Pre-Operative Occupational Therapy for Patients Having Total Hip Replacements
Received: 06-Sep-2017 / Accepted Date: 13-Oct-2017 / Published Date: 16-Oct-2017 DOI: 10.4172/2161-0711.1000563
Abstract
This evidence-based project implemented a pre-operative education class designed by an occupational therapist (OT). In total, 14 participants scheduled for an elective posterior lateral total hip replacement (THR) were recruited. The class focused on post-surgical precautions following a posterior lateral total hip replacement, performing activities of daily living (ADL's) while following specified precautions, and modifying the home as needed to facilitate performance of daily activity. A 15 question Knowledge Inventory (KI) and the Speilberger State Trait Anxiety Inventory (STAI 6) was administered before and immediately after the intervention. Results indicated that participants felt prepared after receiving this intervention, results on the KI significantly improved post intervention and although their anxiety fluctuated prior to and post intervention, they felt the content within the class was important to hear.
Keywords: Education; Hip arthritis; Durable medical equipment; Precautions; Activities of daily living; Anxiety
Introduction
In the United States, the length of stay at a hospital following a total hip replacement (THR) has drastically decreased from several weeks to roughly three days [1]. While the amount of time a patient can stay at the hospital has been reduced, education on safety and restrictions post discharge is lacking.
Restrictions associated with posterior lateral hip replacements involve no bending past a 90° angle, no turning the operated leg in, and not crossing ones legs [2]. The restrictions result in a client modifying the way in which he or she performs activities of daily living (ADLs). Improving functional independence is a key component to the practice of occupational therapy [3]. In order to achieve this in clients having a THR, an occupational therapist must educate the client on the use of durable medical equipment, which includes a: raised toilet seat, reacher, sock aide and shoe horn [3]. The study conducted by Havixbeck et al. concluded that although patients were satisfied with the education they received from an occupational therapist, they would have preferred more time and additional practice.
There are numerous studies that focused on the benefits of preoperational education classes. Dore et al. found that clients who attended a pre-operative education class had a reduced hospital stay by three days without altering patient satisfaction [4]. Some of the benefits include decreasing anxiety, decreasing pain, decreasing length of stay and increasing patient satisfaction. A study compared clients who attended an education session prior to surgery to those who did not. The study concluded that clients who had education prior to surgery had a reduced length of stay [5]. According to Hodgekinson pre-operative teaching offers clients the ability to receive the material ahead of time, allowing them the ability to process the information and absorb it, thus resulting in improved outcomes post operation.
The goal of this evidence-based project was to determine the effects of providing occupational therapy to patients before undergoing a posterior lateral hip replacement. Having a preoperative occupational therapy consult and education session regarding precautions and durable medical equipment can decrease clients’ anxiety. In a study involving 239 patients, 70% experienced preoperative anxiety [6]. Anxiety can result from a client’s inability to focus on a task. Clients are extremely overwhelmed after surgery resulting in difficulty retaining information. If preoperative education is not available for clients, they typically receive the majority of the information for the first time after surgery. This project focused on if clients feel prepared for surgery after receiving preoperative rehabilitation.
This project, conducted at the Hospital for Special Surgery, focused on whether participants feel prepared for surgery after receiving preoperative education. At the Hospital for Special Surgery, the current clinical pathway for clients having a THR is two days [1]. Clinical pathways provide goals for both the client and the caregiver. The pathways outline the steps one must take to achieve these goals [1].
Clients who are undergoing a surgery that requires an overnight stay at the hospital do not see a therapist prior to the procedure. Total hip replacements require clients to stay in the hospital for one to two days. As a result, clients having THRs are not seen by a physical or occupational therapist prior to surgery at the Hospital for Special Surgery. Instead, clients are given the opportunity to attend a brief presurgical class run by nursing. This class focuses on the hospital stay and does not discuss physical or occupational therapy in detail or what to expect post-surgery.
Participants
Surgeons served as the referral source for this project. The 14 participants were recruited either via the total joint replacement class offered at the Hospital for Special Surgery, through the office administrators of the surgeons that agreed to participate in this project, or individually by this author as they were checking in for the total joint class. Over the six-week implementation of this project, 14 participants completed the intervention. Initially, 24 individuals were interested in participating in this evidence-based project. Out of the initial 24 who volunteered to participate in this project, 10 individuals did not meet the inclusion criteria because their surgeons did not provide consent through the IRB. Out of the 14 participants who did meet the inclusion criteria, 64%, were female, while five (35%) were male.
Measures
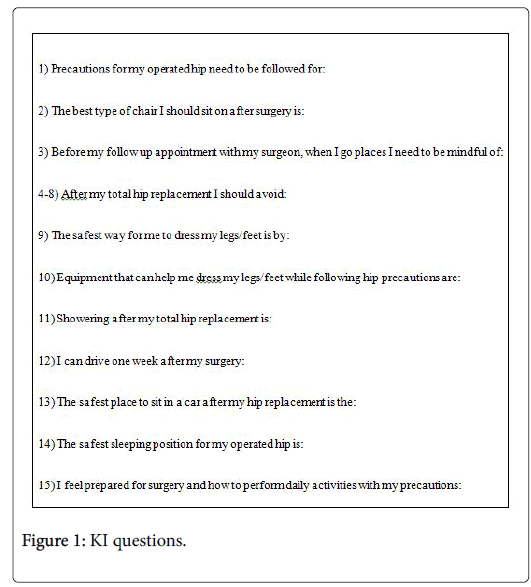
Currently, there are no existing reliable and valid assessments that measure a client’s knowledge of precautions and preparedness after a total hip replacement. The Knowledge Inventory (KI) was designed by the author and incorporated extensive feedback from other inpatient and outpatient clinicians. It contained 15 multiple choice questions that asked participants to accurately identify hip precautions they will need to incorporate in their daily lives after having a posterior lateral hip replacement (Figure 1).
The KI was administered prior to and immediately after the intervention to determine their ability to correctly identify the safest and most recommended ways to perform ADLs with THR precautions before and after pre-operative occupational therapy education “PreOp- OTed”.
The State Trait Anxiety 6 (STAI 6) was also given prior to and post intervention to determine participant’s level of anxiety at a given moment. The State Trait Anxiety 6 (STAI 6) has undergone reliability and validity testing [7]. The instrument has been found to be valid and reliable in numerous reliability and validity tests [8], making it an ideal choice for this project. Anxiety can have different definitions, depending on the situation. For the purpose of this project, anxiety was defined as the apprehensive feelings a patient may experience related to an upcoming medical procedure, associated restrictions and rehabilitation.
Data collection
Participants were given clickers that had corresponding numbers after signing the consent form. The clickers stayed with the same participant for the duration of the education class and were used to complete the KI prior to and immediately following the PreOp-OTed. This allowed the author the ability to compare results pre and post intervention while maintaining each individual’s anonymity.
The KI was administered through a PowerPoint; however paper versions were available as a precaution for PowerPoint malfunction. The benefit of the clicker system was that it automatically populated participant’s responses into an Excel spreadsheet. Printed copies of the STAI 6 were given pre and post intervention as well. This information was manually completed by participants and then added to Excel by the author [8-12].
Data analysis
After each education class, the Excel spreadsheet with participant’s responses to the pre and post intervention KI and STAI 6 were saved on a password protected computer. The data was organized in Excel by clicker number, KI and STAI 6. From there it was organized further by pre and post intervention responses [13-18]. To avoid bias, the author was blind to which participant had which clicker. Individuals were not asked to identify themselves in anyway during the intervention other than by surgeon and gender. A statistician was utilized during the design aspect of this project and she determined that a sign rank test would be beneficial in order to compare data pre and post intervention.
Results
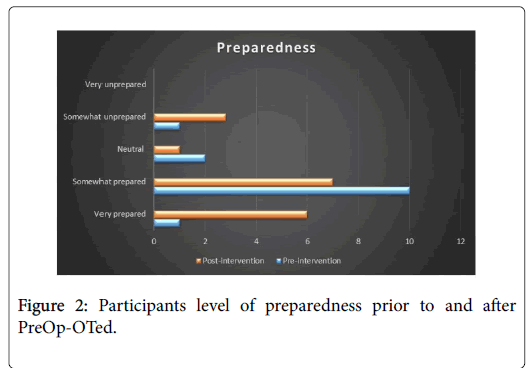
The KI was comprised of 15 questions, one of which involved the participant rating his or her level of perceived preparedness for surgery and performing daily activities with precautions. Out of 14 participants, only one felt less prepared after the intervention. Initially this person rated them self as “very prepared” and then after completion of the evidence-based project they felt “somewhat prepared.” Otherwise, the 13 other participants either felt equally as prepared post intervention or more prepared (Figure 2). Not one person before the intervention or after the intervention felt “very unprepared.” Interestingly, those that felt prepared prior to the intervention scored the lowest on the initial KI.
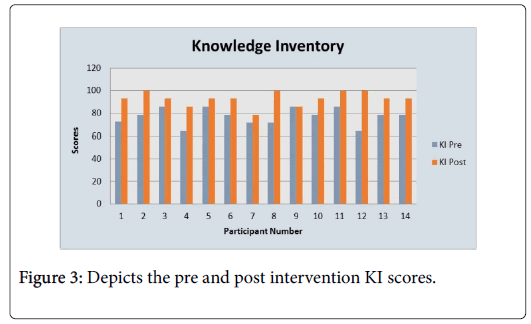
Therefore, although they felt prepared, they actually were unaware of their precautions. Figure 3 provides a summary of the KI results for participants pre-intervention as well as post intervention. Prior to the intervention, participant’s scores on the KI reflected the awareness they had for their precautions, which was minimal. After the intervention however, 93% of the KI scores increased overall, as compared to the pre-intervention scores. This indicates that participants were more aware of their precautions after the intervention, as they relate to daily activities [19-22].
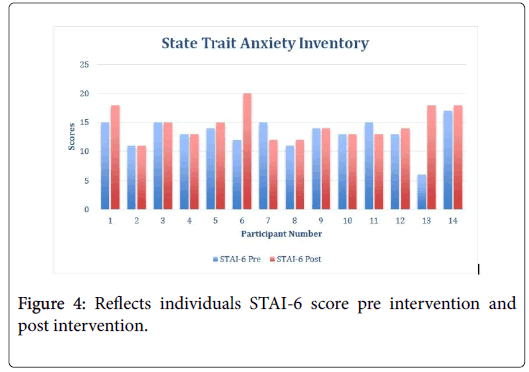
On the other hand, Figure 4 indicates the results of the pre as well as the post-intervention STAI-6. The results of the STAI-6 in regards to anxiety, 50% felt an increase in anxiety while 36% stayed the same throughout the intervention and 14% experienced a decrease in anxiety.
This indicates that some individuals experienced decreased level of anxiety after the completion of the PreOp-OTed while some stayed the same and some increased. Many factors could have contributed to this fluctuation as participants have several other pre-surgical screening appointments the same day this intervention occurred.
Although this author did not follow the participants postoperatively, with the IRB consent she was able to look their hospital length of stay up, which was noted within the electronic medical system [22-26]. Out of the 14 participants, nine of them were cleared from physical therapy in one day. However, at the Hospital for Special Surgery, the clinical pathway for an individual having a THR is two days. Therefore, although the participants were cleared from physical therapy prior to the pathway, they remained in the hospital throughout the allotted pathway time. Due to the small sample size, a statistical analysis would not yield meaningful results; therefore this type of testing was not performed.
Limitations
As with any project, this intervention had its limitations. One way this project was limited was due to its small sample size of 14 participants. It was also limited by the fact it only targeted participants that were having posterior lateral total hip replacements, versus anterior or modified hip replacements. Participants involved in this project were recruited on a voluntary basis and informed of the project; therefore, only clients who wanted to learn more participated. Additional limitations include not having a control group to compare results and the short time this project was performed [26-37]. Due to the short length of stay at the Hospital for Special Surgery, there was a limited opportunity to be flexible in terms of recruiting and implementing. The last perceived limitation of this project is that it took place in one day versus following up with patients in the hospital to administer the KI and STAI 6 post surgery. Further research is needed with a more diverse population not only in terms of surgical procedure and population but in terms of participants.
Conclusion
This evidence-based project correlated with the literature and has the potential to positively impact the OT profession. Education is a key aspect of the OT profession and is extremely important in terms of recovery. According to Gulotta et al. the length of stay for THRs at the Hospital for Special Surgery is two nights. The fact that the hospital stay is shorter means that individuals are returning home sooner and as a result, need to feel prepared to perform their ADLs earlier. Therefore, an OT consult educating clients on ways to perform ADLs with precautions is imperative. As indicated through the KI, prior to the intervention, participant’s scores were low, which means they were not aware of their precautions as they relate to ADLs. This indicates that patients are spending less time in the hospital and being discharged home prior to understanding their precautions. With this in mind, OT can play a critical role not only post-operatively, but also pre-operatively.
According to Gaston et al. patient’s satisfaction following joint arthroplasty is affected by completion and fulfillment of pre-surgical expectations. Patient satisfaction is often correlated with patient expectations being met. Therefore, pre-operative education provides individuals with realistic expectations for post-operative care. The concept of having patients and their family members educated by an OT prior to the surgery can help get the profession more recognized.
In summary, the administered KI indicated that participants felt prepared after the intervention and their scores reflected an increase in correct responses. On the other hand, the results of the STAI-6 fluctuated. However, several factors may have contributed to this. On the day this intervention took place they had several other appointments, and they had just previously attended the total joint class. Although the results varied, each participant reported to the author that they are glad he or she participated and found the content extremely valuable.
References
- Gulotta L, Lyman S, Nestor B, Padgett D, Sculco T, et al. (2011) Fast track THR: One hospital’s experience with a 2-day length of stay protocol for total hip replacement. HSS J 7: 223-228.
- Mechlengurg I, Mikkelsen L, Mikkelsen S, Peterson M, Soballe K (2014) Does reduced movement restrictions and use of assistive devices affect rehabilitation outcome after a total hip replacement? Eur J Phys Rehabil Med 50: 383-393.
- Havixbeck K, Finlayson M (1992) A post-discharge study on the use of assistive devices. Can J Occup Ther 59: 201-207.
- Dore C, Hughes S, McGregor A, Owen A, Rylands H (2004) Does preoperative hip rehabilitation advice improve recovery and patient satisfaction? J Arthroplasty 19: 464-468.
- Jones S, Alnaib M, Gibson A, Jones S, Kader D, et al. (2011) Preoperative patient education reduces length of stay after knee joint arthroplasty. Ann R Coll Surg Engl 93: 71-75.
- Belachew T, Nigussie S, Wolancho W (2014) Predictors of preoperative anxiety among surgical patients in Jimmy University Specialized Teaching Hospital, South Western Ethiopia. BMC Surgery 14: 1-10.
- Spielberger CD (1972) Anxiety: Current trends in theory and research. New York and London: Academic Press.
- Gorsuch R, Lushene R, Spielberger C, Vagg P (1983) Jacobs State-Trait Anxiety Inventory (STAI). American Psychological Association. Canada.
- Gaston P, Hamilton D, Howie C, Lane J, MacDonald D, et al. (2013) What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open 3: 1-8.
- American Occupational Therapy Association (2006) AOTA’s Centennial Vision.
- American Occupational Therapy Association [AOTA] (2014) Occupational therapy practice framework: Domain and process (3rd edn.) American Journal of Occupational Therapy 68: S1-S48.
- Babitu U, Christelis N, Dugal J, Liew S, Mutalima N, et al. (2015) An enhanced recovery after surgery program for hip and knee arthroplasty. Med J Aust 20: 363-368.
- Bedforth N, Foxall G, French J, Hardman J, Jlala H (2010) Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. British Journal of Anaethesia 104: 369-374.
- Berger B, Jennrich M, Kearney M, Lyons S, Robinson R (2011) Effects of preoperative education on patient outcomes after joint replacement surgery. Orthop Nurs 30: 391-396.
- Broad J, Collins M, Engelke S, Norwick J, Pellino T, et al. (1998) Increasing self-efficacy through empowerment: preoperative education for othropaedic patients. Orthop Nurs 17: 48-59.
- Centers for Disease Control and Prevention (2015) Changing Patterns in Hospitalization and Inpatient Surgery of Rural and Urban Residents.
- Chetty C, Ehlers D (2009) Orthopaedic patients’ perceptions about their pre-operative information.J Democratic Nurs Organization of South Africa 32: 55-60.
- Cole MB, Tufano R (2008) Applied theories in occupational therapy: A practical approach. Thorofare, NJ: SLACK.
- Crum K (2011) Readiness for discharge, occupation-based treatment in the orthopedic setting. OT Practice 16: 14-23.
- Daltroy L, Eaton M, LiangM, Morlino C, Poss R (1998) Preoperative education for total hip and total knee replacement patients. Arthritis Care Res 11: 469-478.
- Dwyer A, Porter P, Tarassoli P, Thomas W (2012) Enhanced recovery program in total hip arthroplasty. Indian J Orthop 46: 407-412.
- Stern C, Lockwood C (2000) Knowledge retention from pre-operative patient information. Int J Evid Based Healthc 3: 45-63.
- Evans P, Moulton L, Smith T, Starks I (2015) Pre-operative education prior to elective hip arthroplasty surgery improves postoperative outcome. Int Orthop 39: 1483-1486.
- Fisher G, Kielhofner G, Lee S, Taylor R (2008) Theory use in practice: a national survey of therapists who use the model of human occupation. Ame J Occup Ther 62: 106-117.
- Fitzpatrick E, Hyde A (2006) Nurse-related factors in the delivery of preoperative patient education. J Clin Nurs 15: 671-677.
- Foster JD, Francis NK, Jones EL, Middleton RG, Smith JR, et al. (2014) A systematic review of patient reported outcomes and patient experience in enhanced recovery after orthopaedic surgery. Ann R Coll Surg Engl 96: 89-94.
- Gorman K, Scott P, Stevens L, Nahm E (2012) Effects of a web-based preoperative education program for patients undergoing ambulatory surgery: A preliminary study. J Hospital Administration 1: 21-29.
- Gudnason V, Jonsson B, Jonsson H, Olafsson O, Iwarsson Set al. (2005) Short hospital stay augmented with education and home-based rehabilitation improves function and quality of life after hip replacement. Acta Orthopaedica 76: 555-562.
- Kielhofner G (2008) Model of human occupation: Theory and application. Occupational Therapy in Mental Health 25: 1.
- Kielhofner G (2009) Conceptual foundations of occupational therapy practice. Philadelphia, PA: F. A. Davis. 1: 149-174.
- Kruzik N (2009) When waiting-room brochures won’t do: Patient education requires a human touch. J Asso Perioperative Registered Nurs 90: 381-387.
- McDonald S, Page MJ, Wasiak J, Sprowson A (2014) Preoperative education for hip or knee replacement. Cochrane Database Syst Rev 1: CD003526.
- Spalding N (1995) A comparative study of the effectiveness of a preoperative education programme for total hip replacement patients. British J Occup Therapy 58: 526-531.
- Thomas C (2015) The hospital discharge race: Is sooner always better? Heart Sisters.
Citation: Keaney K, Lawdis K (2017) Pre-Operative Occupational Therapy for Patients Having Total Hip Replacements. J Community Med Health Educ 7: 563. DOI: 10.4172/2161-0711.1000563
Copyright: © 2017 Keaney K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 10215
- [From(publication date): 0-2017 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 9100
- PDF downloads: 1115