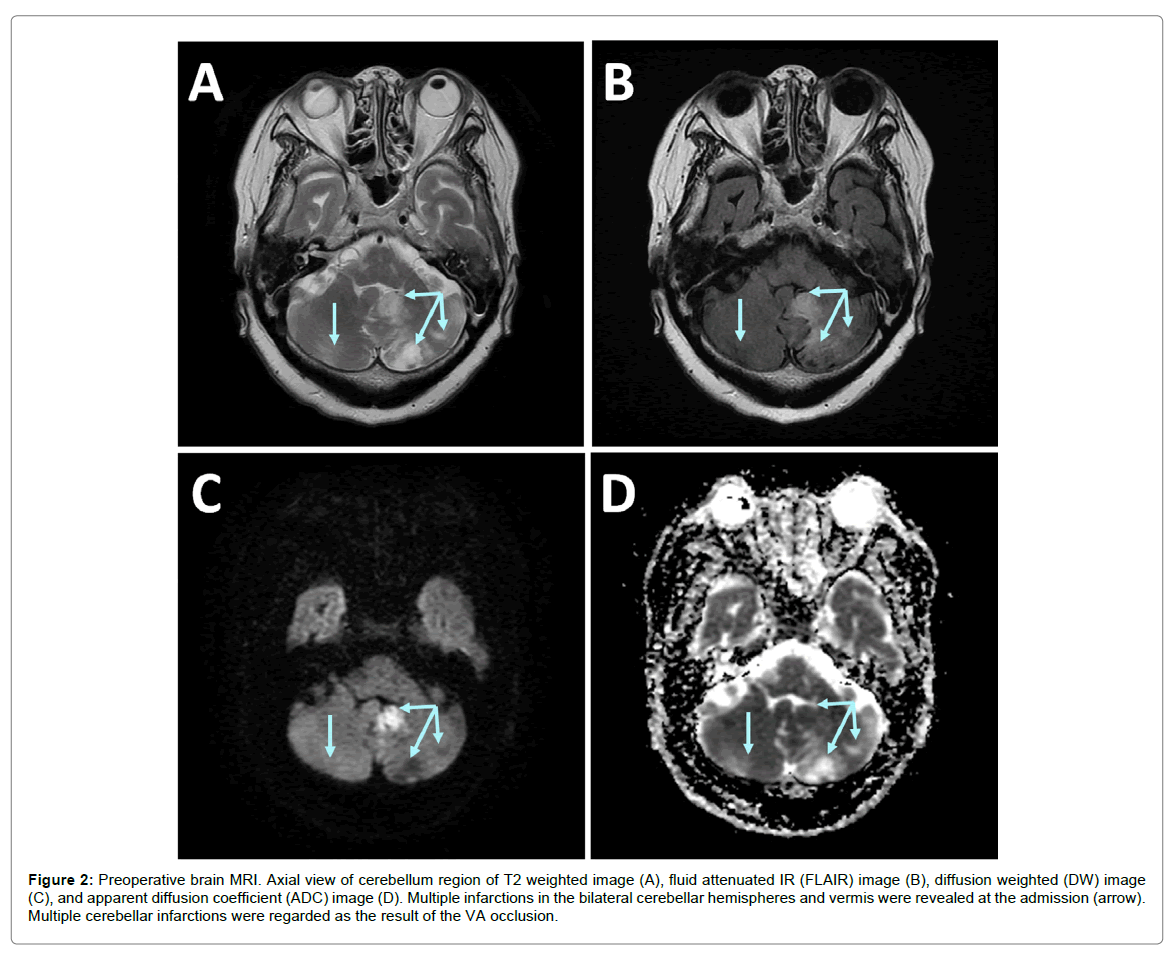
There was no sign of cervical myelopathy, but she suffered from severe neck pain in the neck extended position and from gait disturbance due to dizziness. Her vital signs were stable, apart from transient tachycardia with Atrial Fibrillation (AF) that had never been treated. On cranial magnetic resonance imaging (MRI), acute infarctions in the bilateral cerebellar hemispheres and vermis were revealed at admission (Figures 2A-D). The left posterior inferior cerebellar artery and right superior cerebellar artery were considered involved in these infarctions. Although anticoagulation therapy with heparin and warfarin was initiated conservatively for the treatment of AF and to prevent the recurrence of cerebral infarction, a new infarction in the left cerebellar hemisphere was found 2 weeks after admission.
Figure 2: Preoperative brain MRI. Axial view of cerebellum region of T2 weighted image (A), fluid attenuated IR (FLAIR) image (B), diffusion weighted (DW) image (C), and apparent diffusion coefficient (ADC) image (D). Multiple infarctions in the bilateral cerebellar hemispheres and vermis were revealed at the admission (arrow). Multiple cerebellar infarctions were regarded as the result of the VA occlusion.
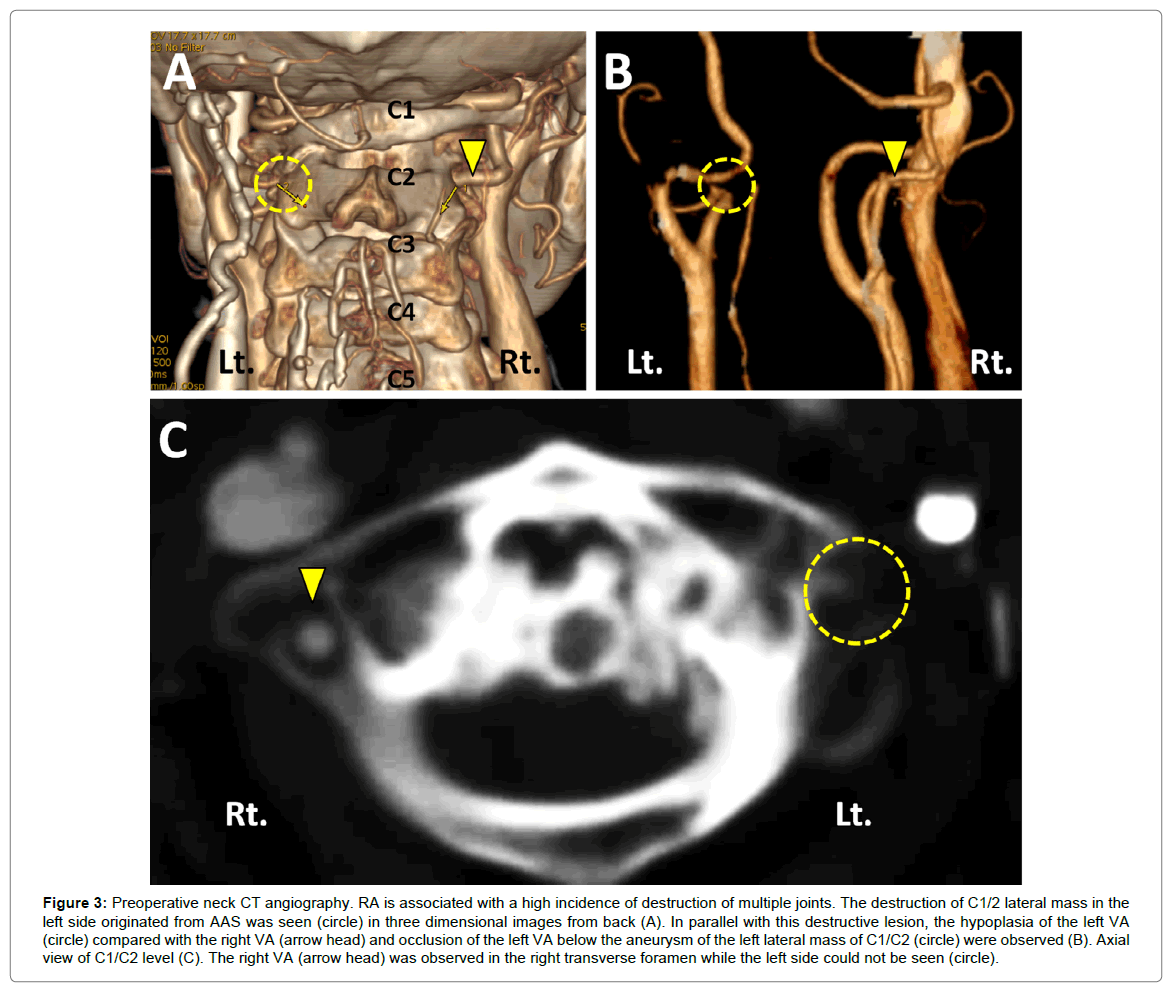
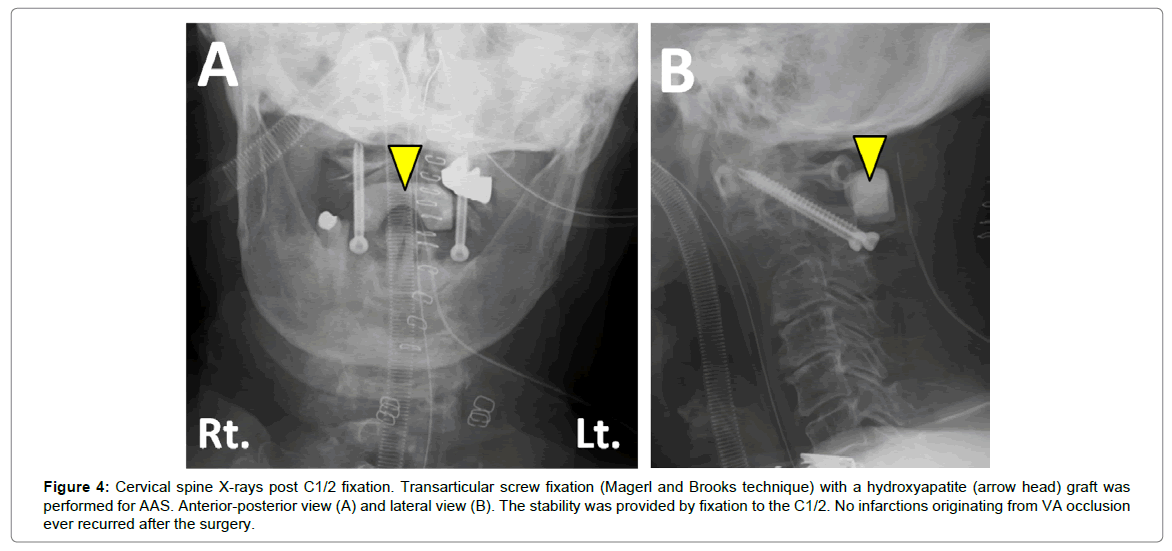
Cervical CTA in the slight extension position demonstrated the destruction of a C1/2 lateral mass in the left side originating from AAS (Figure 3A). It also showed hypoplasia and occlusion of the left VA below the aneurysm of the left lateral mass of C1/C2 (Figures 3B and 3C). Angiography revealed a dissecting aneurysm in the left VA at the C1/C2 level, where there were concerns about bleeding or causing ischemia. The occlusion or ischemia of VA due to this aneurysm following C1/C2 subluxation was suspected. Because this aneurysm could not be managed by endovascular embolization using detachable coils or stents as for a region, a posterior C1/C2 fusion at the reduced position was performed 6 weeks after the first infarction. Transarticular screw fixation (Magerl and Brooks technique [4,5]) with a hydroxyapatite graft was chosen based on consideration of the C2 deformity and anatomical variation in the path of the VA (Figures 4A and 4B). No surgical complications occurred, and her complaint of neck pain and vertigo in the extension position disappeared. After the discharge of hospital, she suffered from severe Pneumocystis Pneumonia (PCP), and subsequently acute cerebral infarction due to thrombophilia or septic embolization occurred at the area governed by the internal carotid artery 6 weeks after the surgery. However, no infarctions originating from VA occlusion ever recurred after the surgery.
Figure 3: Preoperative neck CT angiography. RA is associated with a high incidence of destruction of multiple joints. The destruction of C1/2 lateral mass in the left side originated from AAS was seen (circle) in three dimensional images from back (A). In parallel with this destructive lesion, the hypoplasia of the left VA (circle) compared with the right VA (arrow head) and occlusion of the left VA below the aneurysm of the left lateral mass of C1/C2 (circle) were observed (B). Axial view of C1/C2 level (C). The right VA (arrow head) was observed in the right transverse foramen while the left side could not be seen (circle).
Figure 4: Cervical spine X-rays post C1/2 fixation. Transarticular screw fixation (Magerl and Brooks technique) with a hydroxyapatite (arrow head) graft was performed for AAS. Anterior-posterior view (A) and lateral view (B). The stability was provided by fixation to the C1/2. No infarctions originating from VA occlusion ever recurred after the surgery.
Discussion
Patients with upper cervical RA often have neurological symptoms associated with compression of the spinal cord or the brain stem, while some patients develop thromboembolic stroke related to positional and transient VA occlusions [1]. The VA ascends laterally to the transverse foramen of C2, and from there, the segment emerges and sweeps laterally to pass through the transverse foramen of C1. Because of this serpentine path, the positional occlusion/stasis of VA is sometimes attributed to AAS associated with RA. Since Gaikwad et al. reported an RA patient who had multiple posterior circulation infarctions; the positional occlusion of the VA associated with RA has been regarded as an uncommon case [6]. The prevalence of positional VA occlusion has been reported to be 6% for RA patients whose AADI was greater than 5.0 mm [1]. As mentioned before, 3D-CTA of the VA and Doppler ultrasonography were useful for making this diagnosis [1,2]. A MRI of the cervical spine with time-of-flight MRA of the neck arteries in flexion and extension position may provide valuable information to demonstrate the positional effect on VA.
Atlantoaxial fixation in RA patients provided a better outcome for cervical spine function, with the improvement of pain or numbness in the neck, shoulders, and upper extremities, and the improvement of lower-extremity function [7]. Furthermore, some authors have reported such RA patients to have a good clinical course without recurrent infarctions after posterior fusion [1,6,8]. In this case, the aneurysm in the left VA at the C1/C2 level was difficult to manage by endovascular intervention because of the anatomical feature of VA: these C1 and C2 segments of VA change its direction steeply. Due to the risk for endovascular treatment at this region, a posterior C1/2 fixation was chosen. To avoid positional VA occlusion and a dissecting aneurysm, C1/2 transarticular screw fixation, which is technically demanding due to anatomical variation in the path of the VA [9,10], was performed under a navigation system. As a result, the patient’s symptoms were improved and the recurrence of cerebellum infarctions due to positional VA occlusion never occurred after the surgery.
After the discharge of the hospital, she suffered from severe pneumocystis pneumonia PCP and subsequently new infarction occurred at the area governed by the internal carotid artery. Atheroma or stenosis of the internal carotid artery could not be found and AF with tachycardia completely disappeared after antiarrhythmic therapy. In addition, venous thrombosis was also found in inferior vena in CT. As it is known that immunosuppressed RA patient likely suffer from severe infectious diseases and secondary thrombophilia or embolism [11-13], thrombophilia due to PCP or septic embolization was strongly suspected. Although the new infarction occurred in entirely different pathogenesis based on the immunosuppression of RA, we consider that C1/C2 fixation was effective for stabilizing the atlantoaxial joint and preventing neck pain, deterioration of neurological findings and the recurrence of cerebellum infarctions due to the positional VA occlusion.
Conclusion
The transarticular fixation of C1/2 is effective for stabilizing the atlantoaxial joint and preventing the recurrence of cerebellum infarctions due to positional VA occlusion.
Consent
Written informed consent was obtained from the patient to publish this case report and any accompanying images. A copy of the written consent is available for review by the editors of this journal.
Acknowledgement
We thank Dr. Naoki Yamamoto from the Section of Orthopaedic Surgery, Graduate School, Tokyo Medical and Dental University (Tokyo, Japan) for assistance with the patient’s medical care.
References
- Tateishi Y, Tagami A, Baba H, Osaki M, Kawakami A, et al. (2016) Duplex ultrasonography-detected positional vertebral artery occlusion in upper cervical rheumatoid arthritis. Spine 41: 26-31.
- Yoshitomi H, Neo M, Ito H, Takemoto M, Masaki Y, et al. (2011) Doppler ultrasonography and computed tomography angiography demonstrate positional occlusion of vertebral artery associated with one-sided destruction of the atlantoaxial lateral mass caused by rheumatoid arthritis: a case report. Spine 36: E1493-E1496.
- Takeshima Y, Matsuda R, Hironaka Y, Motoyama Y, Nakase H (2015) Rheumatoid Arthritis–Induced Lateral Atlantoaxial Subluxation With Multiple Vertebrobasilar Infarctions. Spine 40: E186-E189.
- Brooks AL, Jenkins EB (1978) Atlanto-axial arthrodesis by the wedge compression method. J Bone Joint Surg Am 60: 279-284.
- Grob D, Magerl F (1987) Surgical stabilization of C1 and C2 fractures. Der Orthopade 16: 46-54.
- Gaikwad SB, Suri A, Garg A, Kanodia A, Gupta V, et al. (2004) Positional occlusion/stasis of vertebral arteries in a case of cervical rheumatoid arthritis presenting with multiple posterior circulation infarcts. Spine 29: E321-E325.
- Iizuka H, Iizuka Y, Mieda T, Tsunoda D, Kobayashi R, et al. (2017) The clinical outcomes of atlanto-axial arthrodesis in patients with rheumatoid arthritis–Assessment according to the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). J Orthop Sci 22: 401-404.
- Fujiwara H, Kaito T, Makino T, Yonenobu K (2012) Positional occlusion of the vertebral artery in a case of rheumatoid atlantoaxial subluxation presenting with multiple cerebral and cerebellar infarction. Mod Rheumatol 22: 605-609.
- Harms J, Melcher RP (2001) Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine 26: 2467-2471.
- Oda I, Abumi K, Sell LC, Haggerty CJ, Cunningham BW, et al. (1999) Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine 24: 2377-2382.
- Ryu JH, Swensen SJ (2003) Cystic and cavitary lung diseases: focal and diffuse. Mayo Clin Proc 78: 744-752.
- Gupta T, Parikh K, Puri S, Agrawal S, Agrawal N, et al. (2014) The forgotten disease: Bilateral Lemierre’s disease with mycotic aneurysm of the vertebral artery. Am J Case Rep 15: 230-234.
- Papadoulas S, Zampakis P, Liamis A, Dimopoulos PA, Tsolakis IA (2007) Mycotic aneurysm of the internal carotid artery presenting with multiple cerebral septic emboli. Vascular 15: 215-220.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 5681
- [From(publication date):
specialissue-2017 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 4754
- PDF downloads : 927