Peripheral Talus Fractures-A Clinical Observational Study of 16 Cases
Received: 05-Mar-2018 / Accepted Date: 27-Mar-2018 / Published Date: 03-Apr-2018 DOI: 10.4172/2329-910X.1000264
Abstract
Background: Peripheral talar fractures are rare injuries. They comprise fractures of the lateral process, the lateral and medial tubercle of the posterior process, the medio-caudal ridge, and traumatic osteochondral fractures of the lateral talar dome. The objective of this observational case series was to report the clinical and radiological outcome after surgical treatment.
Methods: 16 peripheral talar fractures could be included in this retrospective case series. All patients were treated operatively and followed for a minimum of 12 months. Clinical and radiological outcome were recorded.
Results: Mean follow-up was 16 months. 13 subjects presented with concomitant injuries. 2 patients suffered an additional spine fractures, and 4 patients were polytraumatized. No non-union or mal-union were observed. One patient needed subtalar and calcaneo-cuboidal fusion during follow up due to a concomitant calcaneal fracture. Other secondary procedures like implant removal were necessary in 5/16 subjects. During the last follow-up the recorded AOFAS score (mean ± SD) was 87.3 ± 6.6 and the EQ5-D (mean ± SD) 0.91 ± 0.06.
Conclusion: With early diagnosis and timely surgical treatment good results can be expected after peripheral fractures of the talus. Less favourable outcomes are usually associated with concomitant injuries.
Keywords: Talus fracture; Snowboarders ankle; Lateral talar process; Posterior talar process; Osteochondral fracture of the talus
Introduction
Peripheral talar fractures comprise fractures of the lateral and posterior process with its lateral and medial tubercle, the medial or medio-caudal ridge, the talar head as well as traumatic osteochondral lesions of the lateral and medial talar dome [1]. They are a heterogeneous entity of injuries in terms of mechanism, pathology, treatment and outcome. However, they share some common traits, for which reason they are analysed together: they are rare, easily overlooked, and show poor results if neglected [2].
Peripheral talar fractures are more common than central body fractures of the talus or talar neck fractures [1]. The incidence of peripheral talar fractures has traditionally been estimated with 0.3 to 1% of all ankle injuries [2,3]. However, a recent radiological evaluation of 132 talar fractures showed that 18% of all talar fractures involved the lateral process and 16% involved the posterior process [4]. Generally, peripheral fractures of the talus are regarded as less severe, since they are associated with less severe soft tissue injury and lower incidence of avascular necrosis [1,2,5]. Injury mechanisms remain controversial. Before snowboarding, fractures of the lateral process were seen after falls from height, as dorsiflexion-inversion injuries, and as high-velocity injuries. Today this fracture is also referred to as snowboarders’ ankle. Janes et al. were the first to describe this unusual fracture entity in 1990 [6]. Later the pathomechanism was explained as result from axial loading and sudden severe dorsiflexion with the hind foot in inversion, producing a shearing force transmitted from the calcaneus to the lateral process of the talus. Resent biomechanical studies, however, suggest that an external rotational component is an important momentum for lateral process fractures [7].
Two different injury mechanisms have been suggested for fractures of the lateral tubercle of the posterior process–also known as Shepherd’s fracture [8]: (1) forced hyper plantarflexion and inversion in some cases associated with medial subtalar dislocation [9,10] and (2) hyper dorsiflexion and inversion resulting in an avulsion of the posterior talofibular ligament [2].
Fractures of the medial tubercle of the posterior process – also known as Cedell’s fracture [11] are secondary to pronationdorsiflexion forces causing an avulsion of the insertion of the posterior deltoid ligament [12,13]. These injuries may be associated with subtalar dislocations [10]. Fractures of the talar head are less common. Hence it is difficult to define a clear fracture mechanism. They may be associated with dislocations of the Chopart’s joint (transverse tarsal joint) and other fractures of the talus [14]. Osteochondral fractures of the talus are associated with twisting injuries of the ankle. They may occur with or without associated ankle fracture or acute lateral instability. They have to be distinguished from osteochondral lesions due to repetitive trauma [15,16].
The standard diagnostics are conventional X-ray in dorso-plantar lateral and oblique projections. However, when suspected, e.g. with subtalar dislocation or adequate injury mechanism CT scans are mandatory. Standard secondary images reformations should include axial sagittal and coronal views. Moreover, 3D views (volume rendering technology, VRT) are helpful for analyzing the myriad fracture pathology and for planning surgical approaches [17]. Peripheral talus fractures are easily misdiagnosed using conventional x-rays and a high index of suspicion is necessary [2,18,19]. In a recent study the most common fracture missed by radiography was a compression fracture of the talar dome (31% not seen on radiography), followed by isolated lateral process (21%) and posterior tubercle (15%) fractures [4].
Non operative treatment is possible for non-displaced fractures and comprises cast immobilization for 6 weeks as well as limited weight bearing combined with physical therapy (lymphatic drainage, cooling, etc.). However, most authors advocate operative treatment for dislocated fractures – gaps or steps with more than 2 mm [1,2]. The primary aim is to reduce and fix the fracture. This, however, is not always easy. Depending on fragment size resection of the fragment may be the only choice. The same may also be necessary in multifragmentary situations. Surgical approaches depend on the exact location and configuration of the fracture. Arthroscopic and mini-open approaches have been suggested [1,2]. In selected cases osteotomies of the medial or lateral malleolus might be necessary.
The objective of this consecutive case series was to describe injury mechanisms, the diagnostic algorithm, surgical treatment and outcome of peripheral talus fractures in order to add some more information to the existing literature, which consists mainly of case reports and small cohorts.
Patients and Methods
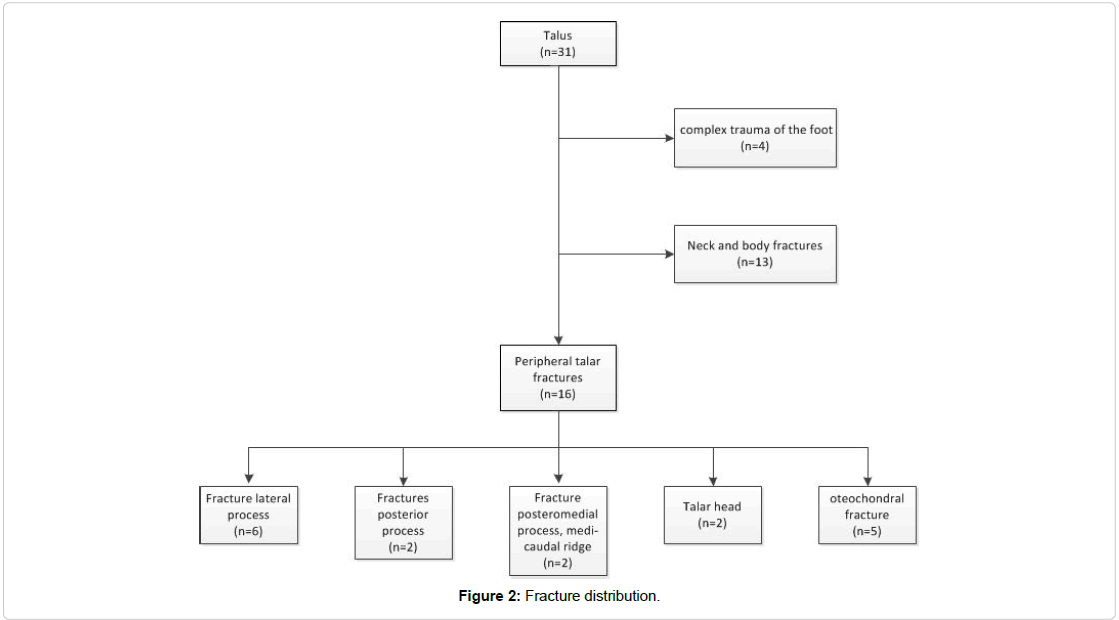
The hospital data base was searched for all acute fractures of the talus between 2010 and 2014. A total of thirty-one subjects could be identified. Patients with complex trauma of the foot, as defined by Zwipp (>5 points on the Zwipp scale) [20,21], talar neck and body fractures, as well as all patients with chronic osteochondral lesions due to repetitive trauma were excluded.
The institutional review board was informed about the study, formal consent, however, was not required.
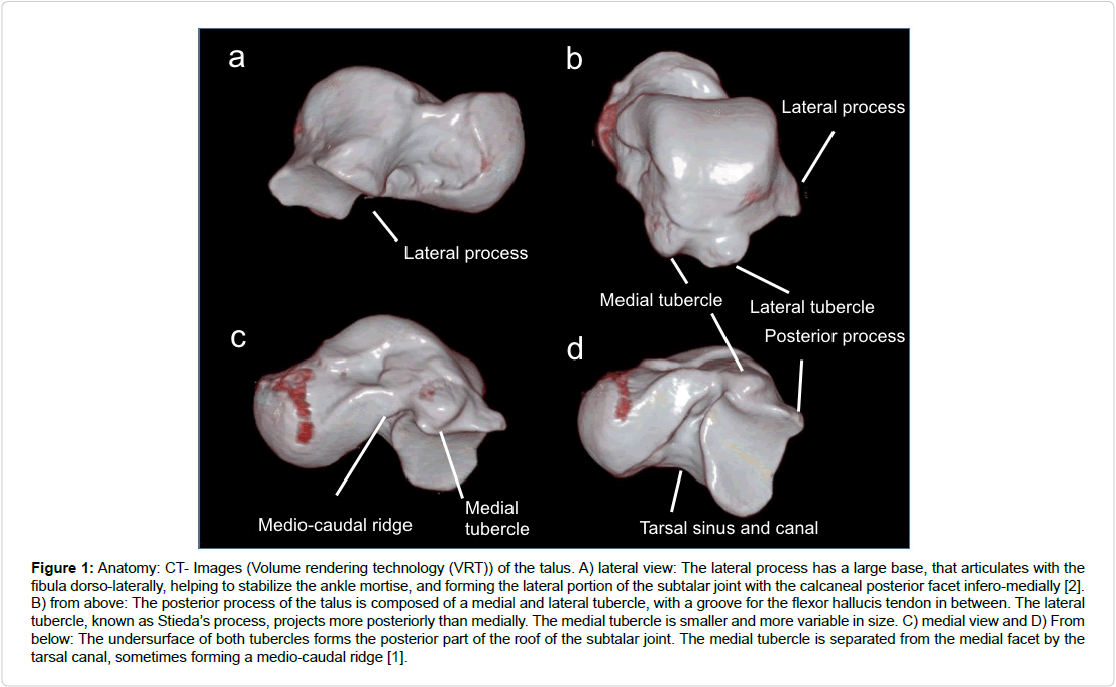
16 subjects with a peripheral fracture of the talus were included in the retrospective case series. Figure 1 displays talus anatomy and Figure 2 the distribution of the fractures.
Figure 1: Anatomy: CT- Images (Volume rendering technology (VRT)) of the talus. A) lateral view: The lateral process has a large base, that articulates with the fibula dorso-laterally, helping to stabilize the ankle mortise, and forming the lateral portion of the subtalar joint with the calcaneal posterior facet infero-medially [2]. B) from above: The posterior process of the talus is composed of a medial and lateral tubercle, with a groove for the flexor hallucis tendon in between. The lateral tubercle, known as Stieda’s process, projects more posteriorly than medially. The medial tubercle is smaller and more variable in size. C) medial view and D) From below: The undersurface of both tubercles forms the posterior part of the roof of the subtalar joint. The medial tubercle is separated from the medial facet by the tarsal canal, sometimes forming a medio-caudal ridge [1].
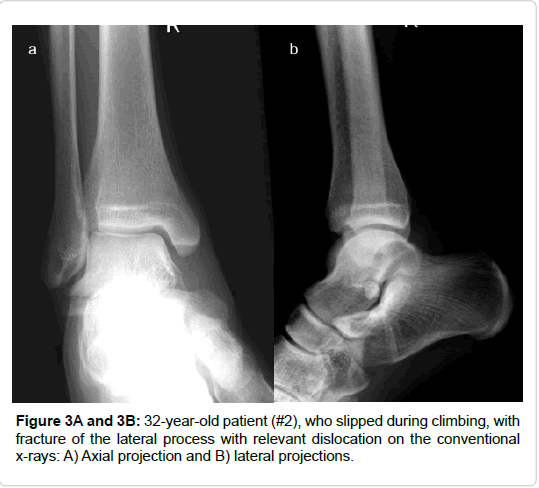
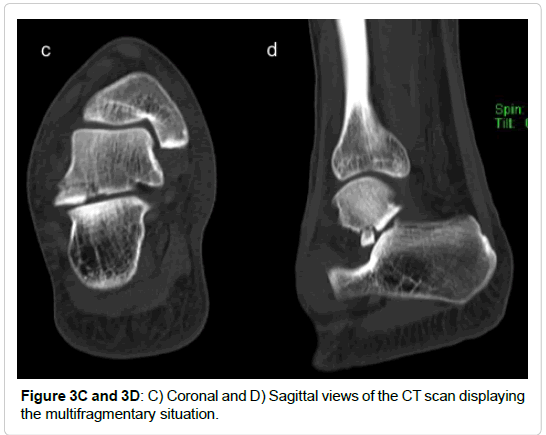
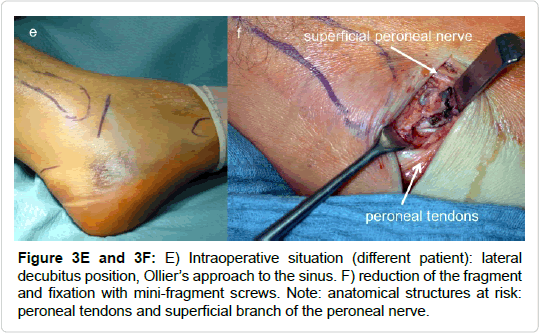
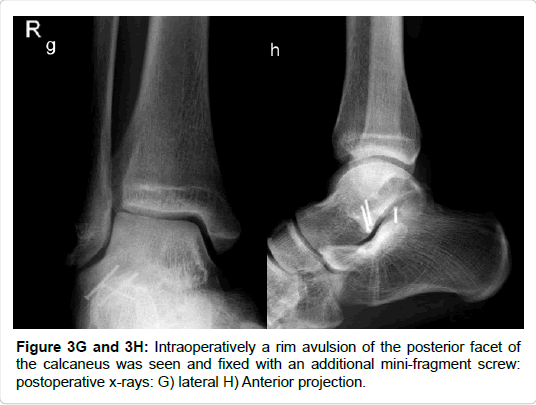
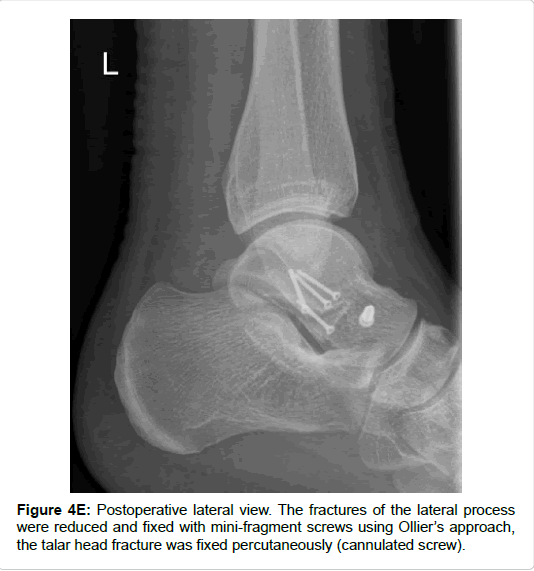
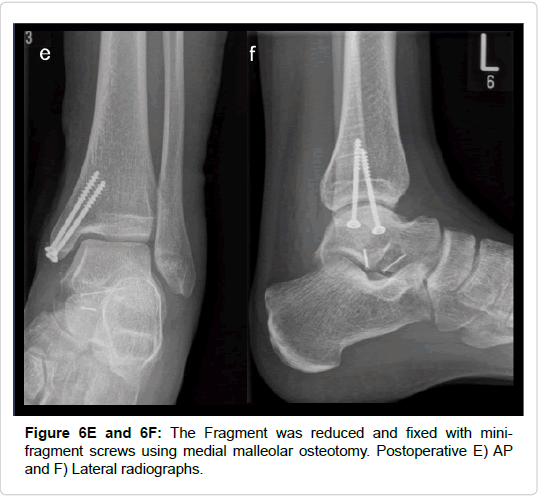
All included fractures were treated surgically (by 4 different surgeons). In cases of severe soft tissue injury, a joint-bridging, triangular external fixator was applied according to AO principles of damage control. Definitive treatment followed after soft tissue recovery. Approaches and implants are highlighted in Table 1 and Figures 3-7. For lateral process fractures a (limited) direct lateral approach, or Ollier’s approach were used (Figures 3E and 3F). In the case of concomitant injuries extended or combined approaches had to be used. For fractures of the posterior process a postero-lateral approach was used. Fractures of the medio-caudal ridge were more variable. According to the exact anatomy and location of the fracture a postero-medial approach or an osteotomy of the medial malleolus was used.
| No | Type of Fracture | Timing of surgery [days] |
Procedures | Approach |
|---|---|---|---|---|
| 1 | Lateral process | 17 | Mfx*, resection of fragment | Ollier |
| 2 | Lateral process | 4 | Screw fix, Resection of flake | Ollier |
| 3 | Osteochondral fracture | 4 | Screw fix, Brodstrom proc | Lateral |
| 4 | Lateral process | 10 | Screw fixation, locking plate | Extended lateral |
| 5 | Lateral process | 7 | Screw fix, resection of flake | Ollier extended lateral |
| 6 | Lateral process | 8 | Screw fix, Resection of flake | Extended lateral |
| 7 | Medio-caudal ridge | 21 | Screw fix, resection of flake | - |
| 8 | Osteochondral fracture | 10 | Arthroscopy fix with EthipinÒ | Arthros-copy |
| 9 | Posterior process (lateral tubercle) | 15 | Screw fix, EthipinÒ, M | Med. mall. osteotomy |
| 10 | Osteochondral fracture | 7 | Ex. fix, ORIF ankle fx, Fibrin glue | Lateral, medial |
| 11 | Osteochondral fracture | 8 | Ex. fix, ORIF ankle fx, Mfx | Lateral, medial |
| 12 | Osteochondral fracture | 10 | EthipinÒ | Osteotomy lat. Mall. |
| 13 | Medio-caudal ridge | 0 | Ex. fix | - |
| 14 | Lateral process | 7 | Screw fix | Medial |
| 15 | Posterior process (lateral tubercle) | 0 | Ex fix, screw fix | Postero-lateral |
| 16 | Medio-caudal ridge | 7 | Screw fix | Osteotomy med. mall. |
| *fx=Fracture, Mfx=Microfracturing | ||||
Table 1: Timing of surgery, procedures and approaches.
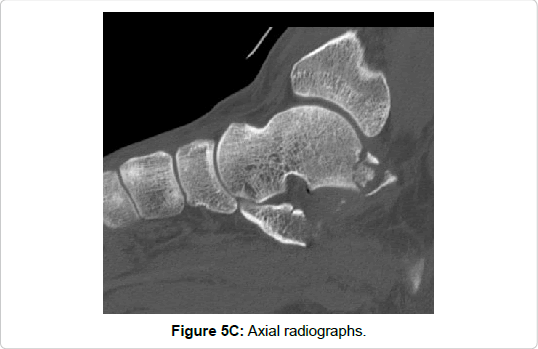
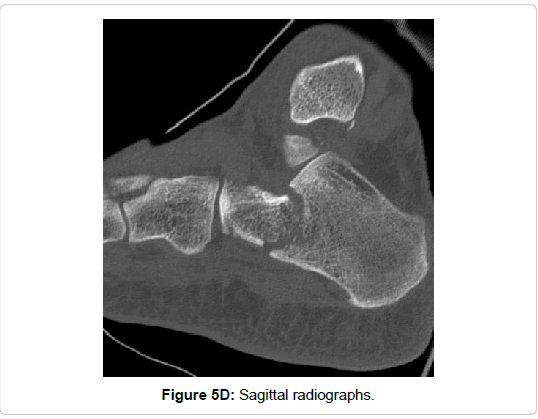
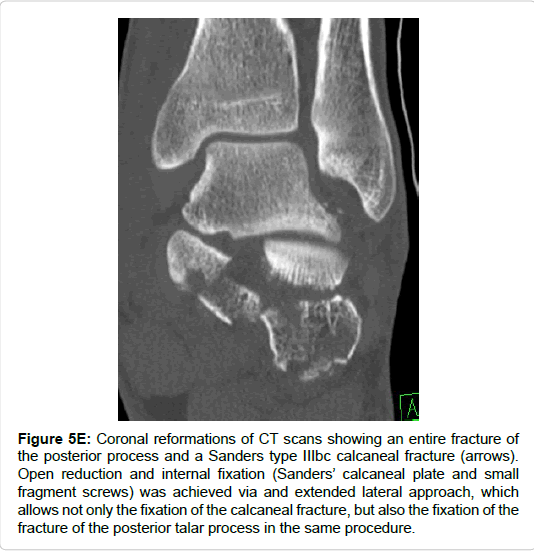
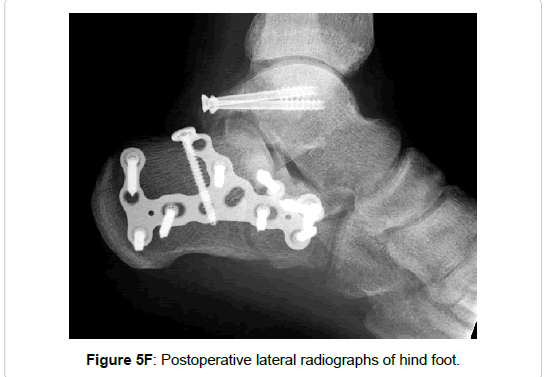
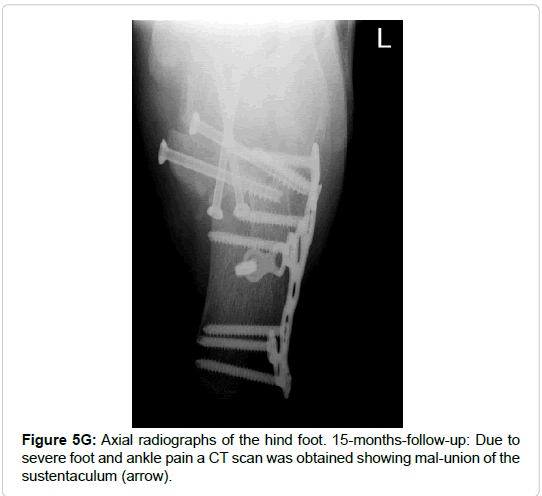
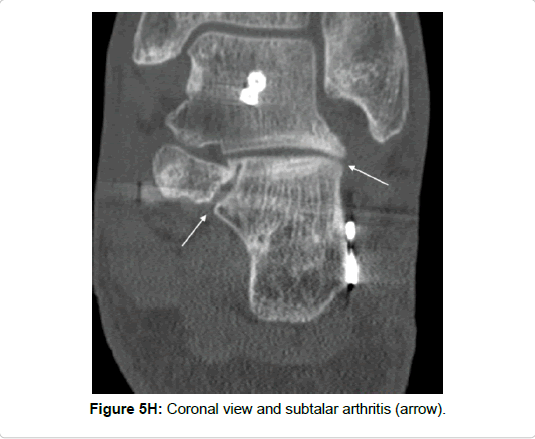
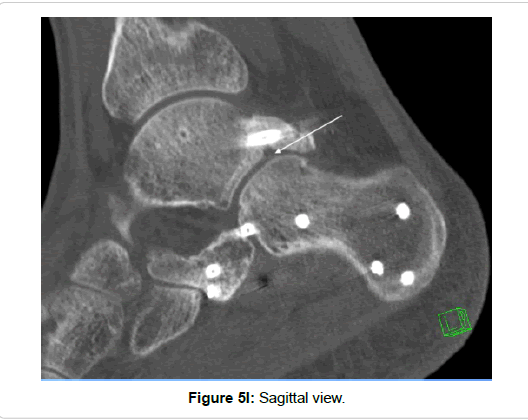
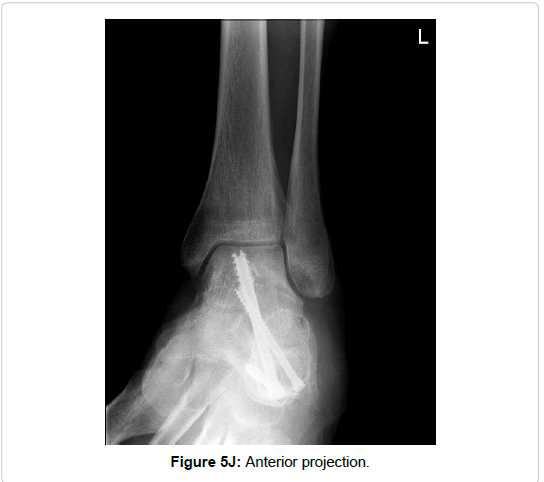
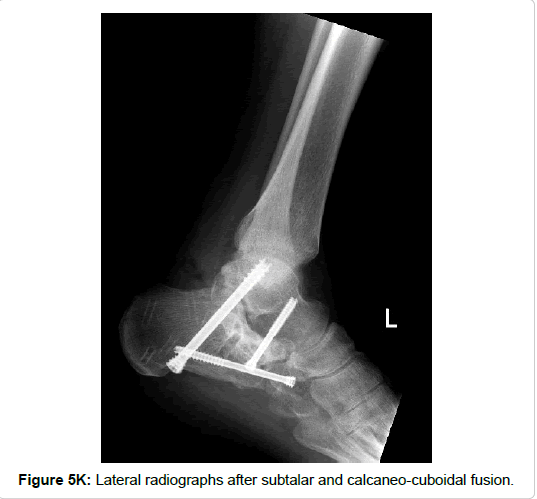
Figure 5e: Coronal reformations of CT scans showing an entire fracture of the posterior process and a Sanders type IIIbc calcaneal fracture (arrows). Open reduction and internal fixation (Sanders’ calcaneal plate and small fragment screws) was achieved via and extended lateral approach, which allows not only the fixation of the calcaneal fracture, but also the fixation of the fracture of the posterior talar process in the same procedure.
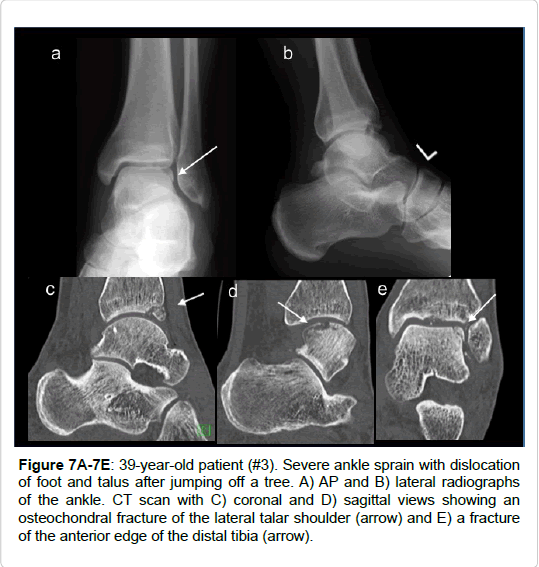
Figure 7A-7E: 39-year-old patient (#3). Severe ankle sprain with dislocation of foot and talus after jumping off a tree. A) AP and B) lateral radiographs of the ankle. CT scan with C) coronal and D) sagittal views showing an osteochondral fracture of the lateral talar shoulder (arrow) and E) a fracture of the anterior edge of the distal tibia (arrow).
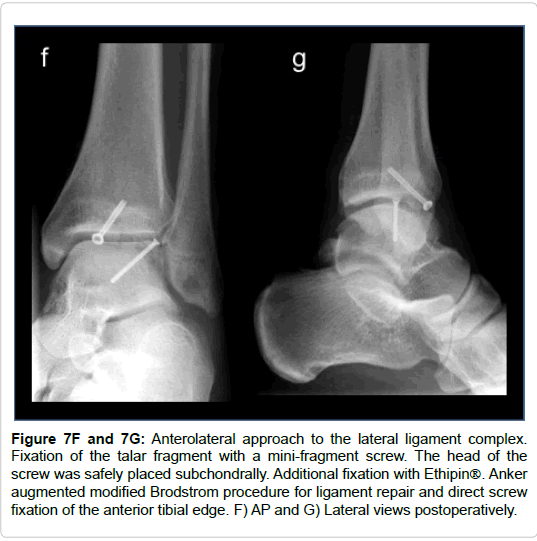
Figure 7F and 7G: Anterolateral approach to the lateral ligament complex. Fixation of the talar fragment with a mini-fragment screw. The head of the screw was safely placed subchondrally. Additional fixation with Ethipin. Anker augmented modified Brodstrom procedure for ligament repair and direct screw fixation of the anterior tibial edge. F) AP and G) Lateral views postoperatively.
Fixation of the fractures was achieved using different types (small and mini fragment cortical screws, headless cannulated compression screws) and sizes (2.0–3.5 mm) of screws.
All patients received pain treatment perioperatively. A single-shot antibiotic treatment was administered preoperatively. None of the subjects received postoperative antibiotic treatment.
Postoperatively all subjects received a walker (VACoped®) for 6 weeks. Free range of motion was allowed after wound healing. Partial weight-bearing was encouraged for 6 weeks. All patients received physical therapy postoperatively (lymphatic drainage, mobilization).
Mean follow up was 16 months (range 12–20 month). The records of all patients were analyzed retrospectively for trauma mechanism, concomitant injuries, the number and type of surgical interventions, timing of surgery and complications. All Subjects had routine followup visits at 6 and 12 weeks, 6 months and one year with a clinical and radiological evaluation. All subjects were seen by two senior foot and ankle surgeons during their visits. The American Orthopaedic Foot and Ankle Score (AOFAS hindfoot score) and the EQ-5D, a standardized instrument for measuring generic health status, were recorded [22].
The radiological investigation consisted in standing anteriorposterior and lateral views of the ankle, dorso-plantar and lateral views of the foot as well as Broden views to evaluate fracture reduction, implant integrity and foot position. Bony union was assessed at 12 months using CT scans.
Statistical analysis
Data are reported either as mean and standard deviation (SD) or median and range. Statistical analysis was performed using SPSS 21.0. Nonparametric statistical tests (Spearman Rank Correlation Coefficient) were used to determine a meaningful association or difference between the parameters and groups where indicated for this small series. Statistical significance was assumed with p<0.05.
Results
During the 5-year period 16 consecutive peripheral talar fractures (52% of all fractures of the talus) were recorded in our hospital information system. They consisted in 3 isolated fractures. 13 subjects presented with concomitant ipsilateral (12) and contralateral (1) injuries. 2 subjects suffered additional spine fractures, and 4 subjects were polytraumatized (ISS>16). None of the patients had relevant comorbidities affecting treatment or outcome.
Table 2 summarizes the demographic data. Mean age was 38 years (18-61). During initial workup all subjects obtained conventional x-rays and CT scans. 9 subjects received an additional MRI scan (Table 2).
| No | Age (years) | Fracture type | Injury mechanism | Concomitant injury | Multiple injury | Soft tissue injury* | MRI |
|---|---|---|---|---|---|---|---|
| 1 | 54 | Lateral process | Fall from height | Wrist fx**, Soft tissue injury knee | x | 2° | - |
| 2 | 32 | Lateral process | Fall from height/ Climbing |
- | - | 1° | - |
| 3 | 39 | Osteochondral fracture | Jumping | Dislocation of the foot, tibia fx | - | 2° | x |
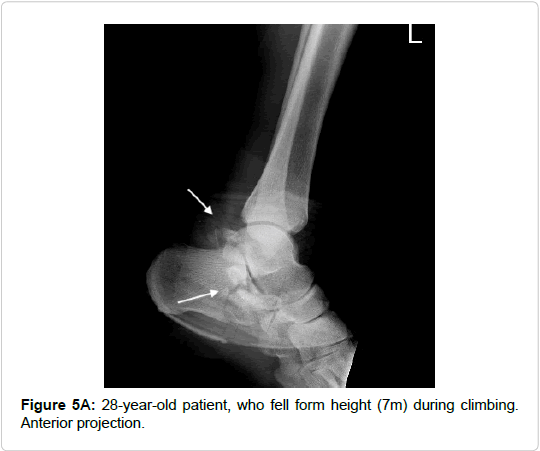
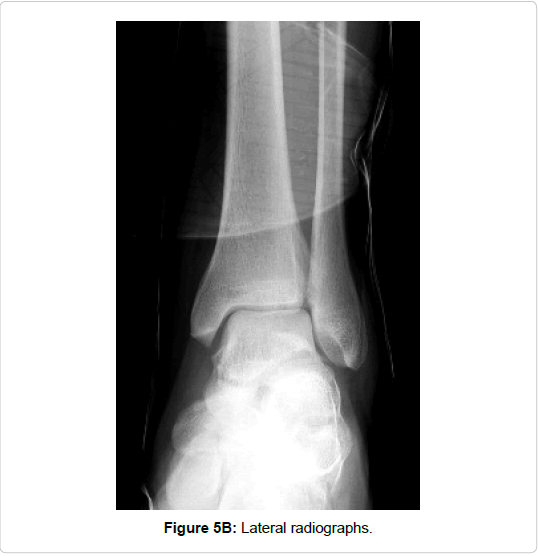
| 4 | 28 | Lateral process | Fall from height | Calcaneal fx | - | 3° | - |
| 5 | 49 | Lateral process | Supination | - | - | 2° | - |
| 6 | 62 | Lateral process | Fall from height | Calcaneal fx, TH 12, L1 fx | x | 2° | - |
| 7 | 31 | medio-caudal ridge | Supination | Subtalar dislocation | x | 2° | x |
| 8 | 17 | Osteochondral fracture | Gymnastics | Syndesmosis | - | 1° | x |
| 9 | 19 | posterior process (lateral tubercle) | Fall from height | L1 fx | x | 2° | - |
| 10 | 60 | Osteochondral fracture | Black ice | Ankle fx | - | 3° | x |
| 11 | 28 | Osteochondral fracture | Boulder | Ankle fx | - | 3° | x |
| 12 | 21 | Osteochondral fracture | Jumping | Contralateral calcaneal fracture. | - | 2° | x |
| 13 | 60 | Medio-caudal ridge | Fall from height | Extrusion of talus | - | 3° | x |
| 14 | 23 | Lateral process | Mountain bike | Calcaneal fx Talar head fx | - | 2° | |
| 15 | 45 | posterior process (lateral tubercle) | Trampoline | Extrusion of talus | - | 3° open | x |
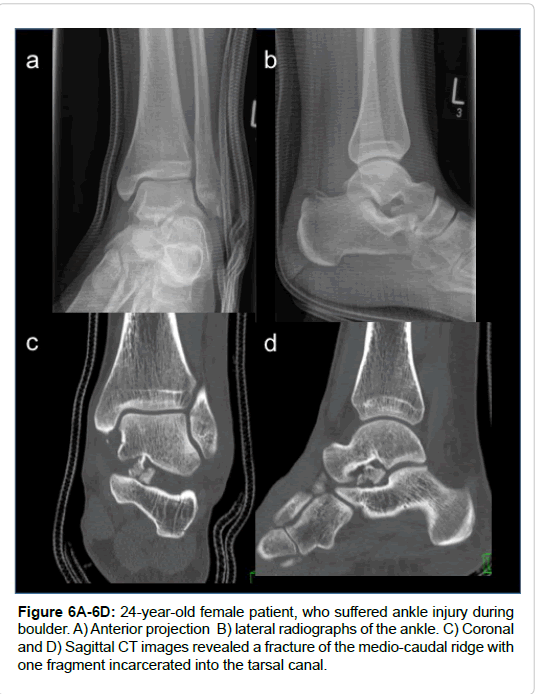
| 16 | 24 | medio-caudal ridge | Boulder | - | - | 2° | x |
| *Soft tissue injury according to tscherne’s classification. **fx=Fracture, Mfx=Microfracturing. |
|||||||
Table 2: Demographic data, fracture type, injury mechanism and diagnostics.
All fractures were treated surgically after careful preoperative planning. Surgical timing approaches and implants used are elaborated in Table 1. Facture fixation was considered for all articular steps or gaps of more than 2 mm. Fragments smaller than 2 mm were resected. If chondral delamination was present microfracturing of the subchondral bone was considered. Screws-size for fixation was based on fragment dimensions (2.0 – 3.5 mm).
During the follow up (mean 16 months) no general complications were recorded. Specifically, no wound healing problems, or infections were seen. The recorded AOFAS (mean ± SD) score was 87.3 ± 6.6 and the EQ5-D 0.91 ± 0.06. Four subjects showed mild osteoarthritis, 1 patient with lateral process fracture and concomitant ipsilateral calcaneal fracture (Sanders type IIC) received subtalar and CC-joint fusion. None of the patients developed chronic instability. Implant removal was necessary in 5 patients, either after osteotomy of the medial or lateral malleolus or after plate osteosynthesis of concomitant fractures. Indications for implant removal were local discomfort and in one case prior to subtalar fusion. Orthotics were recommended in 4 subjects (patients No. 4,6,10 and 15). Detailed results are reported in Table 3. Figures 3-7 show 5 typical cases of peripheral talar fractures.
| No | Type of fracture | Follow-up | Outcome AOFAS |
Outcome EQ5-D |
Outcome, interventions |
|---|---|---|---|---|---|
| 1 | Lateral process | 15 | 85 | 0.887 | - |
| 2 | Lateral process | 17 | 85 | 0.887 | - |
| 3 | Osteochondral fracture | 15 | 90 | 0.887 | - |
| 4 | Lateral process | 15 | - | - | Subtalar arthrodesis |
| 5 | Lateral process | 20 | 85 | 0.887 | - |
| 6 | Lateral process | 15 | 85 | 0.887 | Implant removal |
| 7 | medio-caudal ridge | 12 | 90 | 0.999 | - |
| 8 | Osteochondral fracture | 15 | 100 | 1 | - |
| 9 | posterior process (lateral tubercle) | 18 | 87 | 0,877 | - |
| 10 | Osteochondral fracture | 18 | 83 | 0,788 | Implant removal |
| 11 | Osteochondral fracture | 18 | 87 | 0,887 | Implant removal, arthroscopy |
| 12 | Osteochondral fracture | 18 | 90 | 0,999 | Implant removal |
| 13 | Medio-caudal ridge | 18 | 87 | 0,887 | - |
| 14 | Lateral process | 18 | 77 | 0,887 | - |
| 15 | posterior process (lateral tubercle) | 12 | 78 | 0,887 | - |
| 16 | Medio-caudal ridge | 12 | 100 | 1 | Implant removal |
Table 3: Follow-up, outcome.
Discussion
Even if all fractures of the talus are taken together, they remain a rare injury. The epidemiology of talar fractures, central or peripheral, remains unclear. Most studies are case series. Even so called epidemiological studies on talus fractures do not report more than 30 fractures [23]. In our case series peripheral fractures were seen as often as talar neck and body fractures. This is supported by recent radiological evaluation of 132 fractures of the talus that suggested that peripheral talus fractures are much more frequent than expected [4].
Patient collectives depend on the level of the trauma centre and the location of the hospital (rural or urban) [24,25]. This series describes the patient collective of a level II trauma centre in an urban environment (620.000 inhabitants).
Although peripheral fractures are a heterogeneous entity they shared some common traits. Most of the fractures in our series (12/16) were associated with sports activities. All fractures were related to high energy injuries: fall from height, boulder, climbing, trampoline. These findings are supported by almost all case series [7,26-29].
Peripheral fractures of the talus need a high index of suspicion due to the difficulty to diagnose and classify these fractures on plain x-rays. Recognition of these fractures is important because
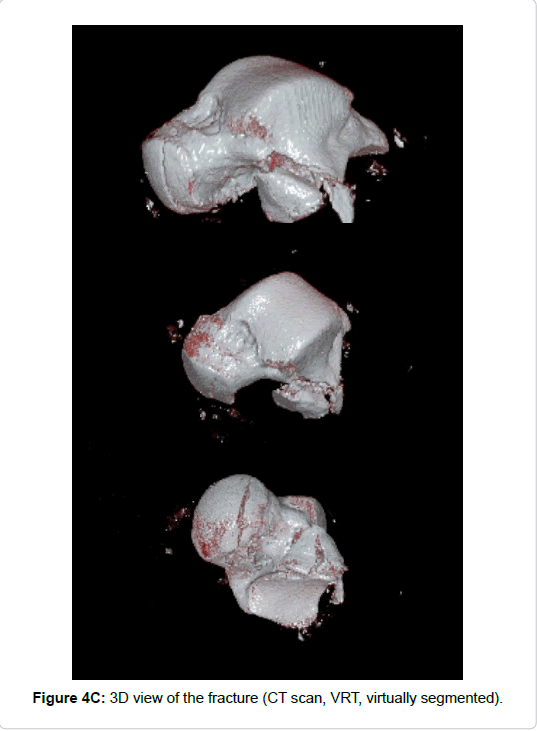
they can lead to severe limitations in ankle and subtalar function [29]. In this series all patients received CT scans for diagnosis and 9/16 subjects obtained MRI scans in addition. Important information can be gained using CT scans with multiplanar reformation. 3D reconstructions of the CT scans (volume rendering technology (VRT) with or without segmentation) might be helpful to better understand fracture morphology and to plan surgical treatment [17]. If ligament, tendon, or cartilage injuries are suspected and conservative treatment is aimed at MRI scans are mandatory [30].
In this case series fractures of the lateral process were seen with the highest incidence, followed by osteochondral fractures of the lateral talar shoulder. Fractures of the posterior process or medio-caudal ridge of the talus were observed less frequently. This is well supported by literature [12,13,31-33]. We had no problems to differentiate types of fractures. It might, however, be difficult to discern fractures of the entire posterior process from posteriorly located body fractures. Concomitant injuries were frequent (13/16). This was reported by others as well [4]. Complex injuries of the foot were excluded in this series due to the severe soft tissue compromise, and therefore different outcome.
Subtle OCL associated with ankle fractures might have been missed due to limitations of documentation or data-base search, although we routinely checked for osteochondral lesion in all ankle dislocation fractures intraoperatively, as proposed by Aktas et al. [34]. In their retrospective study of 86 arthroscopically assisted ankle fractures they found osteochondral lesions - above all - in distal fibular fractures (14/20).
Isolated trauma of the foot was recorded in 11/16 cases. One case was associated with a contralateral calcaneal fracture (Figure 5) and 4 patients were polytraumatized.
Almost all case reports and review articles on the topic stress the fact that surgical treatment of displaced fractures of the talar processes seems to be the best choice for successful outcome [2]. In these case series screw fixation of the fragments, or-if too small–removal is advocated. Delayed union, non-union, posttraumatic subtalar arthritis, are reported as the typical complications of peripheral talar fractures [2]. A few reports also describe impingement or tarsal tunnel syndrome as sequela of this fracture entity [35-38]. Secondary interventions are frequent, they comprise implant removal, arthrolysis and debridement of the joint surface. For osteochondral lesions secondary cartilage repair procedures like microfacturing, osteochondral transfer or autologous chondrocyte transplantation have been described as well [39-42]. However, these interventions did not play any role in this series.
Subtalar and calcaneo-cuboidal joint fusion was necessary in one patient with a fracture of the entire posterior process. However, rather due to the concomitant calcaneal fracture (Sanders type III) than due to the peripheral talar fracture (Figures 5H and 5K).
Outcome was generally excellent, unless combined injuries were present, like ipsilateral calcaneal fractures. In this respect peripheral talar fractures are in clear contrast to talar neck or body fractures [43]. AOFAS scores ranged between 77 and 100. Several authors reported less favourable outcome if a talar or subtalar dislocation was present [9,10,44,45]. In our series this was the case in 4/16 patients. However, we did not observe a significant worse outcome (AOFAS-Score) in patients with dislocations (Spearman rank correlation, p=0.823). This might be attributed to the small number of patients and the heterogeneous collective of patients with different types of peripheral talar fractures. Mild osteoarthritis was seen radiographically in 2 additional patients and cartilage damage on MRI in another two patients. Therefore, we cannot exclude the development of further osteoarthritic changes with longer follow-up.
Parsons et al. reviewed the existing case series of fractures of the lateral process in 2003 [46]. They reported good result in almost all cases if treated surgically, whereas non-operatively treated patients showed good results only in 60%. They reported non-unions in 60% (vs. 5%) for conservative treatment. Much less data is available for fractures of the posterior process and, due to the heterogeneity, also for osteochondral fractures of the lateral shoulder of the talus. The tenor of the existing reports, however, is the same as above: excellent results with surgical treatment and bad results when fractures are neglected [12,47].
The major limitation of this case series–as with all publications on the topic - is the limited number of patients. As with other rare injuries only case reports or limited case series have been published. However, it is one of the few case series comparing peripheral talar fractures and presenting objective and patient reported outcome measurements after a minimum follow-up of 12 months. Several publications emphasize that fracture of the postero-medial tubercle may lead to posterior ankle impingement [48]. Therefore, we advocate surgical treatment. However conservative treatment has been shown to be successful as well [36].
Conclusion
Peripheral talar fractures are uncommon but important injuries, that may result in significant disability if the diagnosis is neglected and proper treatment delayed. To avoid this a high index of suspicion is necessary in all patients with acute ankle pain and suitable trauma.
CT scans are mandatory to analyse the injury properly and to plan surgical treatment, which is indicated for fragments larger than 5 mm or, fracture displacement of more than 2 mm involving the articular surface. In the majority of the cases a mini-open or arthroscopicassisted reduction and (cannulated) screw fixation is required. Very small and comminuted fragments may be excised. With this long-term complication, including mal-union, non-union or severe subtalar joint osteoarthritis is avoided.
References
- Richter M (2013) Peripherial talar fractures. Oper Orthop Traumatol 25: 542-553.
- Boack DH, Manegold S (2004) Peripheral talar fractures. Injury 35 : 23-35.
- Peml M, Kalal P, Kopacka P, Kloub M (2016) Peripheral factures of the talus. Mid-term results. Acta Chir Orthop Traumatol Cech 83: 399-404.
- Dale JD, Ha AS, Chew FS (2013) Update on talar fracture patterns: A large level I trauma center study. AJR Am J Roentgenol 201: 1087-1092.
- von Knoch F, Reckord U, von Knoch M, Sommer C (2007) Fracture of the lateral process of the talus in snowboarders. J Bone Joint Surg Br 89: 772-777.
- Bladin C, Giddings P, Robinson M (1993) Australian snowboard injury data base study. A four-year prospective study. Am J Sports Med 21: 701-704.
- Boon AJ, Smith J, Zobitz ME, Amrami KM (2001) Snowboarder's talus fracture. Mechanism of injury. Am J Sports Med 29: 333-338.
- Shepherd FJ (1882) A Hitherto undescribed fracture of the astragalus. J Anat Physiol 17: 79-81.
- Chen YJ, Hsu RW, Shih HN, Huang TJ (1996) Fracture of the entire posterior process of talus associated with subtalar dislocation: A case report. Foot Ankle Int 17: 226-229.
- Park CH, Park KH (2016) Fracture of the posterior process of the talus with concomitant subtalar dislocation. J Foot Ankle Surg 55: 193-197.
- Cedell CA (1974) Rupture of the posterior talotibial ligament with the avulsion of a bone fragment from the talus. Acta Orthop Scand 45: 454-461.
- Kim DH, Berkowitz MJ, Pressman DN (2003) Avulsion fractures of the medial tubercle of the posterior process of the talus. Foot Ankle Int 24: 172-175.
- Kim DH, Hrutkay JM, Samson MM (1996) Fracture of the medial tubercle of the posterior process of the talus: A case report and literature review. Foot Ankle Int 17: 186-188.
- Ibrahim MS, Jordan R, Lotfi N, Chapman AWP (2015) Talar head fracture: A case report, systematic review and suggested algorithm of treatment. Foot 25: 258-264.
- Josten C, Rose T (1999) Acute and chronic osteochondral lesions of the talus. Orthopade 28: 500-508.
- McCriskin BJ, Cameron KL, Orr JD, Waterman BR (2015) Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop 6 : 161-171.
- Roll C, Schirmbeck J, Muller F, Neumann C, Kinner B (2016) Value of 3D reconstructions of CT scans for calcaneal fracture assessment. Foot Ankle Int 37: 1211-1217.
- Bali K, Prabhakar S, Gahlot N, Dhillon MS (2011) Neglected lateral process of talus fracture presenting as a loose body in tarsal canal. Chin J Traumatol 14: 379-382.
- Funasaki H, Kato S, Hayashi H, Marumo K (2014) Arthroscopic excision of bone fragments in a neglected fracture of the lateral process of the talus in a junior soccer player. Arthrosc Tech 3: 331-334.
- Kinner B, Tietz S, Muller F, Prantl L, Nerlich M, et al. (2011) Outcome after complex trauma of the foot. J Trauma 70:159-168.
- Zwipp H, Dahlen C, Randt T, Gavlik JM (1997) Complex trauma of the foot. Orthopade 26: 1046-1056.
- Malviya A, Makwana N, Laing P (2007) Correlation of the AOFAS scores with a generic health QUALY score in foot and ankle surgery. Foot Ankle Int 28: 494-498.
- Sakaki MH, Saito GH, de Oliveira RG, Ortiz RT, Silva Jdos S, et al. (2014) Epidemiological study on talus fractures. Rev Bras Ortop 49 (4):334-339.
- Howard J, Sundararajan R, Thomas SG, Walsh M, Sundararajan M (2006) Reducing missed injuries at a level II trauma center. J Trauma Nurs 13: 89-95.
- Cudnik MT, Newgard CD, Sayre MR, Steinberg SM (2009) Level I versus Level II trauma centers: An outcomes-based assessment. J Trauma 66: 1321-1326.
- Chan GM, Yoshida D (2003) Fracture of the lateral process of the talus associated with snowboarding. Ann Emerg Med 41: 854-858.
- Correia SI, Silva-Correia J, Pereira H, Canadas RF, da Silva Morais A, et al. (2017) Posterior talar process as a suitable cell source for treatment of cartilage and osteochondral defects of the talus. J Tissue Eng Regen Med 11: 1949-1962.
- Lunebourg A, Zermatten P (2014) Fracture of the lateral process of the talus: A report of two cases. J Foot Ankle Surg 53: 316-319.
- Sariali E, Lelievre JF, Catonne Y (2008) Fractures of the lateral process of the talus. Retrospective study of 44 cases. Rev Chir Orthop Reparatrice Appar Mot 94: 1-7.
- Park J, Che JH (2018) Talus fracture of the medial tubercle of the posterior process: Interposition of the flexor hallucis longus tendon. J Foot Ankle Surg (Article in Press).
- Dougall TW, Ashcroft GP (1997) Flexor hallucis longus tendon interposition in a fracture of the medial tubercle of the posterior process of the talus. Injury 28: 551-552.
- Ebraheim NA, Patil V, Frisch NC, Liu X (2007) Diagnosis of medial tubercle fractures of the talar posterior process using oblique views. Injury 38:1313-1317.
- O'Loughlin P, Sofka CM, Kennedy JG (2009) Fracture of the medial tubercle of the posterior process of the talus: Magnetic resonance imaging appearance with clinical follow-up. HSS J 5:161-164.
- Aktas S, Kocaoglu B, Gereli A, Nalbantodlu U, Guven O (2008) Incidence of chondral lesions of talar dome in ankle fracture types. Foot Ankle Int 29: 287-292.
- Wang PH, Su WR, Jou IM (2016) Lateral hindfoot impingement after nonunion of fracture of the lateral process of the talus. J Foot Ankle Surg 55: 387-390.
- Watanabe H, Majima T, Takahashi K, Kawaji H, Takai S (2017) Split fracture of the posteromedial tubercle of the talus: Case report and proposed classification system. J Foot Ankle Surg 56: 187-190.
- Cetinkal A, Topuz K, Kaya S, Colak A, Demircan MN (2011) Anterior tarsal tunnel syndrome secondary to missed talus fracture: A case report. Turk Neurosurg 21: 259-263.
- Stefko RM, Lauerman WC, Heckman JD (1994) Tarsal tunnel syndrome caused by an unrecognized fracture of the posterior process of the talus (Cedell fracture): A case report. J Bone Joint Surg Am 76: 116-118.
- Anthonissen J, Rommens PM, Hofmann A (2016) Mosaicplasty for the treatment of a large traumatic osteochondral femoral head lesion: a case report with 2 year follow-up and review of the literature. Arch Orthop Trauma Surg 136: 41-46.
- Largey A, Faure P, Hebrard W, Hamoui M, Canovas F (2009) Osteochondral transfer using a transmalleolar approach for arthroscopic management of talus posteromedial lesions. Orthop Traumatol Surg Res 95: 537-542.
- Liu W, Liu F, Zhao W, Kim JM, Wang Z, et al. (2011) Osteochondral autograft transplantation for acute osteochondral fractures associated with an ankle fracture. Foot Ankle Int 32: 437-442.
- Badekas T, Takvorian M, Souras N (2013) Treatment principles for osteochondral lesions in foot and ankle. Int Orthop 37: 1697-1706.
- Xue Y, Zhang H, Pei F, Tu C, Song Y, et al. (2014) Treatment of displaced talar neck fractures using delayed procedures of plate fixation through dual approaches. Int Orthop 38: 149-154.
- Ebraheim NA, Skie MC, Podeszwa DA (1994) Medial subtalar dislocation associated with fracture of the posterior process of the talus. A case report. Clin Orthop Relat Res 303: 226-230.
- Liu Z, Zhao Q, Zhang L (2012) Medial subtalar dislocation associated with fracture of the posterior process of the talus. J Pediatr Orthop B 21: 439-442.
- Parsons SJ (2003) Relation between the occurrence of bony union and outcome for fractures of the lateral process of the talus: A case report and analysis of published reports. Br J Sports Med 37: 274-276.
- Bhanot A, Kaushal R, Bhan R, Gupta PN, Gupta RK, et al. (2004) Fracture of the posterior process of talus. Injury 35 (12):1341-1344.
- Mas Martinez J, Verdu Roman C, Martinez Gimenez E, Sanz-Reig J, Bustamante Suarez de Puga D, et al. (2017) Arthroscopic treatment of a malunion of a posteromedial tubercle fracture of the talus. Arthrosc Tech 6: 2107-2110.
Citation: Roll C, Kinner B (2018) Peripheral Talus Fractures-A Clinical Observational Study of 16 Cases. Clin Res Foot Ankle 6: 264. DOI: 10.4172/2329-910X.1000264
Copyright: © 2018 Roll C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7511
- [From(publication date): 0-2018 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 6565
- PDF downloads: 946