Neck Injury after Whiplash Trauma in a Defined Population in Northern Sweden – Long-Term Sick Leave and Costs of Low Productivity.
Received: 20-Aug-2014 / Accepted Date: 11-Sep-2014 / Published Date: 18-Dec-2013 DOI: 10.4172/2161-1165.1000170
Abstract
Background: Neck injuries following whiplash trauma can lead to long-term sequelae. Population-based studies covering traffic and non-traffic whiplash trauma are rare. The aim was to describe the incidence of neck injuries following whiplash trauma during one year, from a well-defined area served by a single hospital, and the resulting long-term sick leave during a five-year follow-up. Possible risk factors for sick leave and the cost of lost productivity were also studied.
Methods: From the injury register of Umeå University Hospital, the year 2001’s data set of soft tissue neck injuries and fractures was extracted. Those injured by whiplash trauma were included. The Swedish Social Insurance Agency provided five-year post-injury data on sick leave in 2006. Epidemiological aspects were described, a logistic regression was conducted to find risk factors for long-term sick leave, and the cost of lost productivity was calculated.
Results: Four hundred and seventeen cases were included. The incidence was 383 per 100,000 person-year. In 14% of 18-64 year olds, sick leave was granted for more than two weeks and the median number of sick days in this group was 298. Old age, having a Whiplash Associated Disorders (WAD) grade of 1, being injured in traffic and being injured at velocity exceeding 50 km/h were significant risk factors for sick leave. A few (6%) had fractures, however, their average sick-leave time was not significantly longer than the sick leave of those with only soft tissue injuries. The cost to society for lost productivity was estimated at 4.4 million Euros during the five-year follow-up.
Conclusion: Neck injuries following whiplash trauma arise from both traffic and non-traffic injury events and affect people of all ages. Consequently long-term sick leave occur in a minority of the patients, commonly among older persons and persons injured in traffic. The costs to society from lost productivity is high.
Keywords: Neck injury, Whiplash injury, Sick leave, Epidemiology, Cost of illness
162320Introduction
The incidence of neck injuries following whiplash trauma is believed to be over 300 per 100,000 person-year after traffic collisions [1]. The “true” incidence is, however, difficult to assess because emergency department (ED) reports [2-5], studies based on police reports [6], and insurance company reports [7,8] provide differing figures based on varying definitions and inclusion criteria. Population-based studies covering traffic and non-traffic whiplash trauma are rare. There are two previous ED-reports from Sweden including both traffic and non-traffic injury events. In the first study from 1985-86 including all ages, the incidence of neck injuries was 117 per 100,000 person-year [9]. In the second study from 1988-90 including adults, the incidence was 227 per 100,000 person-year [10]. From the Netherlands, Versteegen et al. reported that the incidence of “neck sprains” from non-traffic injury events among patients of all ages increased from 5.5 per 100,000 person-year in 1970-74 to 24.1 per 100,000 person-year in 1990-94 [5]. During the same period, the incidence of neck injuries following car accidents increased from 3.4 to 40.2 per 100,000 person-year [4].
Persons subject to neck injury following whiplash trauma may experience neck pain, neck stiffness, or other symptoms – whiplash associated disorders (WAD) – such as headache, dizziness or auditory impairment [11,12]. These symptoms resolve within three months in many cases but in 20-50% of the cases, chronic symptoms are reported [13,14]. The return-to-work rate following whiplash injuries was found to be 95% in a 2005 review [15]. More recently, Buitenhuis et al. found 34% of 733 whiplash insurance claimants had some degree of work disability one month after injury, at six months, the figure was 19% and at 12 months 13% had work disability [16]. Jöud et al. showed that the median number of sick days increased from the year prior to the year after a neck injury [17]. The costs to society from neck injuries are large, and indirect costs such as lost productivity holds the lion’s share [18,19]. Chappuis et al. found an average cost per whiplash-claim of 9,000 Euros in ten European countries [20]. The Swedish Society of Medicine and the Whiplash Commission Medical Task Force found that the cost for whiplash injuries in Sweden (9.5 million inhabitants) nears 500 million Euros annually [19].
There is a lack of ED-based cohorts investigating long-term sick leave after neck injuries. Such cohorts will include many of the “mild” neck injury cases that are not included in insurance company records. Thus, the figures presented from ED-based cohorts will better reflect the full spectrum of neck injuries in society and the calculations of cost of injury will be a valuable complement to studies of other design.
Based on a cohort of persons of all ages with neck injuries following a traffic or non-traffic whiplash trauma who attended the ED of a mid-sized Swedish hospital, the aims of the study were:
1. To establish the incidence of neck injuries (WAD 1-4) in the defined population.
2. To describe epidemiological aspects of neck injuries in three age-groups (0-17, 18-64, and ≥65 years).
3. To describe the consequent long-term sick leave (≥15 days) during a five-year follow-up of age group 18-65.
4. To find possible risk factors for long-term sick leave sick leave.
5. To calculate the cost of lost productivity.
Materials and Methods
Patients and procedure
During 2001, 137,000 inhabitants in the well-defined catchment area of Umeå University Hospital comprised the population at risk for having an injury following a traffic or non-traffic injury event demanding medical attention at the emergency department (ED). The hospital is the only one in the area and the distance to the next nearest hospital is 110 km. From 1 Jan 2001 to 31 Dec 2001, 10,493 patients were registered in the injury register of the ED (8,997 non-vehicle related injuries and 1,496 vehicle related injuries). The register contains all types of injuries and the study-specific data set originates from this register.
Upon arrival at the ED, all injured persons were asked to answer a questionnaire about the injury-causing incident. This self-explanatory questionnaire was filled out by the patient or accompanying persons. Data from all available medical records, ambulance and police reports were included in the injury register. Sometimes, information was also gathered from bystanders and relatives. If necessary, supplementary details were retrieved by telephone interviews conducted by one of the injury registers’ coders. These trained administrators then assessed all the information to find all injuries and injury mechanisms. In cases with multiple injuries, up to three additional injuries were registered. By checking against the hospital’s compulsory E-number registration for “external cause”, the problem of losing inpatients from the data set was eliminated [21]. The proportion of registration misses among outpatients was about 10% for non-traffic and 5% for traffic injuries in the monthly quality control of the register (ie, when all registered patients during 3 randomly selected days were compared with all hospital visits for the same period) – these losses were random.
In 2004, extraction of data from the injury register to the study-specific data set was conducted. The following procedure was used: All persons registered by the coders as having an injury localized to the neck were identified (n=568). The questionnaires and the medical records concerning these cases were then re-evaluated by the authors and the patients were included in the study if the following criteria were fulfilled:
1. The neck injury should be caused by a whiplash-like movement to the neck (acceleration-deceleration mechanism [22], thus no cases with a neck injury caused by direct violence to the neck were included (for example a punch). All injury mechanisms from traffic were considered to be whiplash-like.
2. The neck injury should be a strain, sprain, fracture, ligament, or joint injury. No wounds or cuts were included.
3. The injured had to have sought medical attention within 30 days of the incident.
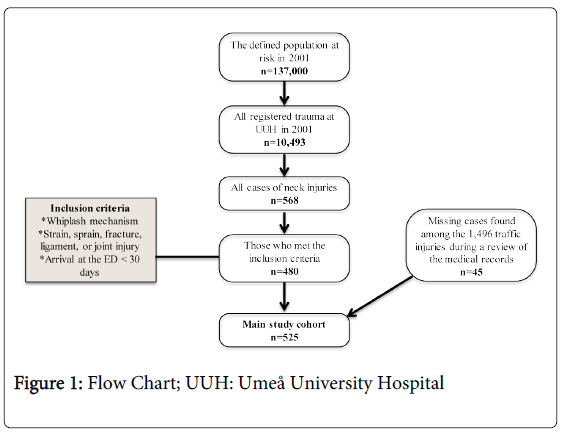
After applying these criteria to the 568 identified cases in the injury register, 480 cases remained. A final effort was then conducted in purpose of finding missing cases among the 1,496 traffic cases. When all questionnaires and medical records were read once more, 45 additional cases were found. Altogether 525 cases of all ages were included in the final data set; see flow chart, Figure 1.
All injuries were assessed to fit within WAD-grade 1-4 [22]. The authors set the WAD-grades in retrospect based on data from the medical records. Because WAD-grades 2 and 3 were difficult to distinguish, they were combined into one group (WAD 2-3). The classification of the injuries’ severity was conducted by one of the authors based on the Abbreviated Injury Scale (AIS) [23]. The scale ranges from 1 (minor injury) to 6 (maximal injury, in most cases fatal). When assessing the velocity of the crashes, the velocity of the vehicle in which the injured person was traveling was registered. Exceptions were when the injured person was travelling in a vehicle that had stopped and was hit by another vehicle; the velocity of the other vehicle was then registered.
Sick leave
All Swedish citizens older than 18 and usually to the retirement age of 65 are compulsory insured and granted economic compensation from the Swedish Social Insurance Agency (SSIA) in case of injury or illness. SSIA administrates and registers payment of sickness benefits and disability pensions. In their database, the cause of sick leave (ICD-10 diagnosis [21] and free text) as well as the degree to which sickness benefits are being granted is registered. All cases in age group 18-64 years (n=417) were, therefore, scrutinized by the authors with assistance from personnel at the SSIA to find sick leave periods that occurred between 2001 and 2006. Because the causes of sick leave are clearly stated in this register, it was possible to include only the sick-leave periods connected to the WAD arising from the specific neck injuries in question. Sick leave periods due to concomitant injuries were excluded. Persons that had sickness benefits due to WAD prior to the injury or previous disability pension were excluded in the calculation of sickness data. In 97% of the cases the data was found. The first 14 days of sick leave are paid by the employer and not registered by SSIA. Sick leave shorter than 15 days are, therefore, not included in our data set.
Cost of lost productivity
The cost of lost productivity was calculated by multiplying the total sick years (1 sick year = 365 days of full-time sick leave) by the yearly cost of one employee, including payroll taxes in Sweden in 2001 (43,100 Euros) [24].
Definitions of categories of injury events
Falls: Horizontal and vertical falls.
Car, bus, or truck crashes: Four-wheel vehicle road crashes.
Other vehicle-related injury events: Bicycle, moped, motorcycle, or snowmobile crashes.
Contact with object: The victim was hit by an object (or another person). This includes sports injuries, assaults, and collision with an object during a fall.
Statistical analysis
PASW Statistics 18 was used (SPSS Inc., Chicago, IL). Medians were presented with interquartile range (IQR) as measure of variability. The difference in the number of cases being granted sick leave in various subgroups was statistically analysed with the Likelihood Ratio-test (G2). Post hoc analysis was conducted using partitioning of the G2-statistics and pairwise comparison using Bonferroni correction [25]. The distribution of sick days within each subgroup was analysed using either the non-parametric Mann-Whitney U-test or the Kruskal-Wallis test. The level of statistical significance was p=0.05. Two clusters of variables were univariate analysed: 1. demographic and injury-specific data; 2. car-specific data. The variables with a p-value of <0.1 when tested for the outcome “sick leave: yes or no” were selected to be included in a logistic regression analysis. Because only one of the variables of car-specific data had a p-value <0.1 (velocity), the significant variables from the demographic and injury-related data were included also in that logistic regression. Because the number of persons on sick leave following fall injuries was zero, that variable could not be included in the logistic regression. We solved this problem by choosing to include vehicle related injury events and non-vehicle related injury events (including falls) in the regression. Additionally, 18-19 year olds had zero sick leave days; thus the age was included in the regression as a continuous variable. The enter-method, which enters all variables concurrently, was used. Nagelkerke R2 was used as a measure of goodness of fit for the models.
Ethics
The Regional Ethical Review Board in Umeå approved the study.
Results
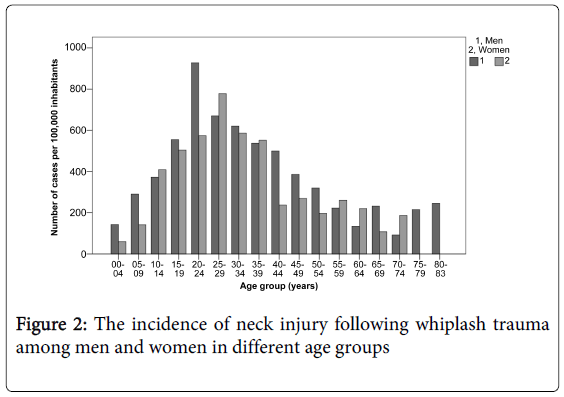
The incidence of neck injury following whiplash trauma was 383 per 100,000 person-year. For additional age and sex-specific incidences (Table 1 and Figure 2).
| n | n per 100,000 person-year (Men; women) | |
|---|---|---|
| All ages | 525 | 383 (429; 338) |
| 0-17 years | 85 | 280 (286; 273) |
| 18-64 years | 417 | 481 (530; 431) |
| ≥65 years | 23 | 115 (175; 70) |
Table 1: The incidence of neck injury following whiplash trauma in children and adolescents, adults, and elderly persons (numbers in bracket are for men and women respectively)
Epidemiological aspects
The 525 cases consisted of 292 (56%) men and 233 (44%) women; the median age was 29 years (IQR 21). The baseline characteristics for children and adolescents, adults, and elderly persons are shown in Table 2. The most common cause of injury was car- bus, or truck-crash (n=320; 61%).
| Children and adolescents (0-17 years) | Adults (18-64 years) | Elderly persons (≥65 years) | |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Sex | |||
| Women | 40 (47) | 185 (44) | 8 (35) |
| Men | 45 (53) | 232 (56) | 15 (65) |
| Type of injury event | |||
| Fall | 31 (37) | 37 (9) | 7 (30) |
| Car/bus/truck-crash | 11 (13) | 300 (72) | 9 (39) |
| Other vehicle crashes | 9 (11) | 24 (6) | 5 (22) |
| Contact with object | 34 (40) | 56 (13) | 2 (9) |
| WAD-grade | |||
| 1 | 20 (24) | 142 (34) | 4 (17) |
| 2-3 | 64 (75) | 266 (64) | 13 (57) |
| 4 | 1 (1) | 9 (2) | 6 (26) |
Table 2: Baseline characteristics in children and adolescents, adults,and elderly persons, Abbreviation: WAD: Whiplash associated disorders.
Three hundred and sixty six (70%) of the patients attended the ED on the day of injury and 514 (98%) within the first week. Of all injured, 64 (12%) were treated as inpatients for a median of one day (IQR 1). Of patients with an isolated neck injury of WAD-grade 1-3 (n=372), only nine (2%) were treated as inpatients. An AIS-score ≥2 (WAD 4 or significant concomitant injuries) was associated with a higher number of inpatient days (data not shown).
All WAD 1-3 injuries were classified as AIS 1. The 16 WAD 4 injuries (3% of the injured) were classified as AIS 2, 3 and 5. Additional injuries were found in 145 patients (28%). Of these, 20 patients (4%) had moderate injuries (AIS 2 - mostly concussions and fractures), three patients (0.6%) had serious injuries (AIS 3 - unstable fractures to the thoracic/lumbar spine or skull base fractures) and four patients (0.8%) had severe injuries (AIS 4 - three subdural hematomas and one ruptured spleen).
Long-term sick leave and its risk factors among adults (ages 18-64)
In 58 (14%) of the 417 patients in age group 18-64, sick leave was granted for ≥15 days. The median number of days on sick leave was 298 (IQR 1074), 36 (62%) of the patients were men and 22 (38%) were women. Eleven (3%) patients were still on 100% sick leave after the five-year follow-up period; two (0.5%) were on 75% sick leave and six (1%) on 50% sick leave. Six of these 19 cases were injured in rear-end car, bus, or truck crashes, three in crashes with initial impact from the front or diagonally from the front, four were involved in rollovers, three were injured in side collisions and one was thrown from his vehicle after a collision. One patient was a bicyclist hit by a car and one was a farmer who was hit in the head by a hay bale. Four of these 19 patients had concomitant injuries of AIS-grade 1 and 1 patient had an AIS 2 injury.
The results of our univariate analysis of baseline and injury-specific data vs. presence of sick leave and the length of sick leave are shown in Table 3. Interesting findings were:
| Presence of sick leave | Duration of sick leave (days) | |||
|---|---|---|---|---|
| n (%) | p-value | Median (IQR) | p-value | |
| Sex | ||||
| Men (n 232) | 36 (16) | 260 (1362) | ||
| Women (n 185) | 22 (12) | 0.285 | 577 (924) | 0.575 |
| Age-group | ||||
| 18-19 (n 24) | 0 (0) | 0 (n/a) | ||
| 20-24 (n 90) | 5 (6) | 140 (561) | ||
| 25-29 (n 78) | 13 (17) | 443 (1189) | ||
| 30-34 (n 57) | 10 (18) | 530 (1768) | ||
| 35-39 (n 51) | 8 (16) | 82 (1218) | ||
| 40-44 (n 32) | 3 (9) | 1372 (n/a) | ||
| 45-49 (n 29) | 6 (21) | 235 (1494) | ||
| 50-54 (n 24) | 8 (33) | 293 (670) | ||
| 55-59 (n 21) | 3 (14) | 1424 (n/a) | ||
| 60-64 (n 11) | 2 (18) | 0.007* | 153 (n/a) | 0.567 |
| Type of injury event | ||||
| Falls (n 37) | 0 (0) | 0 (n/a) | ||
| C.B.T. (n 300) | 51 (17) | 328 (1375) | ||
| O.V.R.E. (n 24) | 3 (13) | 443 (n/a) | ||
| C.W.O. (n 56) | 4 (7) | 0.001** | 125 (729) | 0.906 |
| WAD-grade | ||||
| 1 (n 142) | 27 (19) | 499 (1013) | ||
| 2-3 (n 266) | 29 (11) | 252 (1126) | ||
| 4 (n 9) | 2 (22) | 0.067 | 752 (n/a) | 0.914 |
| Additional injuries | ||||
| None (n 309) | 42 (14) | 330 (1401) | ||
| AIS 1 (n 79) | 12 (15) | 190 (679) | ||
| AIS 2 (n 23) | 3 (13) | 79 (n/a) | ||
| AIS 3 (n 2) | 1 (50) | 1424 (n/a) | ||
| AIS 4 (n 4) | 0 (0) | 0.589 | 0 (n/a) | 0.648 |
Table 3: Sick leave (≥15 days) due to neck injury among the 417 patients in age group 18-64; Univariate analysis of demographic and injury-related data, *Post hoc tests revealed the following results: In the partitioning of G2-test 18-24 year-olds were less prone to be granted sick leave than 25-29 year olds. When doing pairwise comparison using Bonferroni correction 18-19 year olds and 20-24 year olds were less prone to be granted sick leave than 50-54 year olds; **In the two post hoc tests, the number of patients granted sick leave in Falls was significantly lower compared with C.B.T-Crashes; C.B.T.: Car, bus or truck crash; O.V.R.E.: Other vehicle-related injury events; C.W.O.: Contact with object; WAD: Whiplash associated disorders. IQR: Interquartile range
The share of patients granted sick leave for ≥ 15 days after falls was zero.
Those with the most severe neck injuries (WAD 4) had neither significantly higher percentage of sick leave nor longer sick leave, than those with WAD 1-3.
The presence of additional injuries had no significant impact on the length of sick leave due to the neck injury.
There were no significant differences between men and women.
Age, type of injury event, and WAD-grade were further included in the logistic regression because of p-values <0.1. The logistic regression showed that older age, having a WAD-grade of 1, and being injured in vehicle related injury events all were significant risk factors of being granted long-term sick leave, see Table 4.
| OR | 95% CI | p-value | |
|---|---|---|---|
| Age | 1.03 | 1.01-1.06 | 0.004* |
| Type of injury event | |||
| Vehicle related | 1 | - | - |
| Non-vehicle related | 0.22 | 0.08-0.64 | 0.005** |
| WAD-grade | |||
| WAD 1 | 1 | - | - |
| WAD 2-3 | 0.54 | 0.30-0.97 | 0.037*** |
| WAD 4 | 1.19 | 0.22-6.51 | 0.839 |
| Constant | 0.09 | - | <0.001 |
Table 4: Logistic regression of demographic and injury-related data vs. presence of sick leave among 18-64 year olds; R2=0.056-0.101; *For each year a person ages, the odds are 1.03 times higher to be granted sick leave; **Those injured in non-traffic crashes have 0.22 times the odds (less likely) than those injured in traffic to be granted sick leave; ***Those with WAD-grade 2-3 have 0.54 times the odds (less likely) than those with WAD 1 to be granted sick leave; OR: Odds ratio; WAD: Whiplash associated disorders
Long-term sick leave and its risk factors among 18-64 year old car occupants
The second group being analysed regarding sick leave was adult car occupants (n=275). Forty-three of those (16%) were granted sick leave for ≥15 days. The median number of sick days was 268 (IQR 1,414). For univariate analysis of car-specific baseline data vs. the presence of sick leave and duration of sick leave, see Table 5. Those injured in velocity 50-124 km/h had a close to significant higher share of sick leave than those injured in lower velocities. Velocity was, therefore, included in the logistic regression along with age and WAD-grade. Velocity 50-124 km/h and older age proved to be significant risk factors in the logistic regression while WAD-grade did not, see Table 6.
| Presence of sick leave | Duration of sick leave (days) | |||
|---|---|---|---|---|
| n (%) | p-value | Median (IQR) | p-value | |
| Position in the car | ||||
| Driver (n 218) | 34 (16) | 577 (1516) | ||
| Front seat passenger (n 43) | 8 (19) | 152 (1331) | ||
| Back seat passenger (n 13) | 1 (8) | 23 (n/a) | ||
| Unknown (n 1) | 0 (0) | 0.716 | 0 (n/a) | 0.273 |
| Seatbelt | ||||
| Seatbelt (n 239) | 38 (16) | 384 (1517) | ||
| No Seatbelt (n 15) | 2 (13) | 853 (n/a) | ||
| Unknown (n21) | 3 (14) | 0.949 | 49 (n/a) | 0.691 |
| Headrest | ||||
| Headrest (n225) | 35 (16) | 499 (1477) | ||
| No Headrest (n13) | 1 (8) | 217 (n/a) | ||
| Unknown (n37) | 7 (19) | 0.598 | 68 (1400) | 0.915 |
| Airbag | ||||
| Airbag deployed (n10) | 2 (20) | 195 (n/a) | ||
| Airbag did not deploy (n 159) | 20 (13) | 732 (1673) | ||
| Unknown (n106) | 21 (20) | 0.267 | 217 (1421) | 0.444 |
| Direction of impact | ||||
| Back followed by front (n11) | 2 (18) | 475 (n/a) | ||
| Right front (n 4) | 0 (0) | 0 (n/a) | ||
| Right (n 6) | 3 (50) | 1526 (n/a) | ||
| Right back (n 2) | 0 (0) | 0 (n/a) | ||
| Back (n 119) | 18 (15) | 243 (1677) | ||
| Left back (n 1) | 0 (0) | 0 (n/a) | ||
| Left (n18) | 1 (6) | 23 (n/a) | ||
| Left front (n 3) | 1 (33) | 1797 (n/a) | ||
| Front (n 57) | 9 (16) | 252 (1374) | ||
| Rollover (n 19) | 4 (21) | 844 (1295) | ||
| Impact with animal (n 12) | 2 (17) | 96 (n/a) | ||
| Hit a bump (n 1) | 0 (0) | 0 (n/a) | ||
| Unknown (n 22) | 3 (14) | 0.665 | 764 (n/a) | 0.504 |
| Velocity | ||||
| 0-49 km/h (n 60) | 5 (8) | 1062 (1283) | ||
| 50-124 km/h (n 83) | 18 (22) | 248 (1430) | ||
| Unknown (n 132) | 20 (15) | 0.084 | 358 (1285) | 0.228 |
Table 5: Sick leave after whiplash trauma among the 275 18-64 year old car occupants; Univariate analysis of car-specific data; IQR: Interquartile range
| OR | 95% CI | p-value | |
| Velocity | |||
| 0-49 km/h | 1 | - | - |
| 50-124 km/h | 3.52 | 1.20-10.33 | 0.022* |
| Unknown | 1.94 | 0.69-5.51 | 0.211 |
| Age | 1.03 | 1.01-1.06 | 0.021** |
| WAD-grade | |||
| WAD 1 | 1 | - | - |
| WAD 2-3 | 0.65 | 0.33-1.28 | 0.210 |
| WAD 4 | - | - | - |
| Constant | 0.04 | - | <0.001 |
Table 6: Logistic regression of car-specific data with the addition of age and WAD-grade vs. presence of sick leave among 18-64 year old car occupants; R2=0.042-0.073; *Those injured in velocity 50-124 km/h have 3.52 times the odds (more likely) than those injured in velocity 0-49 km/h to be granted sick leave; **For each year a person ages, the odds are 1.03 times higher to be granted sick leave; OR: Odds ration; WAD: Whiplash associated disorders
The cost of lost productivity
The total sick days granted for the 58 patients who were granted sick leave was 36,919 or 101 sick years. This implies that the total cost of lost productivity during the five-year follow-up period was: in total 4.4 million Euros; 75,100 Euros for each of the 58 cases on sick leave; 10,400 Euros for each of the 417 injured persons in age group 18-64 years; 8,300 Euros for each of the 525 injured in all ages.
Discussion
The current study included patients from a defined population who sought care at the ED for neck injuries (WAD 1-4) following whiplash trauma. The cases were analysed with focus on incidence, long-term sick leave (≥15 days), risk factors for sick leave, and finally the associated productivity loss. The primary findings were that the incidence was 383 per 100,000 person-year, 14% of the patients were granted sick leave ≥15 days and 4.5% were still work disabled after five years. Significant risk factors for long-term sick leave were old age, being injured in traffic crashes, and being injured in velocity ≥50 km/h. WAD grade 1 was a significant risk factor in one of two analysed groups. The cost of lost productivity was 75,100 Euros per person on sick leave.
Generally, comparison between ED-based studies on incidence and epidemiology of whiplash injuries are difficult because many studies are limited to, for example, only traffic injuries, only WAD 1-3, or only adults and the method of case collection varies between the studies. In previous studies from the same geographical area using similar inclusion criteria, an incidence of 117 per 100,000 person-year was observed in 1985-86 [9] and an incidence of 227 per 100,000 person-year was described in 1988-90 [10]. The higher incidence found in the present study indicates that an increase in incidence has occurred. Several authors describe this during the last 30 years [1,19]. Why the incidences has increased is unknown, possible explanations include, for example, improved injury registration and increased propensity to attend the ED after neck injuries [2].
The median age, as well as the share of patients injured in traffic, was in line with other studies from our area and other western countries [3-5,9,10,26]. The percentage of men in our study population was higher than in other studies where male/female ratios ranged from 0.3-1.1 [9,27]. A high number of injured men among the cases injured in other vehicle-related injury events and contact with object might explain this because those groups are often not included in studies of neck injuries.
The share of patients granted sick leave was lower than in some other studies: Mayou and Bryant found that 23% of 63 patients had work absence for more than one month [28]. On the other hand, these authors reported that all of those previously employed full-time returned to work within one year [28]. Buitenhuis et al. showed a high rate of sick leave among insurance claimants [16]. Differing recruitment methods likely explain the differences, and our lower figures [29]. Borchgrevink et al., in an ED-based study, found that 27% of 426 patients had been on sick leave, while Karlsborg et al. reported a median absence from work of six days (0 days–9 months) [30,31]. Those two studies also included short-term sick leave of less than two weeks, making direct comparison with our figures difficult. In an earlier study from our geographical area during 1990-1991, 7% of 255 patients were still on 100% sick leave after five years, compared with 3% in the present study [32]. In the previous study, however, only car occupants were included. Altogether, these results from our area correspond well to the 95% return to work rate shown by Athanasou et al. [15]. Furthermore, it should be emphasized that 86% of the injured persons did not have long-term sick leave, thus indicating a good prognosis from a sick leave perspective.
Risk factors for sick leave because of neck injury following traffic crashes have been studied but not enrolled in any systematic reviews. In one insurance company cohort, high age and concentration difficulties one-month post injury were significant risk factors for prolonged sick leave [16]. Another study reported that subjective cognitive symptoms and decreased range of motion at baseline were significant risk factors for sick leave three years post injury [33]. Miettinen et al. reported that being male or single had a protective effect and in a study of neck and back pain in general, female sex and advanced age were risk factors for disability pension but not sick leave [34,35]. Fort et al. studied predictors for not being able to return to work after traffic-crashes in general and found that having pressed charges, pain at six months, and physical sequelae at six months were independent predictors [36]. The present study´s finding that high age is a risk factor for sick leave confirms some of the previous findings mentioned earlier. An interesting new finding was that vehicle-related injury events was a risk factor for long-term sick leave. Future studies of risk factors for sick leave following neck injuries will, hopefully, include various types of injury events thus providing a possibility to reproduce this result.
The total cost projected into the future for all whiplash injuries in Sweden 2001 (8 million inhabitants, 3.5 million cars) has been estimated at nearly 500 million Euros [19]. There are also significant costs on a personal level for a large proportion of the injured, Leth-Petersen et al. found that only half of whiplash claimants returned to the same earning level that they had prior to the injury [37]. The mean cost for productivity loss per person found in this study (10,400 Euros) can be compared with a study from Sweden showing that whiplash injuries give rise to an approximate eight days average increase in the number of sick days from the year prior to the whiplash injury to the year after the injury [17]. This translates to a cost of about 950 Euros per case the first year after the injury (calculation based on the same method as in the present study). Two reasons can mainly explain the tenfold difference between Joud´s and our results: 1. Sick leave for other reasons was accounted for in Joud’s study; if that had been done in the present study the cost would decrease by up to 30%; 2. A five-year follow up adds a much higher number of sick days than a one-year follow up. In another large register based case-control study, Jennum et al. found that direct (health care) and indirect costs (loss of productivity) was 1,242 Euro per patient the year prior to a whiplash injury and 2,559 Euros the year after, a difference of 1,317 Euros [18]. The costs should be related to costs of preventive measures such as more effective head restraints and restraint systems in cars, and to other injury mitigation measures. Even though the youngest patients were seldom granted long-term sick leave, some were. For young people, a whiplash injury might become a personal disaster, as well as a costly incident for the society and insurance system.
Studies of neck injuries in persons of all ages, including traffic and non-traffic injury events as well as neck injuries of all severities (WAD 1-4), are rare. Because this study has this wide inclusion, it gives a complete picture of all neck injuries treated at the ED of a middle-sized Swedish city. These injuries and the consequent long-term sick leave are described with good validity given the circumstances that the population in the area has well-known demographics, only one medical facility takes care of this type of acute emergencies, the injury registration is stable and reliable, and the social insurance system is compulsory. In 97% of all cases in age group 18-64 we have clear-cut independent documentation of their long-term sick leave 2001-2006. However, because our incidence figures are based on ED-visits, they may not cover all neck injuries in society. ED-cohorts are naturally biased towards severe and moderate cases; there are likely a number of cases with mild strains and sprains, especially following non-traffic injury events that are not attended to by the ED. However, because the inhabitants in the area traditionally seek medical care at the hospital’s ED and because the GP on-call is located at the hospital, the results seem to be appropriate for giving a representative and conservative picture of neck injuries in need of medical attention in the area. Umeå is a city with a low mean age (university city) and may have a disproportionate number of injured bicyclists compared to cities with other demographics. In this study, the whole population in age group 18-64 was considered to be at risk for sick leave. Because some persons at baseline benefit from disability pension and because some are institutionalized, the true population at risk is lower. We could not control for this in our material. The logistic regressions conducted to determine risk factors for long-term sick leave had a poor goodness of fit suggesting that the models do not fit the data very well. It´s also important to emphasize that some of the previously known important risk factors for poor outcome, such as pain intensity and education [38] were not included in the analysis. The somewhat odd finding that WAD grade 1 was a significant risk factor for long-term sick leave has to be interpreted with caution. A systematic review and meta-analysis of risk factors for persistent problems following whiplash injuries came to the opposite conclusion [38]. The fact that the WAD-grades were set in retrospect may have biased the results and the number of patients included in the analysis was small. The cost of lost productivity calculated from sick leave ≥15 days is only a part of the total cost of neck injuries following whiplash trauma and should not be considered to reflect the full spectrum of costs to the individual and to society. However, given that the number of inpatient days was very low in the present study (indicating a low health care cost), and given that adding the first 14 days of sick leave would not have increased the total sick years by more than a few years; the calculation of the cost of lost productivity still gives a good estimate of the total costs to society from these injuries.
As stated previously, the incidence of whiplash injuries from traffic crashes is believed to be >300/100,000/year [1]. The present study highlights that other injury mechanisms also give rise to neck injuries after whiplash-like movements. Two main questions for future studies arise from these facts: 1. What is the true incidence of neck injuries following whiplash trauma in society? 2. What is a non-traffic whiplash trauma, how should it be defined, and are the injury mechanisms similar to those of traffic crashes or not? A large population based study aiming at reaching cases of all severities including cases not seen in hospitals is needed to answer question 1. Such a prospective study should also include follow up at different points to determine the natural history of the condition including sick absence. Notably, falls caused no cases of long-term sick leave in our study – maybe indicating a low trauma-energy and maybe indicating that falls do not cause psychological trauma to the same extent as traffic-crashes. Experimental studies of neck kinematics in falls would be helpful to partly explain this issue and to answer question 2. Future studies on sick leave should try to answer the question; why some people are granted sick leave and some not, and if sick leave can be used to enhance the rehabilitation process.
In conclusion, neck injuries following whiplash trauma arise from both traffic and non-traffic injury events and affect people of all ages. Consequent long-term sick leave occurs in a minority of the patients; commonly among older persons and persons injured in traffic. Because of the high incidence, the small share of patients who are sick absent for very long periods of time will contribute to a high cost to society for lost productivity.
Acknowledgements
This work was supported by a grant from the department of research and development, Västernorrland County Council. The authors wish to thank the staff of The Swedish Social Insurance Agency in Umeå for their assistance in providing data on sick leave. We also wish to thank Gabriel Granåsen for assisting in the statistical analysis.
References
- Holm LW, Carroll LJ, Cassidy JD, Hogg-Johnson S, Côté P, et al. (2009) The Burden and Determinants of Neck Pain in Whiplash-Associated Disorders After Traffic Collisions. J Manipulative PhysiolTher 32: S61–69.
- Styrke J, Stålnacke B-M, Bylund P-O, Sojka P, Björnstig U (2012) A 10-Year Incidence of Acute Whiplash Injuries After Road Traffic Crashes in a Defined Population in Northern Sweden. PM&R 4: 739–747.
- Quinlan KP, Annest JL, Myers B, Ryan G, Hill H (2004) Neck strains and sprains among motor vehicle occupants-United States, 2000. Accid Anal Prev 36: 21–27.
- Versteegen GJ, Kingma J, Meijler WJ, Duis ten HJ. (1998) Neck sprain in patients injured in car accidents: a retrospective study covering the period 1970-1994. Eur Spine J 7: 195–200.
- Versteegen GJ, Kingma J, Meijler WJ, Duis ten HJ. (1998) Neck sprain not arising from car accidents: a retrospective study covering 25 years. Eur Spine J 7: 201–205.
- Martin JL, Perez K, Mari-Dell'Olmo M, Chiron M (2008) Whiplash risk estimation based on linked hospital-police road crash data from France and Spain. InjPrev 14: 185–190.
- Association of British Insurers. (2008) Tackling Whiplash, Prevention, Care, Compensation.
- Cassidy JD, Carroll LJ, Cote P, Lemstra M, Berglund A, et al. (2000) Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med 342: 1179–1186.
- Björnstig U, Hildingsson C, Toolanen G (1990) Soft-tissue injury of the neck in a hospital based material. Scand J Soc Med. 18: 263–267.
- Bring G, Björnstig U, Westman G (1996) Gender patterns in minor head and neck injuries: an analysis of casualty register data. Accid Anal Prev 28: 359–369.
- Hildingsson C, Toolanen G (1990) Outcome after soft-tissue injury of the cervical spine. A prospective study of 93 car-accident victims. ActaOrthopScand 61: 357–359.
- Crutebo S, Nilsson C, Skillgate E, Holm LW (2010) The Course of Symptoms for Whiplash-Associated Disorders in Sweden: 6-Month Followup Study. J Rheumatol 37: 1527–1533.
- Carroll LJ, Holm LW, Hogg-Johnson S, Côté P, Cassidy JD, et al. (2009) Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative PhysiolTher 32(2 Suppl): S97–107.
- Stovner LJ (1996) The nosologic status of the whiplash syndrome: a critical review based on a methodological approach. Spine 21: 2735–2746.
- Athanasou JA (2005) Return to Work Following Whiplash and Back Injury: a Review and Evaluation. Med Leg J 73: 29–33.
- Buitenhuis J, de Jong PJ, Jaspers JPC, Groothoff JW (2009) Work disability after whiplash: a prospective cohort study. Spine 34: 262–267.
- Joud A, Stjerna J, Malmstrom EM, Westergren H, Petersson IF, et al. (2013) Healthcare consultation and sick leave before and after neck injury: a cohort study with matched population-based references. BMJ Open 3: e003172.
- Jennum P,Kjellberg J, Ibsen R, Bendix T (2013) Health, Social, and Economic Consequences of Neck Injuries. Spine 38: 449–457.
- Chappuis G, SoltermannB (2008) Number and cost of claims linked to minor cervical trauma in Europe: results from the comparative study by CEA, AREDOC and CEREDOC. Eur Spine J 17: 1350–1357.
- World Health Organisation (WHO) (2010) International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) version 2010
- Spitzer WO, Skovron ML, Salmi LR, Cassidy, JD, Duranceau J, et al. (1995) Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining “whiplash†and its management. Spine 20(8 Suppl): 1S–73S.
- Committee on Injury Scaling. (1998) The Abbreviated Injury Scale, 1998 revision. Association for the Advancement of Automotive Medicine, Des Plaines, IL.
- Radetzki M (2004) [Total costs for whiplash injuries in Sweden]. 1–28.
- Agresti A. (2002) Categorical Data Analysis. (2ndedn), Wiley-Interscience, New Jersey.
- Sterner Y, Toolanen G, Gerdle B, Hildingsson C (2003) The incidence of whiplash trauma and the effects of different factors on recovery. J Spinal Disord Tech 16: 195–199.
- Versteegen GJ, Kingma J, Meijler WJ, Duis ten HJ (2000) Neck sprain after motor vehicle accidents in drivers and passengers. Eur Spine J 9: 547–552.
- Mayou R, Bryant B (1996) Outcome of 'whiplash' neck injury. Injury. 27: 617–623.
- Nijs J, Inghelbrecht E, Daenen L, Hachimi-Idrissi S, Hens L, et al. (2011) Recruitment bias in chronic pain research: whiplash as a model. ClinRheumatol 30: 1481–1489.
- Borchgrevink GE, Lereim I, Røyneland L, Bjørndal A, Haraldseth O. (1996) National health insurance consumption and chronic symptoms following mild neck sprain injuries in car collisions. Scand J Soc Med 24: 264–271.
- Karlsborg M, Smed A, Jespersen H, Stephensen S, Cortsen M, et al. (1997) A prospective study of 39 patients with whiplash injury. ActaNeurolScand 95: 65–72.
- Bylund PO, Björnstig U (1998) Sick leave and disability pension among passenger car occupants injured in urban traffic. Spine 23: 1023–1028.
- Borenstein P, Rosenfeld M, Gunnarsson R (2009) Cognitive symptoms, cervical range of motion and pain as prognostic factors after whiplash trauma. ActaNeurolScand 122: 278–285.
- Miettinen T, Airaksinen O, Lindgren K-A, Leino E (2004) Whiplash injuries in Finland--the possibility of some sociodemographic and psychosocial factors to predict the outcome after one year. DisabilRehabil. 26: 1367–1372.
- Hansson T, Jensen I (2004) Swedish Council on Technology Assessment in Health Care (SBU). Chapter 6. Sickness absence due to back and neck disorders. Scand J Public Health Suppl 63: 109–151.
- Fort E, Bouffard E, Charnay P, Bernard M, Boisson D, et al. (2011) Return to work following road accidents: Factors associated with late work resumption. J Rehabil Med 43: 283–291.
- Leth-Petersen S, Rotger GP (2009) Long-term labour-market performance of whiplash claimants. J Health Econ 28: 996–1011.
- Walton DM, MacDermid JC, Giorgianni AA, Mascarenhas JC, West SC, et al. (2013) Risk Factors for Persistent Problems Following Acute Whiplash Injury: Update of a Systematic Review and Meta-analysis. J Orthop Sports PhysTher. 43: 31–43.
Citation: Styrke J, Stålnacke BM, Per-Olof Bylund RN, Sojka P, Björnstig U (2014) Neck Injury after Whiplash Trauma in a Defined Population in Northern Sweden – Long-Term Sick Leave and Costs of Low Productivity. Epidemiology (Sunnyvale) 4:170. DOI: 10.4172/2161-1165.1000170
Copyright: © 2014 Styrke J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15811
- [From(publication date): 9-2014 - Aug 23, 2025]
- Breakdown by view type
- HTML page views: 11199
- PDF downloads: 4612