Research Article Open Access
Pain Management in Mesothelioma
MacLeod N1,2*, Klepstad P3,4, Fallon M1,5 and Laird B1,2,51Edinburgh Cancer Research UK Centre, University of Edinburgh, Crewe Road South, Edinburgh EH4 2XR, UK
2Beatson West of Scotland Cancer Centre, 1053 Great Western Rd, Glasgow, G12, UK
3Department of Anaesthesiology and Emergency Medicine, St Olavs University Hospital, Trondheim N-7006, Norway, UK
4Department of Circulation and Medical Imaging, Norwegian University of Science and Technology (NTNU), 7006 Trondheim, Norway, UK
5Western General Hospital, Crewe Road South Edinburgh, EH4 2XU, UK
- Corresponding Author:
- MacLeod Nicholas
Edinburgh Cancer Research UK Centre
University of Edinburgh, Crewe Road South
Edinburgh EH4 2XR, UK
Tel: 0044 141 301 7679
Fax: 0044 141 301 7604
E-mail: Nicholas.macleod@ggc.scot.nhs.uk
Received Date: June 26, 2014, Accepted Date: July 01, 2015, Published Date: July 04, 2015
Citation: MacLeod N, Klepstad P, Fallon M, Laird B (2015) Pain Management in Mesothelioma . J Palliat Care Med 5: 223. doi: 10.4172/2165-7386.1000223
Copyright: © 2015 Macleod N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Pain is the most common symptom in malignant pleural mesothelioma and can be challenging to manage. This article discusses the pathophysiology of pain in mesothelioma, then, through a case history, outlines management options including medication, radiotherapy, chemotherapy and cordotomy.
Keywords
Pain; Malignant; Pleural; Mesothelioma
Introduction
Malignant pleural mesothelioma (MPM) is a rare cancer that originates from mesothelial cells, usually in the pleural lining of the chest. It is typically caused by exposure to asbestos and is traditionally associated with a long latency period, often in the region of 30-40 years [1]. The incidence is expected to peak in the next few years given the widespread use of asbestos in the second half of the last century. Unfortunately, there is no known cure for MPM and so the focus of management is often palliation of symptoms.
Pain is the most common symptom in MPM although fatigue and breathlessness are also highly prevalent [2]. In MPM, pain usually affects the chest in keeping with the underlying disease. However the cause of chest pain in MPM is multifactorial. Pain may be due to direct tumour infiltration of ribs, nerve roots, intercostal nerves, chest wall or, in some cases, due to the tumour invading the neurovascular bundle. In addition, in patients who undergo surgery, post thoracotomy pain is common [3]. The pain associated with MPM is often more severe and difficult to treat than pain caused by lung cancer [4].
The pathophysiology of pain in MPM is generally a mixture of bone and neuropathic pain. Therefore, managing this pain can be notoriously difficult with multiple analgesics, which target different pain mechanisms often being required. Unfortunately, patients may continue to suffer from severe pain despite multiple analgesics and so other options to consider for these patients include palliative radiotherapy, chemotherapy, neuroaxial pain therapy, and cordotomy. All these therapeutic options are discussed herein.
The difficulties of pain management in MPM are perhaps best illustrated via a case history.
Case History
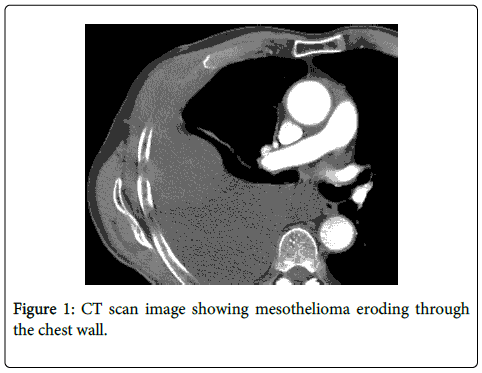
A 68-year-old man presented to his local hospital with severe right-sided chest pain and breathlessness. He had worked as an apprentice carpenter in the shipbuilding industry many years ago. A chest X-ray was performed which showed a right-sided pleural effusion and pleural thickening. A Computerised Tomograph (CT) (Figure 1) scan, including a CT guided biopsy, was done with pathology confirming MPM of sarcomatoid type. Treatment options were discussed with the patient. Chemotherapy was discussed but this was declined by the patient due to low likelihood of benefit. The patient agreed that treatment would be symptomatic only. The gentleman described his pain as “stabbing and shooting”, suggesting a neuropathic component. He also stated that it was severe in intensity.
Prior to admission, he had been taking tramadol (400 mg daily) and gabapentin (300 mg three times daily). During his admission, he was commenced on 40 mg of Morphine Sustained Release Tablets (every 12 hours), 15 mg of Immediate release Morphine Tablets when needed for pain, and a lidocaine patch applied over the chest wall. Tramadol was discontinued.
Pain continued to be problematic and when his morphine dose was escalated, he developed signs of opioid toxicity (muscle jerks and pseudo-hallucinations). He was therefore switched to Oxycodone Sustained Release Tablets (30 mg twice daily). With this, his opioid toxicity improved though was still present. His gabapentin was increased to 600 mg TDS and he remained on a lidocaine patch. Despite all this, his pain remained poorly controlled.
At this point, he received radiotherapy with the aim of improving his pain. Twenty Gy in 5 fractions of radiotherapy were administered which brought about a temporary improvement in his pain but six weeks after treatment, his pain was as severe as it was prior to his radiotherapy. Following this, he was considered for cordotomy but unfortunately died before he was able to receive this.
This case illustrates some of the difficulties patients with MPM face in terms of pain management. Despite multiple analgesics and palliative radiotherapy, his pain remained poorly controlled. Not all cases of MPM are as challenging as this.
Given that the pain associated with MPM is often multifactorial, patients are often on several drugs, which work via different mechanisms of action. It is always important to weigh up the potential benefits of multiple analgesics against the possibility of cumulative toxicity, drug interactions and patient compliance. Commonly used medications and doses are detailed in Table 1. The key components of analgesic treatment are detailed below.
| Drug Name | Type of Analgesic | Typical Starting Dose | Maximum daily dose |
|---|---|---|---|
| Paracetamol | Non Opioid | 1g QDS | 4g |
| Diclofenac | Non Opioid | 50mg TDS | 150mg |
| Codeine Phosphate | Weak Opioid | 30-60mg QDS | 240mg |
| Morphine | Strong Opioid | 10mg every 4-6 hours | No maximum dose |
| Oxycodone | Strong Opioid | 5mg every 4-6 hours | No maximum dose |
| Hydromorphone | Strong Opioid | 1.3mg every 4-6 hours | No maximum dose |
| Gabapentin | Adjuvant | 300mg OD | 3.6g |
| Pregabalin | Adjuvant | 75mg BD | 300mg |
| Amitriptyline | Adjuvant | 10mg OD | 150mg |
| Lidocaine | Adjuvant | 5% patch 12 hours on, 12 hours off | 5% patch 12 hours on, 12 hours off |
| Fentanyl | Strong Opioid | 12mcg per hour. Change every 72 hours | No maximum dose |
| Ketamine | Adjuvant | 5mg BD | No maximum dose |
Table 1: Drugs and dose ranges commonly used for pain management in MPM.
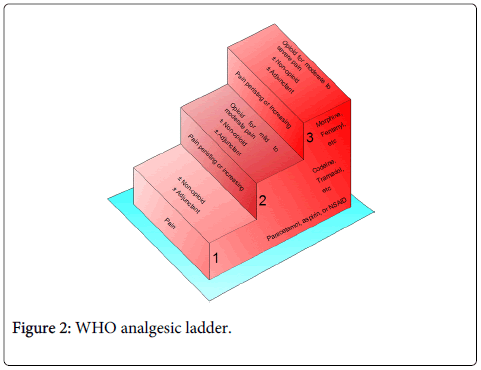
WHO analgesic ladder
The World Health Organisation’s (WHO) Analgesic Ladder for Cancer Pain Relief is recognised as the gold standard for treatment of cancer pain – see Figure 2 – and its principles has been continued in new guidelines [5,6]. It is easy to follow and can be applied to all types of pain, irrespective of aetiology. The first step on the ladder recommends using paracetamol or non-steroidal anti-inflammatories. If pain remains poorly controlled then patients should move on to step two, which involves the use of weak opioids such as codeine.
However, most patients with pain from MPM will quickly move to step three of the ladder which recommends strong opioids plus or minus non-opioids or adjuvant analgesics. Therefore, step two may be skipped and a step three opioid used as the first line opioid [6]. Morphine remains the most commonly used strong opioid though there are now a multitude of others available and often patients may try several different strong opioids in an attempt either to improve analgesic benefit/ reduce toxicity or both [6].
Opioids
Given the severity of pain associated with MPM, the majority of patients will require opioid analgesia with morphine being the most commonly used. It comes in both immediate and sustained release preparations, which are equivalent in terms of analgesic benefit [6,7]. Immediate release preparations are by many favoured for initial dose titration and subsequent breakthrough analgesia while sustained release preparations are more typically saved for long term use [8]. However, a direct titration using sustain released opioids is equally feasible [7]. Patients may require large quantities of opioids to help control their pain. It is not uncommon that, on these large doses, patients develop toxicity with symptoms such as somnolence, myoclonic jerks, cognitive impairment and hallucinations being prevalent. In these circumstances, most would favour a switch to another opioid such as oxycodone.
Adjuvant analgesics
Adjuvant analgesics are drugs whose main indication is not analgesia but they have analgesic properties. They are used in many types of pain including neuropathic pain. They can be used in combination with opioid analgesics or in isolation. However, in MPM, given the often severe intensity of pain, adjuvant analgesics are often used in combination with opioids [9]. Given that there appears to be a significant neuropathic component to the pain in MPM, it is not surprising that these drugs are commonly used in these patients. There are several different types of adjuvant analgesics which can be helpful.
Antidepressants
A Cochrane review summarises the evidence for the use of antidepressants in non-malignant neuropathic pain [10]. Tricyclic antidepressants are the most commonly used antidepressant in neuropathic pain. Amitriptyline has a marginally greater analgesic effect compared to other tricyclic antidepressants such as nortriptyline. Selective Noradrenaline reuptake inhibitors (SNRI) such as Duloxetine and venlafaxine may be of benefit in neuropathic pain, with duloxetine being favoured due to a better side effect profile [11].
Anticonvulsants
There is good evidence that anticonvulsants are effective in neuropathic pain [12]. Gabapentin has been used in the treatment of neuropathic pain for many years and is recommended as a first line treatment [13]. It is generally well tolerated though its dose limiting toxicity is usually somnolence. Pregabalin works in the same way as gabapentin and there is good evidence of its efficacy as an analgesic [14]. A recent prospective, placebo controlled, randomised controlled trial compared pregabalin with gabapentin and amitriptyline for neuropathic cancer pain. The results suggested that all drugs were effective in relieving cancer-related neuropathic pain but that pregabalin was associated with the greatest reduction in pain scores [15].
Other analgesics
Ketamine: There is some evidence supporting the benefit of ketamine in cancer pain [16]. If symptoms exist which are suggestive of central wind-up such as pain on light touch or increased pain to any painful stimulus then ketamine may be helpful. Furthermore, ketamine may renew opioid response when opioid doses are being increased with reduced response.
Topical analgesics: Topical analgesics can play a role in the treatment of pain in MPM with topical 5% lidocaine patches being the most commonly used. The main benefit of these patches is the lack of systemic side effects with local skin irritation being the common side effect. Though there have been no prospective studies in cancer patients, a retrospective review from Australia looked at 97 patients treated with lidocaine 5% patches and their results supported its use in post herpetic, post-surgical and cancer related neuropathic pain [17]. The high potency 8% capsaicin topical patch has proven efficacy in post herpetic neuralgia [18]. A single application of the patch for 30-60 minutes can result in pain relief for up to three months.
Radiotherapy
Many patients with MPM will continue to suffer from severe pain despite multiple analgesics. Therefore, radiotherapy is often considered for these patients. However, there is a dearth of evidence to support its use in any setting in MPM. Despite this, radiotherapy for pain relief is recommended in guidelines from the European Respiratory Society in collaboration with the European Society of Thoracic Surgeons [19].
Perhaps the most convincing evidence in favour of radiotherapy to help pain comes from a study where 22 patients with MPM and pain were treated with hemi thoracic irradiation at a dose of 30 gray in 10 fractions. Of the 19 patients assessable at three months, 13 had an improvement in their pain scores with no increase in their analgesic requirements though the median duration of response was only two months [20].
A recent study looked at palliative radiotherapy at a dose of 36 Grey in 12 fractions [21]. Radiotherapy was not given to the entire hemi thorax but instead was directed to the area that was felt to be causing the pain. This was because hemi-thoracic irradiation was felt to be too toxic. The study showed that pain improved in over 50% of patients two weeks after treatment though this was assessed via a retrospective review of case notes rather than prospectively. Interestingly, CT scans were performed in these patients two months after radiotherapy and a response rate of 43% was reported suggesting that, at an adequate dose, MPM may in fact be a radiosensitive disease.
Chemotherapy
Two phase III studies have shown a survival advantage in the region of two-three months for platinum/antifolate combination chemotherapy in MPM [22,23]. Quality of life data from one of these studies have been published [24]. These data showed that pain scores remained constant throughout treatment. The authors concluded that, in a rapidly fatal disease such as MPM, stabilization of pain was a positive finding. However, the same data can also be interpreted as showing that chemotherapy does not improve pain control in MPM. Therefore, chemotherapy should be prescribed in this disease in an attempt to improve survival rather than to improve pain. If symptom improvement is the aim then other treatment options should be considered.
Although chemotherapy can be offered, a retrospective review of MPM patients showed that, of 156 patients diagnosed, only 54 were deemed of adequate performance status to be offered chemotherapy and ultimately, only 27 patients received chemotherapy. Therefore, this treatment is not widely used in this population [25].
Epidural or intrathecal analgesia
Epidural or intrathecal treatment, usually with a combination of an opioid and a local anaesthetic, are alternative pain treatments for patients where other analgesics and radiotherapy fail to give pain relief. Local anaesthetics lessen the need for opioids and thereby minimize opioid induced adverse effects. Motor paralysis of the lower extremities, which is a frequent side effect related to intrathecal or epidural administration of local anaesthetics, is usually avoided for pains indicating that the neuroaxial catheter is inserted in the upper part of the thoracic column. Still, epidural or intrathecal pain therapies are invasive, are associated with a risk for infections, and need a very close follow-up [26].
Intra pleural analgesia which involves administering local anaethetics into the pleural space has been described and felt to be effective for some malignancies [27]. However, no data exist for this procedure in patients with MPM and, therefore, recommending such a treatment in this patient group is difficult.
Cordotomy
Despite all of the above interventions, many patients with MPM continue to suffer from severe pain. In these instances, there may be a role for percutaneous cervical cordotomy (PCC). This procedure interrupts the spinothalamic tracts at the level of C1/2 and causes loss of pain sensation contralaterally. Unfortunately, there are no prospective, randomised data on the role of cordotomy in MPM. The evidence comes from case series such as that by Jackson et al.3 They performed a retrospective review of 52 patients with MPM who underwent PCC. Their results showed that over 80% of patients were able to reduce their opioid requirements after the intervention and 38% stopped opioids completely. At nine weeks post PCC, 18 patients had a recurrence in their pain requiring an increase in analgesia. Mild weakness was noted in four patients and dysaesthesia was noted in two patients. The authors concluded that PCC had a low complication rate and was successful in treating pain associated with MPM.
A Turkish group reported on 165 patients who underwent PCC, 19 of whom had MPM [28]. Of these 19 MPM patients, 13 were followed up for a median of 5.9 months with six patients being lost to follow up. The only complication reported was one case of post cordotomy dysaesthesia and all patients had an improvement in pain after the procedure. They recommend that all patients with local pain due to MPM should be considered for PCC.
Conclusions
The pain associated with MPM is extremely challenging to manage. Patients will often require a multitude of analgesic drugs since opioids alone are often insufficient to control the pain. It is not uncommon for patients to be on paracetamol, anti inflammatories, opioids, adjuvant analgesics in addition to topical treatments. For some, this combination of drugs may provide adequate analgesia. However, many patients continue to suffer from pain despite this cocktail of drugs. In these patients, other options should be considered. Chemotherapy, while offering a potential survival advantage, does not appear to have a significant impact on pain. Radiotherapy may be of benefit in some patients though prospective randomised data is lacking. Finally, again, despite a lack of prospective randomised data, neuroaxial pain therapy or cordotomy should be considered for patients whose pain is refractory to other treatments.
References
- Davidson B (2008) New diagnostic and molecular characteristics of malignant mesothelioma. UltrastructPathol 32:227-240.
- Muers MF, Stephens RJ, Fisher P, Darlison L,Christopher MB Higgs, et al.(2008) Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial. Lancet 371:1685-1694.
- 3.Jackson MB, Pounder D, Price C, Matthews AW, Neville E (1999) Percutaneous cervical cordotomy for the control of pain in patients with pleural mesothelioma. Thorax 54:238-241.
- Jackson MB, Pounder D, Price C, Matthews AW, Neville E (1999) Percutaneous cervical cordotomy for the control of pain in patients with pleural mesothelioma. Thorax 54:238-241.
- Salminen EK, Silvoniemi M, Syrjänen K, Kaasa S, Kloke M, et al. (2013) Opioids in pain management of mesothelioma and lung cancer patients.ActaOncol52:30-37.
- Geneva W (1996) Cancer Pain Relief, World Health Organization.
- Caraceni A, Hanks G, Kaasa S. (2012) Use of opioid analgesics in the treatment of cancer pain: evidenced-based recommendation from the EAPC. Lancet Oncol 13:e58-68.
- Donnelly S, Davis MP, Walsh D, Naughton M; World Health Organization (2002) Morphine in cancer pain management: a practical guide. Support Care Cancer 10:13-35.
- Klepstad P, Kaasa S, Jystad Å, Hval B, Borchgrevink PC (2003) Immediate- or sustained-release morphine for dose-finding during start of morphine to cancer patients: a randomised, double-blind trial. Pain 101: 193-198.
- Gilron I, Bailey JM, Tu D, Holden RR, Weaver DF, et al. (2005) Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med 352:1324-1334.
- Saarto T, Wiffen PJ (2007) Antidepressants for neuropathic pain. Cochrane Database Syst Rev CD005454.
- Preskorn SH, Irwin HA (1982) Toxicity of tricyclic antidepressants--kinetics, mechanism, intervention: a review. J Clin Psychiatry 43:151-156.
- Backonja MM (2000) Anticonvulsants (antineuropathics) for neuropathic pain syndromes.Clin J Pain 16:S67-72
- Dworkin RH, O'Connor AB, Backonja M (2007) Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 132:237-251.
- FreynhagenR, Strojek K, Griesing T (2005) Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens. Pain 115:254-263.
- Mishra S, Bhatnagar S, Goyal GN, Rana SP, Upadhya SP (2012) A comparative efficacy of amitriptyline, gabapentin, and pregabalin in neuropathic cancer pain: a prospective randomized double-blind placebo-controlled study. Am J HospPalliat Care 29:177-182.
- Bell RF, Eccleston C, Kalso E (2003) Ketamine as adjuvant to opioids for cancer pain. A qualitative systematic review. J Pain Symptom Manage 26:867-875.
- Fleming JA, O'Connor BD (2009) Use of lidocaine patches for neuropathic pain in a comprehensive cancer centre. Pain Res Manag 14:381-388.
- Jones VM, Moore KA, Peterson DM (2011) Capsaicin 8% topical patch (Qutenza)--a review of the evidence. J Pain Palliat Care Pharmacother 25: 32-41.
- Scherpereel A, Astoul P, Baas P, Berghmans T, Clayson H, et al. (2010) Guidelines of the European Respiratory Society and the European Society of Thoracic Surgeons for the management of malignant pleural mesothelioma. EurRespir J 35:479-495.
- Bissett D, Macbeth FR, Cram I (1991) The role of palliative radiotherapy in malignant mesothelioma. ClinOncol (R CollRadiol) 3:315-317.
- Jenkins P, Milliner R, Salmon C (2011) Re-evaluating the role of palliative radiotherapy in malignant pleural mesothelioma. Eur J Cancer 47:2143-2149.
- van Meerbeeck JP, Gaafar R, Manegold C, Van Klaveren RJ, Van Marck EA, et al. (2005) Randomized phase III study of cisplatin with or without raltitrexed in patients with malignant pleural mesothelioma: an intergroup study of the European Organisation for Research and Treatment of Cancer Lung Cancer Group and the National Cancer Institute of Canada. J ClinOncol 23:6881-6889.
- Vogelzang NJ, Rusthoven JJ, Symanowski J, Denham C, Kaukel E, et al. (2003) Phase III study of pemetrexed in combination with cisplatin versus cisplatin alone in patients with malignant pleural mesothelioma. J ClinOncol 21: 2636-2644.
- Bottomley A, Gaafar R, Manegold C, Burgers S, Coens C, et al. (2006) Short-term treatment-related symptoms and quality of life: results from an international randomized phase III study of cisplatin with or without raltitrexed in patients with malignant pleural mesothelioma: an EORTC Lung-Cancer Group and National Cancer Institute, Canada, Intergroup Study. J ClinOncol 24: 1435-1442
- Chapman A, Mulrennan S, Ladd B, MuersMF (2008) Population based epidemiology and prognosis of mesothelioma in Leeds, UK. Thorax 63:435-439.
- Amesbury B, O'Riordan J, Dolin S (1999) The use of interpleural analgesia using bupivacaine for pain relief in advanced cancer. Palliat Med 13: 153-158.
- Kanpolat Y, Savas A, Ucar T (2002) CT-guided percutaneous selective cordotomy for treatment of intractable pain in patients with malignant pleural mesothelioma. ActaNeurochir (Wien) 144:595-599.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 17258
- [From(publication date):
July-2015 - Jun 15, 2025] - Breakdown by view type
- HTML page views : 12578
- PDF downloads : 4680