Research Article Open Access
Our Clinical Experience on Uterine Artery Embolization for the Treatment of Uterine Fibroids: A Retrospective Case-Series of 32 Patients
Isil Yildiz*Department of Radiology, Acibadem University Atakent Hospital, Istanbul, Turkey
- *Corresponding Author:
- Isil Yildiz
Department of Radiology, Acibadem University Atakent Hospital
Istanbul, Turkey
Tel: 905323560244
E-mail: drisilyildiz@gmail.com
Received date: July 11, 2017; Accepted date: July 31, 2017; Published date: August 04, 2017
Citation: Yildiz I (2017) Our Clinical Experience on Uterine Artery Embolization for the Treatment of Uterine Fibroids: A Retrospective Case-Series of 32 Patients. OMICS J Radiol 6:268. doi: 10.4172/2167-7964.1000268
Copyright: © 2017 Yildiz I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Purpose: To present our experience on uterine artery embolization performed in patients with uterine fibroids.
Materials and methods: Thirty-two patients (mean age, 37 years) with symptomatic fibroids who underwent uterine artery embolization in our clinic between July 2014 and May 2015 were retrospectively analyzed. Uterine and fibroid volumes were determined by T1-weighted MR images. The change in symptoms after procedure and the severity of postprocedural pain were assessed by patients.
Results: Median follow-up period was 23 months (range 21-30 months). None of patients had menorrhagia, 79% had less menstrual pain, and 82% had less or none abdominal bloating or swelling during follow-up. The mean volumes of uterus and largest fibroid decreased 55% and 66% after embolization, respectively. The rate of patients who satisfied with the procedure was 97%. Majority of women (81.3%) had severe pain which lasted for 4.0 ± 3.0 days. They returned to daily acitivities within 5.0 ± 1.1 days, and to work within 7.0 ± 2.1 days. None of patients had persisting discharge, permanent amenorrhoea, or infective complications.
Conclusion: Uterine artery embolization is an effective and safe treatment alternative for ymptomatic uterine fibroids provided that an extensive clinical and radiological evaluation is performed. Early postprocedural period can be painful, but pain resolves fast.
Keywords
Uterine fibroid; Artery embolization; Uterine artery
Introduction
Uterine fibroids (leiomyomata uteri) are the most common benign tumors of the uterus that present in more than half of women at the age of 40 and have a peak in the 5th decade [1,2]. Symptomatic fibroids can cause prolonged bleeding, bulk-related symptoms, pain and subfertility [3]. The standard treatment for symptomatic uterine fibroids is hysterectomy or myomectomy.
Arterial embolization is a technique for treatment of uterine fibroids which is used since 1990’s [4]. The studies showed that uterine artery embolization is an effective treatment against uterine fibroid symptoms in 80–94% of patients [5,6]. İt is known that all types of fibroids (submucosal, subserosal and intramural) recieves benefit from embolization [7]. It is a minimally invasive procedure with similar outcomes and lower rate of major complications compared to those of myomectomy [7,8]. The results of several comparative randomized studies suggested that uterine artery embolization should be considered as an option for women with symptomatic fibroids [3,7].
In this study we aimed to present our experience and 2-year follow-up data on uterine artery embolization performed in patients with uterine fibroids in our clinic. There are similar studies have been conducted but our result about menorrhagia is unique.
Materials and Methods
Study design and population
Thirty-eight consequtive patients with symptomatic fibroids who underwent uterine artery embolization in our clinic between July 2014 and May 2015 were retrospectively analyzed. Patients having one or more of fibroid symptoms, which are heavy menstruel bleeding; pelvic, back, flank or leg pain or pelvic pressure; and urinary frequency were included in the study. Exclusion criteria were gynecological cancer, pregnancy, perimenopause symptoms, pedunculated subserous leiomyomata and fibroids with a diameter longer than 12 cm. All of the patients were examined by gynecologists and besides digital pelvic examination, liqıid-based cytology and HPV DNA tests were done to screen for cervical precancerous lesions. Transvaginal ultrasonography was used to support digital pelvic examination to evaluate adnexial regions. Patients with an endometrial thickness above 5 mm and no suspicious submucosal fibroids that disturb endometrial intactness were further evaluated by endometrial sampling. Women with an endometrium thicker than 12 mm were sampled routinely. Six patients were excluded from the study according to the exclusion criteria. Four patients had complex endometrial hyperplasia, one had a pedunculated subserous fibroid of 8 cm diameter and the last one had a multiloculated heterogenous lesion in left adnexial region besides fibroids. Six patients excluded from the study according to the exclusion criteria. Thirty-two patients (mean age, 37 years; age range, 45-49 years) are included in the study.
The study was approved by the Institutional Ethics Commitee (2016/18-5, 10.11.2016), and all patient gave informed consent for the treatment.
Procedure of uterine arterial embolization
All patients were evaluated and followed up by gynecologists and an interventional radiologist (I.Y.) before the procedure. Initial clinical assesment included a pelvic examination and pap smear. Before the procedure, all patients had pelvic magnetic resonance T1-weighted (MR) imaging (1.5T Signa HD, GE Medical Systems, Milwaukee, Wisconsin, USA) and fast spin echo T2-weighted MR imaging (TR/ effectiveTE, 4250/120, matrix size 256×256, field of view 30 cm, section thickness 3 mm) after administration 10 ml of gadolinium. Necrosis is defined as absence of contrast enhancement on MRI. Dimensions for calculating the volume of the uterus, the largest (dominant) leiomyoma, and the position of the fibroids were obtained by the MR images. Formula for a prolate ellipse (L × W × D × 0.5233) was used to calculate the volumes. Dimensions used for calculations were measured on non-contrast T1-weighted images.
Foley catheter and an intravenous line were placed for the procedure. Intravenous cefazolin (1 g) or vancomycin (500 mg) was used for prophylaxis. Local anaesthesia was obtained by prilocaine. Midazolam was administered if necessary. Patients were well hydrated intravenously during and after the procedure. Right or left unilateral femoral artery access was used for the procedures. We didn’t use the radial access. Following a flush pelvic arteriogram, 5.0 F catheter (RIM catheter, Merit Medical Systems Inc., South Jordon, Utah, USA) was used to reach the origin of the uterine artery. Coaxially 2.9 F microcatheter (Embocath plus, Merit Medical Systems Inc., South Jordon, Utah, USA) was advanced into the uterine artery. The microcatheter tip was placed in the ascendant part of the uterine artery in order to avoid embolization of cervicovaginal branch [9]. No other catheter was used to reach the contralateral internal iliac and uterine artery. Trisacryl gelatin microspheres (500 to 900 μm size) (Embosphere, Merit Medical Systems Inc., South Jordon, Utah, USA) were used to embolize each uterine artery until the stasis occurred during 5 heart beats. All the uterine artery embolizations were performed by the same interventional radiologist (I.Y.).
Patients stayed one night at the hospital. Analgesia pump containing 50 mg morphine was used for pain control. Antiemetics were given if necessary.
Pain assessment
The severity of postprocedural pain was assessed by the patient either as ‘less than expected’ or ‘asexpected’ or ‘more than expected’. Additionally, a 6-point scoring system—less than period pain, like period pain, more than period pain, like labour pain, more than labour pain, worst pain ever felt—was used to evaluate pain intensity. The duration of pain was also noted.
Follow-up procedures
At 3, 6, 12, 18 and 24 months after embolization, follow-up MR images were obtained. During the follow-up, patients were also asked to describe their symptoms related to uterine fibroid by choosing one of the following options: improved, unchanged, worsened.
Statistical analysis
Statview 512 software (Abacus Concept, California, USA) was used for statistical analysis. Study data were summarized using descriptive statistics such as mean, standard deviation, median and range (minimum–maximum).
Results
All of the women had regular menstruation periods before the embolization. Menorrhagia and menstruel pain were the most common symptoms reported by 84.4% and 62.5% of patients, respectively (Table 1). Twenty-five patients (78%) had a history of anemia (hemoglobin <12.0 g/dL), for which one patient (3%) required blood transfusion. The number of symptoms per patient ranged between 1-3, which was 1.9 on average.
| Number of women who responded* | Number of patients with symptoms, n(%) | |
|---|---|---|
| Period symptoms | ||
| Heavy | 32 | 27 (100) |
| Painful | 32 | 20 (62.5) |
| Previous anaemia | 32 | 25 (78 ) |
| Previous blood transfusion | 32 | 1 (3.1) |
| Pressure symptoms | 32 | 11 (34.4) |
| Swelling/bloating | 32 | 12 (37.5) |
| Urinary symptoms | 32 | 3 (10) |
| Sciatica | 32 | 1 (3.1) |
Table 1: Summary of presenting symptoms. Values are given as n (%).
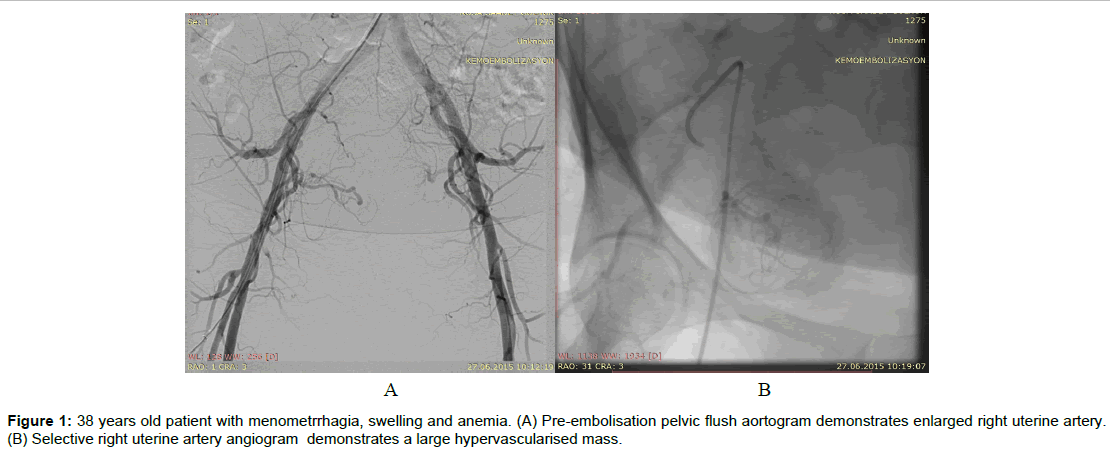
Selective uterine artery embolization was performed bilaterally in 31 patients (96.8%) (Figure 1) and unilaterally in one patient who had a history of pelvic surgery and a fibroid with the main blood supply from the right ovarian artery. All procedures were technically successful.
Outcome of uterine artery embolization
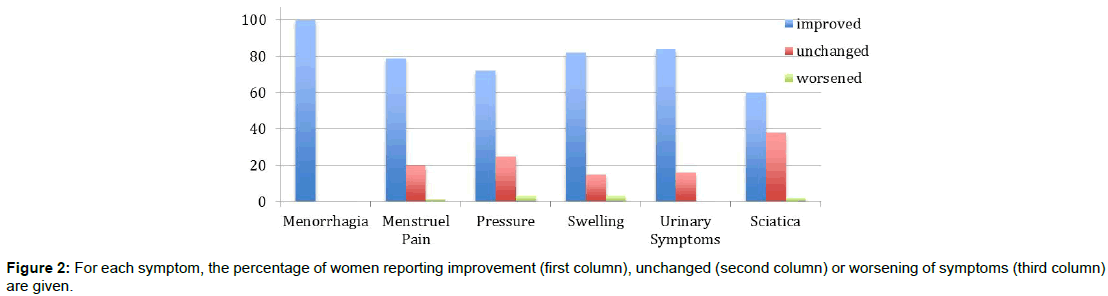
Median follow-up period was 23 months (range, 21-30 months). None of the women had menorrhagia, 79% had less menstrual pain, and 82% had less or none abdominal bloating or swelling during follow-up. During follow-up, one patient got pregnant and delivered by cesarean section at term. The rate of patients who satisfied with the procedure was 97% (Figure 2).
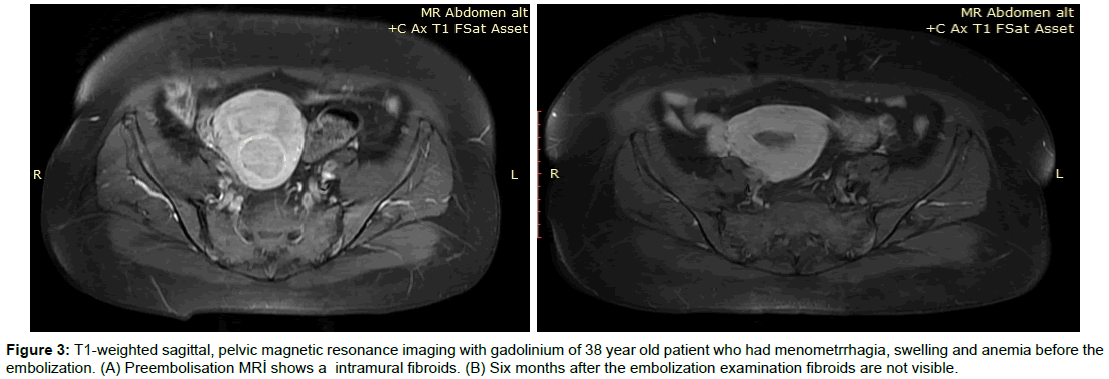
The uterine and fibroid volumes were calculated on follow-up MR imaging at an average of 23 months (range, 21–30 months) after the embolization (Figure 3). The mean volumes of the uterus and largest fibroid decreased 55% and 66% after embolization from 952 to 428 cc and 410 to 140 cc, respectively. The uterine and fibroid volumes before and after embolization were shown in Table 2. All of the patients included in the study had relief in at least one symptom and all of them had a decrease ine fibroid volume but we didn’t find any correlation between the symptom improvement and fibroid volume reduction.
| Magnetic resonance imaging | |||
|---|---|---|---|
| Number of patients | Volume (cc) | ||
| Mean [SD] | Median (range) | ||
| Before | |||
| Uterus | 32 | 952 [541] | 790 (240–2895) |
| Fibroid | 65 | 410 [530] | 280 (15–2400) |
| After | |||
| Uterus | 32 | 428 [272] | 426 (63–1265) |
| Fibroid | 65 | 140 [225] | 82 (0–890) |
Table 2: Magnetic resonance imaging based volumes of uterus and fibroids, baseline and for the follow up. Values are given as n, mean [SD] and median (range).
Figure 3: T1-weighted sagittal, pelvic magnetic resonance imaging with gadolinium of 38 year old patient who had menometrrhagia, swelling and anemia before the embolization. (A) Preembolisation MRİ shows a intramural fibroids. (B) Six months after the embolization examination fibroids are not visible.
Complications
Majority of women (81.3%) reported that they had greater pain after the procedure than they had during normal period. The postprocedural pain was worse than they expected for 17 patients (53%), better for 2 patients (6.4%), as expected for 13 patients (40.6). When the patients asked to describe their pain 0 (0%) told it was less than postprocedure pain, 3 (9.4%) told it was like period pain, 26 (81.3%) told it was more than period pain, 1 (3.1%) told it was more than labour pain, 1 (3.2%) told it was the worst pain ever. After the embolization, patients had pain for 4.0 ± 3.0 days (mean), 4 (1-9) days median. They returned to daily acitivities within 5.0 ± 1.1 days (mean), 6 (1-10)days (median), and got back to work within 7.0 ± 2.1 days (mean), 6 (1-15) days median.
Sixteen women (50%) had vaginal discharge after the embolization, which ended within two weeks in 9 patients, lasted 4-8 weeks in 4 patients, and continued longer than eight weeks in 3 patients. One patient had transient amenorrhea and 2 patients had irregular periods after embolisation. One patient had recurrent menorrhagic symptoms at 16 months and had myomectomy. None of the patients had persisting discharge, permanent amenorrhoea, or infective complications.
Discussion
In this retrospective case-series, we primarily found that uterine arterial embolization decreased uterine and fibroid volume more than half and provided significant improvement in clinical symptoms without causing significant complications.
Uterine artery embolization is a well-established and minimally invasive alternative to surgery for treatment of symptomatic uterine fibroids [3,7]. Preoperative clinical and radiological assessment of fibroid before the uterine artery embolization is very important. All patients being considered for uterine artery embolization must be evaluated both by the gynecologists and radiologists. Pelvic pathologies other than fibroids should be carefully evaluated for contraindications (e.g., malignancy). It is also important to evaluate present infections which may increase the complication risk of the embolization. MR imaging is modality which should be preferred before the embolization procedure for evaluation of the fibroid, uterus and concomitant patologies. It is known that coexisting adenomyosis in uterine fibroids is associated with poor response [10,11]. Excluding adenomyosis would increase the success of the arterial embolization targeting fibroids. On the other hand, uterine artery embolization is also a treatment alternative for adenomyosis. So prediagnosis of adenomyosis is important to plan the arterial embolization procedure. If adenomyosis diagnosed before the embolizaiton, it is not necessary to change treatment protocol. It is only important to know that if there is coexisting adenomyosis the treatment for fibroids may not be as successful as expected. In such a case it is important to inform the patient before the procedure.
The main purpose of the uterine arterial embolization for fibroids is elimination of the symptoms. Fibroid shrinkage is an additional advantage. In this study, we showed that there was a significant improvement in the clinical symptoms of fibroid after the uterine artery embolization. The procedure was well tolerated, and patients were highly satisfied with the procedure. First 24 hours after the procedure was mostly painful, but pain resolves fast so that most women can be back to work within 7 days. The end-point of embolization is also very important for reducing post-operative pain. Encouraging results following less extensive embolization have been presented [12]. The amount of the injected particles is reduced if spasm develops during the injection due to the stasis of the supervenes, which will cause to early termination of the procedure and insufficient embolization. Therefore, prevention of spasm by using microcatheters and slow injection has crucial importance. In order to prevent spasm, we performed very slow injection although it increases fluoroscopy time.
We also recorded a remarkable reduction in fibroid volumes. The measurements on MR imaging showed that uterus and fibroid shrunk by 55% and 66% at two years after embolization, respectively. Similarly, the mean decrease in fibroid size varies from 50-78% in the literature [5,13-15].
We had no infective complications in our series, probably because we excluded or treated pre-existing infection, since infection may lead hysterectomy after the embolisation particulary in subserous, large and pedunculated fibroids [13]. It is also important to be prepared for potentially fatal septic shock early after arterial embolization. If a patient has a temperature >38°C longer than four days and has an increase in pain, infection must be considered. Blood cultures, urine cultures and midstream, full blood count, and vaginal swabs should be evaluated. Pelvic MR imaging sould also be performed. Antibiotics should be administered as early as possible [16].
We had no patient with persisting vaginal discharge or ovarian failure in our study. However, ovarian failure has been reported in 2% of women under the age of 45 after uterine artery embolization [6,17]. Ovarian ischemia following embolization probably accounts for ovarian failure [17,18]. To prevent ovarian failure we used trisacryl gelatin microspheres with minimum size of 500 μm. It has also been reported that premature menopause may occur in 1-4% of women after the uterine artery embolization [17,19]. In some reports, amenorrhea rate reached to 12% over the age of 45 [20]. We had only one patient over the age 45 who didn’t have amenorrheoa after embolization.
There is no evidence that embolization is a cause of infertility. In many previous studies, women get pragnant and have successful deliveries after uterine artery embolization [5,6,21]. Uterine artery embolization or myomectomy was not found to be related with infertiliy [22-24]. In our series, there was one pregnancy with termdelivery.
In comparison to surgical treatment, uterine artery embolization leads to fewer complications and reduces hospital stay and treatment cost, but provides similar profiles of efficacy and quality of life [16,25]. On the basis of current literature data and our findings we suggest that uterine artery embolization is a good alternative for the treatment of fibroids. The effects of various clinical parameters such as pre-embolization size and shape of the fibroids, signal characteristics and contrast enhancement pattern of MR imaging on the response to the treatment have been studied in the previous reports without any significant conclusion [26-28]. In the present study, we have not evaluated clinical factors affecting the outcome of uterine artery embolization. Additionally, the limited sample size of our series and the retrospective design preclude us from reaching a definitive conclusion on clinical applicability of uterine artery emolization and its benefits and disadvantages over myomectomy in the treatment of uterine fibroids. Further comparative and large scale studies are needed to confirm the uterine artery embolization as a safe and effective treatment alternative for uterine fibroids, and to evaluate the predictive factors for the outcome of uterine artery embolization, so that we can determine the patients who can obtain the most benefit from the procedure.
Spies et al. reported results of 200 consecutive patients with a mean follow-up time 21 months [29]. Menorrhagia was improved in 87% and bulk symptoms were improved in 93% at 3 months. In our study none of the patients had menorrhagia. Bulk symptom control is similar in our study (82%). Spies et al. reported that at 1 year, 90% of patients still had symptom control. Twent-one (10.5%) patients had subsequent interventions or rehospitalizations. In our study 1 (3%) patient had susbsequent intervention and rehospitalized.
Walker and Pelage reported results of 400 patients with a 16.7 months follow-up time [30]. Menstrual bleeding was improved in 84% and menstrual pain improved in 79%. In our study menorrhagia was improved in all patients, menstrual pain improved 79%.
Pron et al. reported results of 550 patients from the Ontario Uterine Fibroid Embolization Trial [31,32]. In this study menorrhagia improved in 83%, menstrual pain improved in 77% [33]. None of the reported studies revealed %100 improvement in menorrhagia.
Conclusion
In conclusion, uterine artery embolization is an effective and safe alternative for the treatment of symptomatic uterine fibroids. An extensive clinical and radiological evaluation should be performed, and technical expertise should be sufficient to obtain the best outcome of the procedure.
References
- Wallach EE, Vlahos NF (2004) Uterine myomas: an overview of development, clinical features, and management. Obstet Gynecol 104: 393-406.
- Schwartz SM (2001) Epidemiology of uterine leiomyomata. Clin Obstet Gynecol 44: 316-326.
- Gupta JK, Sinha A, Lumsden MA, Hickey M (2006) Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database Syst Rev 26: CD005073.
- Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, et al. (1995) Arterial embolisation to treat uterine myomata. Lancet 346: 671-672.
- Marshburn PB, Matthews ML, Hurst BS (2006) Uterine artery embolization as a treatment option for uterine myomas. Obstet Gynecol Clin North Am 33: 125-144.
- Pelage JP, Le Dref O, Soyer P, Kardache M, Dahan H, et al. (2000) Fibroid-related menorrhagia: treatment with superselective embolization of the uterine arteries and midterm follow-up. Radiology 215: 428-431.
- Spies JB (2016) Current role of uterine artery embolization in the management of uterine fibroids. Clin Obstet Gynecol 59: 93-102.
- Martin J, Bhanot K, Athreya S (2013) Complications and reinterventions in uterine artery embolization for symptomatic uterine fibroids: a literature review and meta analysis. Cardiovasc Intervent Radiol 36: 395-402.
- Pelage JP, Le Dref O, Soyer P, Jacob D, Kardache M, et al. (1999) Arterial anatomy of the female genital tract: variations and relevance to transcatheter embolization of the uterus. Am J Roentgenol 172: 989-994.
- Smith SJ, Sewall LE, Handelsman A (1999) A clinical failure of uterine fibroid embolization due to adenomyosis. J Vasc Interv Radiol 10: 1171-1174.
- Siskin GP, Tublin ME, Stainken BF, Dowling K, Dolen EG (2001) Uterine artery embolization for the treatment of adenomyosis: clinical response and evaluation with MR imaging. AJR 177: 297-302.
- Spies JB, Benenati JE, Worthington-Kirsch RL, Pelage JP (2001) Initial US experience using trisacryl gelatin microspheres for uterine artery embolization for leiomyomata. J Vasc Interv Radiol 12: 1059-1063.
- Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG (2000) A prospective population-based study of menopausal symptoms. Obstet Gynecol 96: 351-358.
- Spies JB, Roth AR, Gonsalves SM, Murphy-Skrzyniarz KM (2001) Ovarian function after uterine artery embolization for leiomyomata: assessment with use of serum follicle stimulating hormone assay. J Vasc Interv Radiol 12: 437-442.
- Kim MD, Lee HS, Lee MH, Kim HJ, Cho JH, et al. (2010) Long-term results of symptomatic fibroids treated with uterine artery embolization: in conjunction with MR evaluation. Eur J Radiol 73: 339-344.
- Subramanian S, Spies JB (2001) Uterine artery embolization for leiomyomata: resource use and cost estimation. J Vasc Interv Radiol 12: 571-574.
- Baber R, Abdalla H, Studd J (1991) The premature menopause. Prog Obstet Gynaecol 9: 209-226.
- Siddle N, Sarrel P, Whitehead M (1987) The effect of hysterectomy on the age at ovarian failure: identification of a subgroup of women with premature loss of ovarian function and literature review. Fertil Steril 47: 94-100.
- Cassou B, Derriennic F, Monfort C, Dell'Accio P, Touranchet A (1997) Risk factors of early menopause in two generations of gainfully employed French women. Maturitas 26: 165-174.
- Chrisman HB, Saker MB, Ryu RK, Nemcek AA, Gerbie MV, et al. (2000) The impact of uterine fibroid embolization on resumption of menses and ovarian function. J Vasc Interv Radiol 11: 699-670.
- Ravina JH, Ciraru-Vigneron N, Aymard A, Le Dref O, Merland JJ (2000) Pregnancy after embolization of uterine myoma: report of 12 cases. Fertil Steril 73:1241-1243.
- Bulman JC, Ascher SM, Spies JB (2012) Current concepts in uterine fibroid embolization. Radiographics 32: 1735-1750.
- McLucas B, Goodwin S, Adler L, Rappaport A, Reed R, et al. (2001) Pregnancy following uterine artery embolization. Int J Gyn Obstet 74: 1-7.
- Sterling KM, Siskin GP, Ponturo MM, Rholl KS, Cooper JM (2002) A multi-center study evaluating the use of Gelfoam only for uterine artery embolization for symptomatic leiomyomata. J Vasc Interv Radiol 13: S19.
- Goodwin SC, Bradley LD, Steward EA, Nosher JL, Sterling KM, et al. (2006) Uterine artery embolisation versus myomectomy: a multicenter comparative study. Fertil Steril 85: 14-21.
- Kirby JM, Burrows D, Haider E, Maizlin Z, Midia M (2011) Utility of MRI before and after uterine fibroid embolization: why to do it and what to look for. Cardiovasc Intervent Radiol 34: 705-716.
- McLucas B, Adler L, Perella R (1999) Predictive factors for success in uterine fibroid embolization. Min Invas Ther Allied Technol 8: 429-432.
- Watson GMT, Walker WJ (2002) Uterine artery embolisation for the treatment of symptomatic fibroids in 114 women: reduction in size of the fibroids and women's view of the success of treatment. Br J Obstet Gynaecol 109: 129-135.
- Spies JB, Ascher SA, Roth AR, Kim J, Levy EB, et al. (2001) Uterine artery embolization for leiomyomata. Obstet Gynecol 98: 29-34.
- Walker WJ, Pelage JP (2002) Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG 109: 1262-1272.
- Pron G, Bennett J, Common A, Wall J, Asch M, et al. (2003) The Ontario uterine fibroid embolization collaboration group. the ontario uterine fibroid embolization trial. Part uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids. Fertil Steril 79: 120-127.
- James BS (2013) Current evidence on uterine embolization for fibroids. Semin Inter Radiol 30: 340-346.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 3910
- [From(publication date):
August-2017 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 3035
- PDF downloads : 875