Observing Digital Cardiac Rehabilitation using myHeart During the First Wave of COVID-19: A Real-World Multicentre Evaluation
Received: 14-Apr-2023 / Manuscript No. jcpr-23-95955 / Editor assigned: 17-Apr-2023 / PreQC No. jcpr-23-95955 (PQ) / Reviewed: 01-May-2023 / QC No. jcpr-23-95955 / Revised: 08-May-2023 / Manuscript No. jcpr-23-95955 (R) / Published Date: 15-May-2023 DOI: 10.4172/jcpr.1000193
Abstract
Objective: COVID-19 significantly impacted cardiac rehabilitation (CR) delivery. Service disruption left numerous patients without treatment access. Many healthcare teams made use of digital apps to support CR delivery and patients remotely. This evaluation aimed to analyse digital CR access from the myHeart interactive, cloud-based self-management app during the pandemic.
Methods: Five NHS secondary care CR services agreed to combine existing anonymised app data between Mar-Oct 2020 for 12-weeks to align as much as possible with traditional CR models.
Descriptive quantitative analyses of in-app CR education and exercise video access were performed. App usage feedback questionnaire were provided for clinicians and patient users.
Results: N=350/434(80.6%) patients activated myHeart. No statistically significant differences were observed across age groups (P=.332) or gender (P=.881) between users who activated myHeart and those who did not.
N=314/350(89.7%) users accessed 5,469 CR videos with N=313/314(99.7%) accessing 3,606 within the first 6-weeks of activation. No statistically significant differences were observed across gender (P=.978) or age group (P=.274) for education video views. Users with angina only diagnosis accessed more exercise videos than other reported diagnoses (P=.030). Patient user feedback responses showed a statistically significant increase in selfmanagement confidence following myHeart access (P=<.001).
Conclusion: Since COVID-19, digital health has advanced considerably and its benefits are becoming increasingly acknowledged. myHeart provided remote timely CR during service disruption. This evaluation is the beginning of a journey to understand app usage however further research is needed to fully understand the role digital health can play in the delivery of CR.
Keywords
Cardiac rehabilitation; Digital application (app); COVID- 19; Remote monitoring; Self-management; Digital health; Mobile health; Patient education
Introduction
Cardiovascular disease remains a leading cause of death worldwide, and accounts for more than a quarter of all UK deaths [1]. Following a cardiac event, intervention, or diagnosis patients are routinely offered a comprehensive cardiac rehabilitation (CR) Programme [2]. This complex treatment is aimed at promoting a healthy lifestyle through education and exercise, and supporting long-term management of heart health [3-5].
Despite CR being an essential and evidenced part of recovery, the service remains under delivered. The 2019 National Audit of Cardiac Rehabilitation (NACR) reported that 50% of those eligible did not receive CR in 2017/2018[6]. Reasons are multifactorial and include low referral rates, non-attendance at traditional centre-based classes as a result of distance and timing of classes, patient specific factors such as gender, ethnicity, age, socioeconomic status, illness perception, perceived need, and self-efficacy [4,7-11]. Suggested alternatives to improve participation include home-based programmes or digital solutions. It is also considered these alternatives, aimed at providing greater access to CR, will contribute to the 2028 National Health Service (NHS) goal of providing CR to 85% of those eligible [12-15].
Digital health
Digital health interventions were introduced into healthcare in support of increasing accessibility, albeit adopted slowly [16]. However, the emergence of COVID-19 expedited its implementation dramatically in order to reach patients remotely. The pandemic added emphasis to an already apparent need to redesign healthcare delivery. Related service disruption during the first outbreak caused CR participation to fall by 30-40% in the UK compared with 2019 [13,17-19]. Healthcare teams had to reduce avoidable exposure to patients, yet still provide the service [20]. Digital health offered an immediate solution to the delivery of CR in these challenging circumstances [21].
Recent studies exploring the impact of digital health have shown it can improve health outcomes for those with long-term conditions, including mental health, diabetes, cardiac and respiratory disease [22,23]. Since the pandemic, NHS Digital reports an increase in NHS application (app) registrations of 111% [24]. However, evidence is limited as to how users engage with an app for CR, or whether they are more likely to access CR when provided digitally.
This evaluation of retrospective data aimed to analyse digital CR access from the myHeart self-management app as a standalone method of CR delivery during the pandemic.
Methods
myHeart
myHeart is a cloud-based interactive digital self-management application (app) and is widely used within the NHS. All patiententered data and activity can be viewed and tracked by clinicians to support remote patient monitoring, subsequently providing data for clinical management, clinical audit, service evaluation, and research. myHeart offers CR videos, incorporating the British Association for Cardiovascular Prevention and Rehabilitation (BACPR) Standards [25] to provide clear guidance on exercise, education and lifestyle to support self-management. myHeart CR education and exercise content can be seen in the Supplementary. There are 45 different CR education videos ranging from 56 seconds to 5.49 minutes each. At first access the videos are locked meaning users must view each video consecutively, they remain unlocked once viewed. The CR exercise videos are gated and time restricted based on cardiac event and diagnosis. There are different levels of exercise program conducted either by standing or sitting, all of which contain a warm up, conditioning and cool down structure. Before commencing any exercise users must read and agree to the health and safety checklist. Prior to the pandemic, each participating NHS site had previously incorporated myHeart into service delivery as an additional tool to support centre-based and home-based CR.
App Users
Five NHS CR sites in Scotland, the Northeast and Southwest of England sought to explore myHeart access following the first wave of COVID-19 as part of a service evaluation. Individual site app usage reports were provided and thereafter all sites agreed to combine anonymised app data for analysis to explore myHeart CR use.
As part of CR at each site, myHeart had been implemented into usual practice to support service delivery prior to this evaluation. In keeping with usual care, adults over 18 years referred for CR were assessed for app suitability. This included having access to an internet connected device such as a mobile phone, a basic understanding of technology, and willingness to use myHeart.
Retrospective anonymised myHeart data, entered between March 2020 and October 2020, was evaluated for each user. Twelve weeks of app data was captured to align as much as possible with the traditional in-person CR length of 8 to 12 weeks (2-hour session, once a week) depending on site. Those patients who did not fully complete the app enrolment process were categorized as failed to activate.
The healthcare team’s contacted users to assess health status and provide app support either by telephone, or sending in-app notifications for those who had activated using the myHeart clinician dashboard. Short, bespoke questionnaires were provided to both clinicians and patients to obtain feedback on app experience, with emphasis on selfmanagement confidence.
Evaluation outcomes
The primary outcome was to quantify access of in-app CR exercise and education videos. Secondary outcomes included uptake to the app (activation), clinical contact to provide live support, and demographic characteristics of users including smoking. Bespoke voluntary anonymised feedback questionnaires, based on the NHS Friends and Family Test, were offered to both patient and clinical users to assess ease of use, the apps ability to provide a remote CR option, and whether patient users felt supported to confidently self-manage their health.
Data handling and Statistical analysis
Users who had fully activated the app across all five sites were included in the analysis. Descriptive quantitative analyses were conducted using IBM SPSS V26. App retention was evaluated for 12-weeks (84 days) since app activation using Kaplan-Meier plots. For this, an event was defined as the day a participant last recorded an activity within the 12-weeks evaluated. Participants with app activity on the 84th day were censored instead. To evaluate statistical evidence of differences in retention between app reported demographics, a logrank test was used.
Activity in the app was described for all enrolled patients across the 12 weeks by the total number of different days the app was accessed during this time. As all data was positively skewed, analysis was conducted using median and interquartile range (IQR). For comparisons of app activity between app reported demographics, age was categorized into 5 groups (≤33, 34-48, 49-64, 65-78, ≥79 years) [26]. Comparisons of CR access according to diagnosis used the first reported diagnosis only. Hypothesis testing of continuous activity data were analysed using Kruskal Wallis (27). Alpha was set at 0.05 for all hypothesis tests.
Ethics statement
This evaluation of existing app data did not require Institutional Review Board approval as it did not include any personally identifiable information, there was no comparable standard treatment arm, no randomisation allocation, and myHeart is a digital tool currently in use within all participating sites where patients have the option to use it or not [27]. All data collected for this evaluation was anonymised at the point of user registration as per the app’s security processes. At activation users must agree to the apps terms and conditions of use and privacy policy before obtaining app access which includes the sharing of anonymised data for research and evaluation purposes. Each of the participating NHS CR sites agreed to share anonymised app data for this analysis. The anonymised feedback questionnaires were optional and offered to both clinician and patient app users by their respective CR team.
Data Availability
All data analysed during this study are included in this article.
Results
Sample characteristics
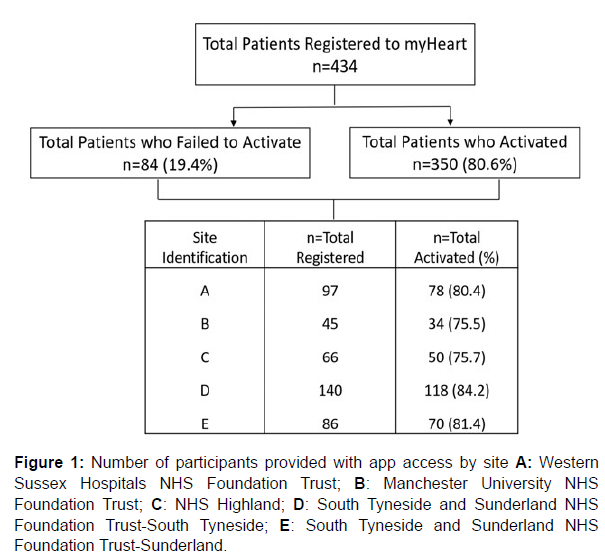
A total of 434 patients were registered to myHeart, of which 350 (80.6%) activated the app (Figure 1).
Figure 1: Number of participants provided with app access by site A: Western Sussex Hospitals NHS Foundation Trust; B: Manchester University NHS Foundation Trust; C: NHS Highland; D: South Tyneside and Sunderland NHS Foundation Trust-South Tyneside; E: South Tyneside and Sunderland NHS Foundation Trust-Sunderland.
The mean app recorded age for those who activated was 62.4 years (SD 11.8). A total of 255 (72.9%) users recorded their gender, 186 males and 69 females. There were no statistically significant differences between those who activated the app (N=350) and those that did not (N=84) in age (mean 62.6 years, SD 13.79), P=.332, or gender (where reported N=255, P=.881). A cardiac diagnosis was reported by 251 (71.7%) users. The age of those reporting a Myocardial Infarction was 59.3 (SD 11.7) years, Heart Failure 61.4 (SD 12.4) years, and Angina, 62.3 (SD 12.2) years. Of the 251 who reported a cardiac diagnosis there were 40 (15.9%) who reported more than one. Smoking status was reported by 116 (33.1%) users. Demographic data for all myHeart users is shown in (Table 1).
| Site | Total (n=350) | |||||
|---|---|---|---|---|---|---|
| Characteristic | A | B | C | D | E | |
| Gender, n (%) | ||||||
| Male | 34 (43) | 18 (53) | 26 (52) | 65 (55) | 43 (62) | 186 (53) |
| Female | 16 (21) | 6 (18) | 14 (28) | 21 (18) | 12 (17) | 69 (20) |
| Not Reported | 28 (36) | 10 (29) | 10 (20) | 32 (27) | 15 (21) | 95 (27) |
| Age, mean (SD) | 63.3 (11.9) | 63.5 (8.5) | 61.1 (11.5) | 62.2 (13.3) | 62.3 (10.6) | 62.4 (12) |
| Smoking Status, n (%) | ||||||
| Non-smoker | 9 (12) | 5 (15) | 11 (22) | 19 (16) | 12 (17) | 56 (16) |
| Ex-smoker | 18 (23) | 4 (12) | 6 (12) | 17 (14) | 9 (13) | 54 (15) |
| Current | 1 (1) | 0 | 0 | 3 (3) | 2 (3) | 6 (2) |
| Not Reported | 50 (64) | 25 (73) | 33 (66) | 79 (67) | 47 (67) | 234 (67) |
| Diagnosis Type*, n | ||||||
| Angina | 16 | 5 | 10 | 13 | 21 | 65 |
| Myocardial Infarction | 39 | 18 | 26 | 45 | 30 | 158 |
| Heart Failure | 8 | 3 | 9 | 43 | 5 | 68 |
| *Some users recorded a combination of diagnoses | ||||||
Table 1: App reported demographics for patients who activated myHeart at each site A: Western Sussex Hospitals NHS Foundation Trust; B: Manchester University NHS Foundation Trust; C: NHS Highland; D: South Tyneside and Sunderland NHS Foundation Trust-South Tyneside; E: South Tyneside and Sunderland NHS Foundation Trust-Sunderland.
The 350 activated users accessed myHeart a median 3 (IQR 2-7) different days, with the median time between first and last day of app access being 17 (IQR 2– 46) days. The median number of events recorded by a patient was 5 (IQR 1 - 17). The overall median times the app was accessed was 12 (IQR 1-47) times.
Primary outcome
A total of 5,469 CR videos were viewed by 314 (89.7%) users.
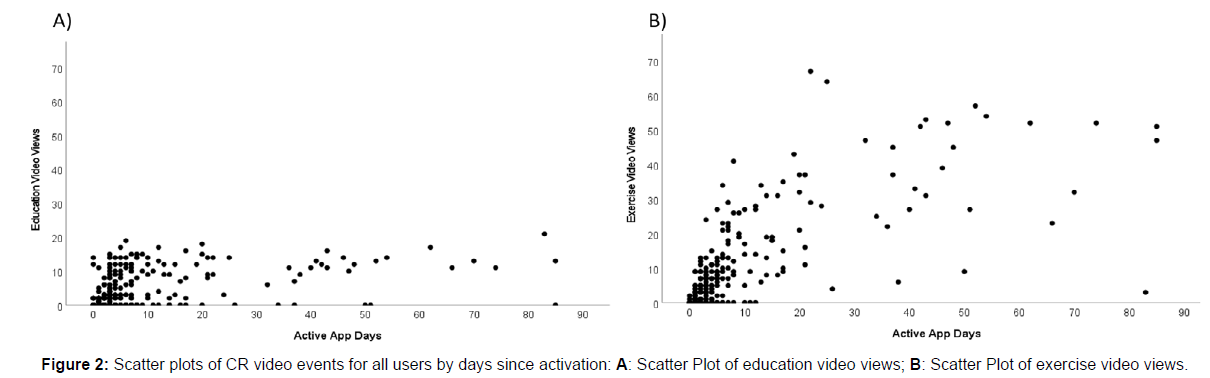
Education videos were accessed a median 6 (IQR1-7, range 1 to 20) times and exercise videos a median 9 (IQR 1-18, range 1 to 66) times (Figure 2). Within the first 6 weeks following activation 313 (99.7%) users viewed 3,606 CR videos.
Video activity for CR education and exercise were compared between app reported demographics. There was no statistically significant gender differences observed for education video views. On averages, males viewed a median 0 (IQR 0-8, 95%CI 2.80-4.31) and females a median 0 (IQR 0-6, 95%CI 2.26-4.67) P=.978. Furthermore, no statistically significant difference was observed between gender and exercise video views with males accessing a median 0 (IQR 0-10, 95%CI 6.01-9.98), and females a median 3 (IQR 0-9, 95%CI 5.42-11.45) P=.342.
Users in the <33 year age group viewed more CR education videos than those in any other age group (mean 9.0, SD 8.1, 95%CI 11.41- 28.75). Those in the 34-48 year age group viewed the least education videos a mean 2.8 (SD 5.37, 95%CI 0.95-4.70) with a mean difference of 6.2. However, this was not statistically significant, P=.274.
A comparison between different reported first diagnoses showed those with an Angina only diagnosis viewed more CR educational videos (median 14.5, IQR 40, 95%CI 2.99-7.13) than any other diagnosis, though not statistically significant (P=.054). Those with an Angina only diagnosis also accessed more exercise videos (median 16, IQR 4-17, 95%CI 0.27-0.29) than any other diagnoses which was statistically significant (P=.030).
Users who reported a non-smoking status viewed more CR education videos (median 6.5, IQR 3-14, 95%CI 5.43-8.92) than both ex (median 0.5, IQR 0-9) and current smokers (median 3.5, IQR 1-11) which showed a statistically significant difference of p=0.032. Comparisons between smoking status and exercise video views showed no statistically significant difference, P=.055.
Clinical support
The CR healthcare teams provided ongoing clinical support remotely to assess patient health status and any app usage concerns using the myHeart clinician dashboard, enabling them to observe patient CR activity within the app. Contact was made either by telephone or using in-app notifications for those who had activated. Of the 434 patients offered myHeart, clinicians made contact with 237 (54.6%), attempts were made for the remaining 197 (45.6%). On average patients were contacted a mean 2.7 (SD 2.1, range 0 to 20) times and sent in-app notifications a mean 6.2 (SD 3.1, range 1 to 8) times during their respective 12-week CR Programme. Of those who did not complete app activation, contact was made with 31 patients via telephone 2.3 (SD 1.8, mean difference 3.9, range 0 to 20) times. This was significantly lower than those who had activated (P=.007).
User experience
Both clinicians and app users were invited to answer anonymised myHeart user questionnaires. From the 350 patient users 55 (15.7%) responded to one or more of the questions. This response rate is in keeping with the Health Survey for England Feasibility Study (HSE FS) and HSE 2019 response rates [28]. There was a statistically significant difference observed between before and after having access to the app in terms of an increase in self-management confidence. Analysis showed that n=18/50 (36%) reported they had more confidence after having access to the app, P=<.001 (95%CI 0.23-0.57).
Twenty five clinicians were also asked to provide feedback on the app's functionality and suitability for service delivery, of which 20 (80%) responded. (Figure 3) shows the questionnaire results for both clinicians and patient users.
Discussion
This evaluation has shown positive uptake of a digital health intervention, myHeart, and provided an insight into its advantages despite the unprecedented circumstances. myHeart provided patients with access to CR and supported clinicians to remotely monitor patients during COVID-19. These results suggest myHeart is a feasible enhancement to standard CR that can provide support to patients outside of the hospital environment and encourage a shared-care approach during rehabilitation.
Of the patients offered myHeart in the pandemic, 80.6% activated the app, with 89.7% of these accessing in-app CR videos within the study period of their first 12 weeks of use. Online platforms and digital apps offer many benefits including overcoming attendance barriers caused by distance and asynchronous delivery of content enabling those with work or caring commitments to engage [29]. Not only can they potentially improve uptake by engaging hard to reach populations, there is evidence that home-based exercise is more sustainable than in-centre delivery in terms of long-term behaviour change [30-32]. Uptake to myHeart showed an acceptance rate of >80% across 3/5 sites, and over 75% across all sites, suggesting it is possible to supplement traditional CR with digital health. An enhanced, or hybrid, model incorporating digital health may not only provide patients with additional information but support autonomous self-management.
Furthermore, despite a small number of users responding to the feedback the overall functionality of the app was perceived as beneficial. Regardless of the abrupt implementation of myHeart as a total replacement for CR during the pandemic, both patients and clinicians used it. In keeping with other apps there was a fall in continuous activity over subsequent weeks [33] though this may be due to patients using the app solely for CR. It is also possible that some users have obtained the necessary information in a lesser timeframe thereafter accessing it sporadically when needed [34]. The flexibility of myHeart means it can be used for multiple purposes and clinical teams should consider guiding patients towards the desired usage, be it for CR or monitoring specific clinical data remotely. More research is necessary to fully understand effective engagement with digital health and CR.
This patient cohort was younger than the average cardiac patient [35,36] suggesting a degree of selection bias. Despite this, younger patients appeared to be the higher activity users but there was no statistically significant difference in CR access across age groups. This is not surprising as previous evidence suggests older adults are less likely to use newer technology including the internet [37,38]. However, the proportion of technology enabled older patients has increased since the pandemic to support health and communication needs [39,40].
Gender disparity is widely evidenced in CR programmes, with women being reported as less likely to participate and more likely to drop-out [2,41-43]. Barriers to participation including demographic, socioeconomic, social and medical challenges impact both men and women, but particularly women [41]. Although not statistically significant less women did activate the myHeart app in this study. This highlights the importance for future studies to stratify recruitment to ensure gender difference can be properly compared. Providing digital health as an additional option for CR delivery offers flexibility, and incorporating it as an additional treatment option could promote increased participation in CR amongst women [44]. Further research is needed to explore differences in digital health activity between gender, age and other demographics to help better understand how to maximise app usage. Specific patient factors associated with higher usage of apps requires more research. The impact of the app on routine clinical practice, post pandemic, requires further investigation to understand its impact and benefits on CR delivery, clinical outcomes and cost effectiveness.
Strengths
This evaluation is the beginning of a journey to understand app usage for CR delivery. The use of myHeart under the pandemic circumstances has provided an insight into its capabilities and evidenced the appetite for digital health for both patients and clinical users. There was consistent use across all age groups, with the oldest participant being 87 years, and across gender suggesting that the results are generalisable to these demographics. Moreover, the apps functionality enabled the delivery of the Programme as a standalone option, despite it being designed as a supplementary tool to promote self-management and support conventional service delivery. Data was included from 5 NHS Sites to provide a generalised view across different trusts, which demonstrates this may work in many different regions and is an important consideration for future research.
Limitations
Limitations exist within this evaluation. It is likely that the uptake and persistence with myHeart was influenced by COVID-19 and subsequent service disruption, and therefore not a true reflection of digital health usage. National CR uptake figures were not validated due to staff redeployment as a result of the pandemic therefore it was not possible to compare uptake to the app versus the number referred for CR during this time [45]. Further research in the post-pandemic era is needed to provide greater understanding of digital health usage in CR delivery. Selection bias, particularly with regard to age, gender and user understanding may have played a part in app provision. As all data entered into the app was user reported missing data existed. Additionally, a number of outliers which may have exerted undue influence were present but remained in the analysis as considered to be a normal variation in this setting. Further research is required to determine the validity of outliers when using digital health. Clinical data was not collected therefore there was no way of knowing whether app access influenced health outcome measurements. This evaluation only measured 12-week of in-app data for each user therefore it is not known if or how many users have continued to use myHeart for selfmanagement purposes. Furthermore, missing data is likely to have influenced the analysis. Usage data for in-app clinically reported data, such as blood pressure, heart rate, weight and cholesterol were not included in the analysis as the focus was on CR delivered via myHeart, but these may be important where the app is being used by clinicians to remotely monitor clinical data.
Conclusion
The apps functionality provided digital CR as a standalone option during COVID-19 for both patients and healthcare professionals. Variable app activity highlights the importance of the clinician role in encouraging patients to use the app. Providing patients with this option as part of a structured pathway may contribute to increasing CR attendance rates. Further research to define optimal implementation strategies and show the clinical and health economic impact of myHeart in this setting would enhance understanding of the role digital therapeutics can play in the evolving delivery of healthcare.
Acknowledgments
With thanks to the 5 participating NHS cardiac rehabilitation teams.
Author contribution
• Alison Blythin first author with substantial contribution to conception and design of the work, analysis, and interpretation of data, drafting and revising for intellectual content, final approval for publication, accountable for all aspects of the work.
• Jack Elkes provided substantial contribution to the design of the work, analysis, interpretation of data, drafting and revising for intellectual content and final approval for publication.
• Dr Ronie Walters provided substantial contribution to the interpretation of data, drafting and revising for intellectual content.
• Amber Bhogal provided substantial contribution to the interpretation of data, drafting and revising for intellectual content.
• Ian Thompson substantial contribution to the design of the work.
• Thomas van Lindholm provided the data from the my mhealth Limited platform, and data validation and verification.
• Matt Smith provided the graphic illustrations used in the Supplemental material.
• Prof. Trish Gorely substantial contribution to the interpretation of data, drafting and revising for intellectual content.
• Prof. Tom Wilkinson substantial contribution to the interpretation of data, drafting and revising for intellectual content.
• Prof. Stephen Leslie provided clinical oversight, substantial contribution to the interpretation of data, drafting and revising for intellectual content and final approval for publication.
• Dr. Adam Kirk senior author provided clinical oversight, substantial contribution to conception and design of the work, analysis, and interpretation of data, drafting and revising for intellectual content, final approval for publication, accountable for all aspects of the work. Dr. Adam Kirk acts as guarantor accepting official responsibility for the integrity of the manuscript.
Competing Interests
Alison Blythin, Ian Thompson, Amber Bhogal, , Thomas van Lindholm, Matt Smith, Tom Wilkinson and Adam Kirk are employees of my mhealth Limited. Jack Elkes, Ronie Walters, Trish Gorely, Stephen Leslie have nothing to disclose. The Authors declare no Competing Financial or Non-Financial Interests.
Sponsor/Funding
This work was sponsored and funded by my mhealth Limited.
Patient & Public Involvement (PPI)
A PPI group was formed at myHeart app inception to review the app design, usability, and content. This is a continuous process with participants contributing to ongoing app development.
Publication
This analysis has been conducted for patients, users, healthcare professionals and the public. Results will be displayed on the my mhealth website and efforts will be made to ensure publication using open access. STROBE reporting guidelines have been used.
References
- British Heart Foundation (2019) Cardiac rehabilitation : the big picture.
- NACR (2018) The National Audit of Cardiac Rehabilitation Quality and Outcomes Report 2018.
- The National Institute for Health and Care Excellence (NICE) (2021) Acute coronary syndromes : secondary prevention and rehabilitation overview 1-6.
- Neubeck L, Freedman S Ben, Clark AM, Briffa T, Bauman A, et al. (2012) Participating in cardiac rehabilitation: A systematic review and meta-synthesis of qualitative data. Eur J Prev Cardiol 19: 494-503.
- British Heart Foundation (2019) Cardiac Rehabilitation.
- Blake I (2019) Half of heart patients miss out on life-saving recovery care. British Heart Foundation.
- Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, et al. (2002) Barriers to Participation in and Adherence to Cardiac Rehabilitation Programs: A Critical Literature Review. Prog Cardiovasc Nurs 17: 8-17.
- Foster EJ, Munoz S-A, Crabtree D, Leslie SJ, Gorely T (2021) Barriers and facilitators to participating in cardiac rehabilitation and physical activity in a remote and rural population; a cross-sectional survey. Cardiol J 28: 697-706.
- De Angelis C, Bunker S, Schoo A (2008) Exploring the barriers and enablers to attendance at rural cardiac rehabilitation programs. Aust J Rural Health 16: 137-142.
- Shanmugasegaram S, Oh P, Reid RD, McCumber T, Grace SL (2013) Cardiac rehabilitation barriers by rurality and socioeconomic status: A cross-sectional study. Int J Equity Health 12: 72.
- Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, et al. (2004) Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technol Assess 8: 1-152.
- Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, et al. (2015) Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol 22: 35-74.
- Dalal HM, Doherty P, McDonagh STJ, Paul K, Taylor RS (2021) Virtual and in-person cardiac rehabilitation. BMJ 373: n1270.
- National Guideline Centre (UK) (2018) Chronic Heart Failure in Adults: Diagnosis and Management.
- https://www.longtermplan.nhs.uk/online-version/chapter-3-further-progress-on-care-quality-and-outcomes/better-care-for-major-health-conditions/cardiovascular-disease/
- Cohen AB, Martin SS (2020) Innovation without integration. NPJ Digit Med 3: 15.
- Fersia O, Bryant S, Nicholson R, McMeeken K, Brown C, et al. (2020) The impact of the COVID-19 pandemic on cardiology services. Open Hear 7: e001359.
- NHS England (2020) Cardiovascular Disease. NHS Long Term Plan.
- Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, et al. (2020) COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 396: 381-389.
- Hoeksma J (2020) NHS Providers report highlights digital transformation during Covid-19. Digital Health.
- O’Doherty AF, Humphreys H, Dawkes S, Cowie A, Hinton S, et al. (2021) How has technology been used to deliver cardiac rehabilitation during the COVID-19 pandemic? An international cross-sectional survey of healthcare professionals conducted by the BACPR. BMJ Open 11: e046051.
- Crooks MG, Elkes J, Storrar W, Roy K, North M, et al. (2020) Evidence generation for the clinical impact of myCOPD in patients with mild, moderate and newly diagnosed COPD: a randomised controlled trial. ERJ Open Res 6: 00460-2020.
- North M, Bourne S, Green B, Chauhan AJ, Brown T, et al. (2020) A randomised controlled feasibility trial of E-health application supported care vs usual care after exacerbation of COPD: the RESCUE trial. npj Digit Med 3: 145.
- Poinasamy K (2022) Useful Digital Health Apps and Platforms. BLF and Asthma UK.
- British Association for Cardiovascular Prevention and Rehabilitation (2017) The BACPR Standards and Core Competencies for Cardiovascular Disease Prevention and Rehabilitation. Br Assoc Cardiovasc Prev Rehabil 2017: 1-32.
- Reijneveld SA (2003) Age in epidemiological analysis. J Epidemiol Community Health 57: 397.
- William H. Kruskal & W. Allen Wallis (1952) Use of Ranks in One-Criterion Variance Analysis. J Am Stat Assoc 47: 583-621.
- Health Research Authority (2017) Service evaluation or Research.
- https://digital.nhs.uk/data-and-information/areas-of-interest/public-health/health-survey-for-england---health-social-care-and-lifestyles/feasibility-study-2020---2021/survey-response
- Nabutovsky I, Nachshon A, Klempfner R, Shapiro Y, Tesler R (2020) Digital Cardiac Rehabilitation Programs: The Future of Patient-Centred Medicine. Telemed J E Health 26: 34-41.
- Munro J, Angus N, Leslie SJ (2013) Patient focused internet-based approaches to cardiovascular rehabilitation - a systematic review. J Telemed Telecare 19: 347-353.
- Blair J, Angus NJ, Lauder WJ, Atherton L, Evans J, et al. (2014) The influence of non-modifiable illness perceptions on attendance at cardiac rehabilitation. Eur J Cardiovasc Nurs 13: 55-62.
- Blair J, Corrigall H, Angus NJ, Thompson DR, Leslie S (2011) Home versus hospital-based cardiac rehabilitation: A systematic review. Rural Remote Health 11: 1532.
- Birnbaum F, Lewis D, Rosen RK, Ranney ML ( 2015) Patient engagement and the design of digital health. Acad Emerg Med 22: 754-756.
- Ainsworth B, Steele M, Stuart B, Joseph J, Miller S, et al. (2017) Using an Analysis of Behavior Change to Inform Effective Digital Intervention Design: How Did the PRIMIT Website Change Hand Hygiene Behavior Across 8993 Users?. Ann Behav Med 51: 423-431.
- Crimmins EM, Hayward MD, Ueda H, Saito Y, Kim JK (2008) Life with and without heart disease among women and men over 50. J Women Aging 20: 5-19.
- Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, et al. (2019) Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis 6: 19.
- Opinium Research (2018) Data-Powered Health
- Gandiya T, Dua A, King G, Mazzocco T, Hussain A, et al. (2012) Self-reported “communication technology” usage in patients attending a cardiology outpatient clinic in a remote regional hospital. Telemed J E Health 18: 219-224.
- Sixsmith A, Horst BR, Simeonov D, Mihailidis A (2022) Older People’s Use of Digital Technology During the COVID-19 Pandemic. Bull Sci Technol Soc 42: 19-24.
- Tabassum N (2020) How are older people adapting to digital technology during the COVID-19 pandemic. Centre for Ageing Better.
- Forsyth F, Deaton C (2021) Women and cardiac rehabilitation: Moving beyond barriers to solutions?. Eur J Prev Cardiol 28: 758-760.
- Supervía M, Medina-Inojosa JR, Yeung C, Lopez-Jimenez F, Squires RW, et al. (2017) Cardiac Rehabilitation for Women: A Systematic Review of Barriers and Solutions. Mayo Clin Proc 92: 565-577.
- Mamataz T, Ghisi GLM, Pakosh M, Grace SL (2021) Nature, availability, and utilization of women-focused cardiac rehabilitation: a systematic review. BMC Cardiovasc Disord 21: 1-20.
- Knapton M (2007) The National Audit of Cardiac Rehabilitation Annual Statistical Report 2007. British Heart Foundation 1-40.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Blythin AM, Elkes J, Walters R, Bhogal A, Thompson I, et al. (2023) Observing Digital Cardiac Rehabilitation using myHeart During the First Wave of COVID-19: A Real-World Multicentre Evaluation. J Card Pulm Rehabi 7: 193. DOI: 10.4172/jcpr.1000193
Copyright: © 2023 Blythin AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3959
- [From(publication date): 0-2023 - Dec 14, 2025]
- Breakdown by view type
- HTML page views: 3436
- PDF downloads: 523