Process of Pulmonary Rehabilitation and Program Organization
Received: 13-May-2017 / Accepted Date: 12-Jun-2017 / Published Date: 19-Jun-2017
Abstract
Rehabilitation is recommended as a well-established intervention option for patients with chronic respiratory conditions, suffering from persistent symptomatology and disability. Pulmonary rehabilitation emphasizes the ability of the patient to adapt and self-manage in the face of physical, emotional and social challenges of life by addressing identified pulmonary and extra pulmonary traits as well as behavior and life style factors. In order to create added value for patients and society, pulmonary rehabilitation must be organized as a flexible, individualized, integrated intervention, based on partnering different skills. The general principles of such process-based organization are reviewed.
Keywords: Pulmonary rehabilitation; Chronic disease; Rehabilitation program
74307Introduction
Many patients with chronic respiratory diseases as chronic obstructive pulmonary disease (COPD) are left to cope with the consequences of their chronic, irreversible condition despite escalating symptomatic treatment. Such patients remain dyspneic, dysfunctional and disabled and suffer from a spectrum of comorbidities [1]. All guidelines recommend rehabilitation as a well-established treatment option for these patients in which complex interactions of physical, psychological, social and environmental factors contribute to disability. Indeed, the first authoritative statement of pulmonary rehabilitation from the American College of Chest Physicians, published in 1974, described pulmonary rehabilitation as an art of medical practice, wherein an individually tailored, multidisciplinary program was formulated which through accurate diagnosis, therapy, emotional support and education, stabilizes or reverses both physiopathological and psychopathological manifestations of pulmonary diseases. Also, it attempts to return the patient to the highest possible functional capacity allowed by the handicap and overall life situation [2]. In 1994, the National Institutes of Health defined pulmonary rehabilitation as a multidimensional continuum of services for the patient and the family supplied by an integrated team of specialists in complementary disciplines, having as goal the independent living and functioning of the patient within the society [3]. The ATS/ERS statements confirmed that pulmonary rehabilitation must be considered as a comprehensive intervention based on thorough assessment followed by patienttailored therapies designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors. The latter part of the definition fits with the concept that pulmonary rehabilitation should be both restorative and preventive [4,5]. The main points in common among the various definitions of pulmonary rehabilitation include (1) the focus on chronic respiratory patients and their care givers; (2) individualization of the intervention; (3) an ongoing multidisciplinary intervention; (4) outcomes based on physiological, psychological and social measures considering a global dimension to the individual’s health; and (5) stimulation of long-term adherence to health–enhancing behaviors in order to promote autonomy and social participation of the patient [6].
This consistent definition of pulmonary rehabilitation fits very well with the updated definition of health emphasizing the ability to adapt and self-manage in the face of social, physical and emotional challenges of life [7]. Indeed, the World Health Organization (WHO) definition of health as the state of complete physical, mental and social well-being no longer fits with the actual rise of chronic diseases [8].
The personalized therapy as put forward in the definition of pulmonary rehabilitation is recently revisited as a form of precision medicine for chronic airway diseases targeting identified pulmonary, extra-pulmonary traits of chronic airway diseases as well as the behavior and lifestyle risk factors of these chronic conditions [9]. Focusing on treatable traits in a multidimensional management plan can lead to highly significant improvements in physical, emotional and social functioning [10,11].
Organization of pulmonary rehabilitation
The multidimensional aspects of pulmonary rehabilitation requires skills associated with a variety of health professionals in order to offer an individualized comprehensive care plan based on identified treatable traits. This process of rehabilitation, offered by a dedicated team, is a complex interaction of health care providers around the patient.
First at all, individualization of pulmonary rehabilitation requires that the workforce be organized to offer health care around the patient: the workforce needs to adopt a patient-centered approach. This individualization of the program in a patient-centered approach needs to consider the patient as a partner in the program: information about treatment, goals, and outcomes is shared with patients to prepare them to take greater responsibility in health care decision making [12].
Furthermore, different definitions of pulmonary rehabilitation formulate that health care needs to be considered as a multidisciplinary program [2-5]. Multidisciplinarity can be defined as a non-integrative mixture of disciplines in that each discipline retains its methodologies and assumptions without change or development from other disciplines within the multidisciplinary relationship [13]. In a multidisciplinary relationship cooperation may be mutual but not interactive. Multidisciplinarity in the context of health care means that health care providers from different disciplines work together to collaboratively provide diagnoses, assessments, and treatment within their scope of practice and areas of competence. The concept of multidisciplinary treatment fits very well with the traditional provideroriented approach of health care organizations.
In the NIH definition, pulmonary rehabilitation is described as a multidimensional continuum of services, offered by an interdisciplinary team of specialists [3]. Interdisciplinarity refers to an approach to organize intellectual inquiry: interdisciplinarity involves attacking a subject from various angles and methods, eventually cutting across disciplines and forming a new method for understanding the subject. An interdisciplinary approach of pulmonary rehabilitation fits with the global dimension of the individual’s health. Still the patient is the subject, the recipient of the active involvement of the different disciplines [13].
The most optimal model of team organization is probably the transdisciplinary model: team members work across the boundaries of their professional disciplines, with each one sharing responsibility for all areas of patient care. In this model, health care professionals fulfill their responsibilities interchangeably and each team member becomes a pulmonary rehabilitation specialist [14]. The whole team will become involved in realization of the individual goals and the pulmonary rehabilitation setting creates learning and healing environment for each individual.
In order to set up and to organize such patient-centered health care intervention as put forward in all definitions of pulmonary rehabilitation, it will be crucial to consider necessary core competencies applying to all members of the workforce caring for these patients. Competencies are the skills, abilities, knowledge, behaviors, and attitudes that are instrumental in the delivery of desired results, and, consequently of job performance [15]. Core competencies in the management of chronic conditions are part of the WHO report “Preparing a health care workforce for the 21st century [15].” Five core competencies are formulated to complement existing ones for caring patients with chronic conditions. Besides organization of the workforce around the patient, health care providers and pulmonary rehabilitation team members need communication skills that enable them to collaborate with others. Communication skills include the ability to negotiate, share decisions, solve problems collectively, and establish goals, implement action, identify strengths and weaknesses, clarify roles and responsibilities, and evaluate progress [15]. Third, the workforce needs skills to ensure that the safety and quality of patient care are continuously improved. Fourth, the workforce needs skills that assist them in monitoring patients across time. Finally, the workforce needs to consider patient care and the provider’s role in that care from the broadest perspective, multiple levels of the health care system and the care continuum [15]. This continuum of services directed to persons and their families with the goal of achieving and maintaining the individual’s maximum level of independence and functioning in the community was already considered essential in the NIH definition of pulmonary rehabilitation, put forward in 19943.
Partnering skills is considered as a core competency to enhance care coordination and health outcomes. Partnering requires that health care providers transform their core business in terms of relationships, behaviors, processes, communication, and leadership. Partnering takes a collaborative approach to achieve shared objectives. The shared objective of all rehabilitation programs is to return the patient to the highest possible capacity and to contribute to achieve the individual’s maximum level of independence and functioning in the community. Health care providers working in the framework of a pulmonary rehabilitation setting need to develop skills to set up partnerships with the patient and with others. This ability to work both within and across professional disciplines is a key success factor for every rehabilitation structure.
To realize added value for the individual patient, Porter and Teisberg identified that the provider experience, the scale of the offered medical activity, and the learning in medical conditions must be considered as other critical factors to drive success [16]. They describe that the combined effects of experience, scale, and learning create a virtuous cycle in which the value delivered by a provider can improve rapidly. Deeper penetration in a medical condition leads to accumulating experience, rising efficiency, better information, more fully dedicated teams, increasingly tailored facilities, the ability to control more of the care cycle, efficiencies in medical practice, faster innovations, and better results. This whole virtuous cycle is driven by competition on results [16]. The virtuous cycle to offer added value can be facilitated by setting up integrated practice units, focusing on dedicated aspects of the whole rehabilitation program. Crucial for such an organizational approach is the scaling of the rehabilitation programs so that rehabilitation programs can operate at the productivity frontier, relating the quality of health outcomes achieved in addressing pulmonary rehabilitation to the full cost of providing care for that condition. Desirable volumes need to be defined to offer optimal effectiveness and efficiency. Pulmonary rehabilitation programs need to move away from the vicious cycle of fragmentation, subscale services, dependence on less dedicated resources, shared facilities, quality problems, and inefficiency to really compete on value in the management of patients suffering from chronic respiratory conditions [16].
Although these concepts of pulmonary rehabilitation are widely accepted, huge variability exists in content and organizational aspects among pulmonary rehabilitation programs largely the result of local conditions and financial resources [17]. A recent international survey clearly illustrated these large differences among pulmonary rehabilitation programs across continents including the composition of the rehabilitation teams [17]. The survey also illustrated that most programs are small-scale interventions (median 40 to 75 enrolled individuals per program per year) and that most teams consisted of a median of 5 health care professionals: chest physicians, dieticians, nurses and physiotherapists were the most prevalent team members [17]. Even mono-disciplinary and strictly educational programs are still described as “pulmonary rehabilitation” program, completely neglecting the need for individualized assessment of physio- and psychopathological treatable traits in patients with respiratory problems and multidisciplinary intervention.
Pulmonary rehabilitation as personalized medicine treatment has to offer a tailored, patient-centered and individualised intervention covering the multidimensional and heterogeneous aspects affecting patients suffering from a variety of respiratory conditions. Such intervention strategies can be supported by precision medicine interventions and a wide variety of non-pharmacological interventions as ventilator support, non-invasive ventilation or lung volume reduction procedures. This full range of medical expertise, technical skills and specialized facilities will be needed to compete on added value in the management of patients with chronic respiratory conditions. The scientific community must scrutinously ensure that interventions not fulfilling these criteria and not comprehensively addressing identified treatable traits are no longer accepted as pulmonary rehabilitation variants.
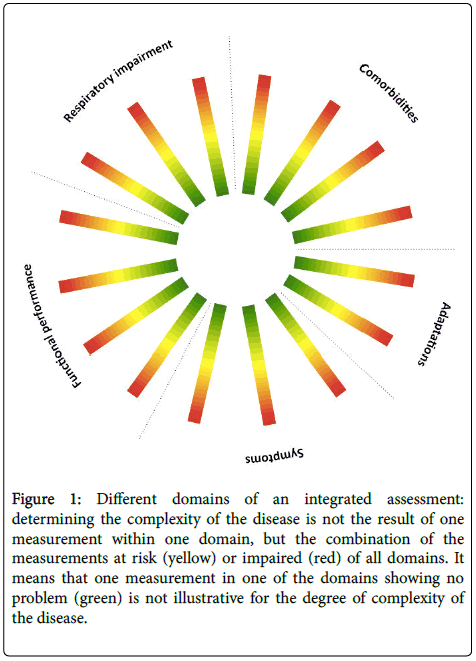
The success of pulmonary rehabilitation is determined, at least in part, by appropriate patient selection and assessment. Identification of treatable traits (Figure 1) and discussion of treatment goals with the patient must form the start of every pulmonary rehabilitation program.
Figure 1: Different domains of an integrated assessment: determining the complexity of the disease is not the result of one measurement within one domain, but the combination of the measurements at risk (yellow) or impaired (red) of all domains. It means that one measurement in one of the domains showing no problem (green) is not illustrative for the degree of complexity of the disease.
Such assessment is part of all definitions of pulmonary rehabilitation [2-5,18].
Ideally, pulmonary rehabilitation must be organized as a flexible, holistic, and integrated intervention, based on partnering of different skills to achieve shared, individualized, patient-related objectives, and to achieve improvement in clinically relevant outcomes and added value to the patient and the community. This requires a process-based organization to manage business around these core processes [19,20].
The sociotechnical systems theory has been developed to design and change organizations in relation to the environmental conditions and strategic choices, and to address the increasing complexity of organizations as a result of increasing external uncertainty and variation within the internal division of labor, as required by offering a tailor-made, individualized program [19,20]. The sociotechnical theory offers a framework to improve efficiency, quality, flexibility and innovation. Indeed, a key feature of sociotechnical design involves bringing together people from different roles and disciplinary backgrounds and with different skills, experience and expertise. Pluralism is the norm, and this implies that they share their views and expertise. They need to educate one another in the opportunities that may exist for the design of a new system, and what they have to offer the design process [19,20].
The holistic approach of pulmonary rehabilitation indeed means organizing around the customer and the need: it has the features of an integrated practice unit (IPU) that treats not only a disease but also the related conditions, complications, and circumstances that commonly occur along with it. In an IPU, personnel regularly work together as a team towards the common goal of maximizing the patient’s overall outcomes as efficiently as possible [16]. The international survey of organizational issues of pulmonary rehabilitation clearly illustrates the complete lack of organizational infrastructure in the majority of programs. Individualization of goals of treatment is completely ignored and replaced by standard health care outcomes as health status, dyspnea and exercise capacity. Performance and process metrics in most programs do not allow any quality control to ensure appropriate standards for pulmonary rehabilitation [17].
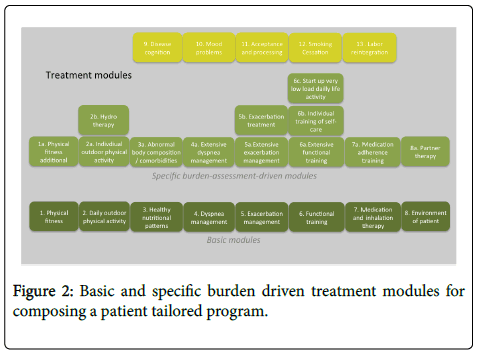
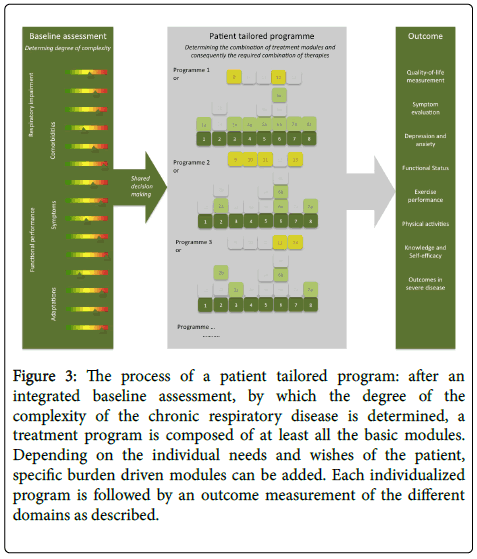
In order to find a balance between individualization of the program and process organization and effectiveness, a modular program structure can be developed consisting a basic modules and step-up interventions based on the level of impairment diagnosed in the baseline assessment procedure. Figure 2 illustrates an example of such patient-tailored program. Each module consists of different interventions in order to achieve the goal of the specific module, which consequently contributes to the outcome and the overall goal of treatment. Every program can be individualized by adding more specific step-up modules to the set of basic modules. Figure 3 depicts the integrated baseline assessment, by which the degree of the complexity of COPD is determined, and the treatment program with its specific modules [21].
Figure 3: The process of a patient tailored program: after an integrated baseline assessment, by which the degree of the complexity of the chronic respiratory disease is determined, a treatment program is composed of at least all the basic modules. Depending on the individual needs and wishes of the patient, specific burden driven modules can be added. Each individualized program is followed by an outcome measurement of the different domains as described.
The final goal of a pulmonary rehabilitation program is to realize an improvement in physical, emotional and social functioning for the individual patient. The duration of the program is an important factor in costs and capacity. The minimum duration of pulmonary rehabilitation has not extensively investigated and most program durations are based on outcomes as exercise training [4,5]. Furthermore, it is generally believed that longer programs yield larger and more endurable training effects [4,5]. The optimum duration of comprehensive pulmonary rehabilitation programs on multidimensional outcome indices needs to be investigated. Principles of value based health care can become very helpful in order to define the balance between outcomes and costs.
The final step in the organization of a pulmonary rehabilitation program is a systematic, multidimensional outcome evaluation in order to allow assessment of realized individual benefits, but also to evaluate population outcomes and to evaluate realized added value for the patient, his environment, the health care system and society [21]. Importantly, pulmonary rehabilitation offers a holistic approach to patients considered as complex adaptive systems: illness and patient behavior cannot be modeled as a simple cause and effect systems [22]. In case of complex adaptive systems, a small change can have a large effect in behavior and outcomes [22-24]. So, the effectiveness of interventions such as pulmonary rehabilitation can be highly dependent on the context in which the program is delivered [22-24]. Furthermore, a multidimensional response outcome needs to be considered to evaluate the efficacy of pulmonary rehabilitation services as responses to regular outcomes are differential within patients with chronic respiratory diseases [25]. Characteristic for complex adaptive systems is the non-linearity in responses and the unpredictability of outcomes [22].
A largely neglected step after pulmonary rehabilitation is the continuation of this partnership between the patient and the health professionals. Indeed, it can be expected that one of the outcomes could be a better and more effective interaction with health care providers by these empowered, more informed and more involved patients [26,27]. Care managers could be a feasible model to organize these services effectively [28].
Conclusion
Pulmonary rehabilitation must offer a holistic, integrated, approach to patients with chronic respiratory diseases to address carefully identified treatable traits. Pulmonary rehabilitation programs need to move away from a supply-driven functional organizational structure towards integrated structures, including the full range of medical expertise, technical skills and specialized facilities needed to compete on added value in the management of patients with chronic respiratory diseases. As an integrated, personalized intervention, pulmonary rehabilitation must be based on partnering of different skills to achieve shared, individualized, patient-related objectives and to achieve improvement in clinically relevant outcomes and added value to the patient and the community. Managing business around the core processes of pulmonary rehabilitation (e.g., intake and assessment, rehabilitative therapies, and outcome evaluation) requires a processbased organization. To maximize the patient’s overall outcomes as efficiently as possible. Organizing pulmonary rehabilitation according to the sociotechnical principles meets the features of such an integrated practice unit to offer a tailor-made, individualized program. Furthermore, to cope with escalating complexity in health care, it is necessary to abandon linear models, accept unpredictability, respect autonomy and creativity, and to respond flexibly to emerging patterns and opportunities. The science of complex adaptive systems provides important concepts and tools for responding to the challenges of health care in the 21st century [22-24].
References
- Vanfleteren LE, Spruit MA, Groenen M, Gaffron S, van Empel VP, et al. (2013) Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 187: 728-735.
- Hodgkin JE, Farrell MJ, Gibson SR, Kanner RE, Kass I, et al. (1981) American Thoracic Society. Medical Section of the American Lung Association. Pulmonary rehabilitation. Am Rev Respir Dis 124: 663-666.
- Fishman AP (1994) Pulmonary rehabilitation research. Am J Respir Crit Care Med 149: 825-833.
- Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, et al. (2006) American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 173: 1390-1413.
- Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, et al. (2013) An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 188: e13-64.
- Lusuardi N, Ambrosino N, Donner C (2005) Definition and rationale for pulmonary rehabilitation. In: Donner C, Ambrosino N, Goldstein R, eds. Pulmonary Rehabiliation 3-8.
- Huber M, Knottnerus JA, Green L, van der Horst H, Jadad AR, et al. (2011) How should we define health? BMJ 343: d4163.
- Agusti A, Bel E, Thomas M, Vogelmeier C, Brusselle G, et al. (2016) Treatable traits: toward precision medicine of chronic airway diseases. Eur Respir J 47: 410-419.
- Spruit MA, Franssen FM, Rutten EP, Wopereis S, Wouters EF, et al. (2016) A new perspective on COPD exacerbations: monitoring impact by measuring physical, psychological and social resilience. Eur Respir J 47: 1024-1027.
- McDonald VM, Higgins I, Wood LG, Gibson PG (2013) Multidimensional assessment and tailored interventions for COPD: respiratory utopia or common sense? Thorax 68: 691-694.
- Grol R, de Maeseneer J, Whitfield M, Mokkink H (1990) Disease-centred versus patient-centred attitudes: comparison of general practitioners in Belgium, Britain and The Netherlands. Fam Pract 7: 100-103.
- Ries A (2005) Guidelines for rehabilitation in the management of chronic obstructive pulmonary disease. In: Donner C, Ambrosino N, Goldstein R, eds. Pulmonary Rehabiliation. Vol Chapter 26. London: Hodder Headline Group 3-8.
- Preparing a healthcare workforce for the 21st century: the challenge of chronic conditions. Chronic Illn 1: 99-100.
- Porter M, Teisberg E (2006) Redefining health. Cambridge: Harvard Business School Press.
- Spruit MA, Pitta F, Garvey C, ZuWallack RL, Roberts CM , et al. (2014) Differences in content and organisational aspects of pulmonary rehabilitation programmes. Eur Respir J 43: 1326-1337.
- Spruit MA, Vanderhoven-Augustin I, Janssen PP, Wouters EF (2008) Integration of pulmonary rehabilitation in COPD. Lancet 371: 12-13
- Clegg CW (2000) Sociotechnical principles for system design. Appl Ergon 31: 463-477.
- van Amelsvoort P (2000) The design of work and organisation: the modern sociotechnical systems approach; an overview of the Dutch sociotechnical systems theory. Vlijmen: ST-GROEP.
- Augustin I, Spruit M, Franssen F, Wouters E (2015) Understanding complexity of chronic non-communicable diseases: an integrated approach for personalized management of patients with COPD. Clin Res Pulm.
- Wilson T, Holt T, Greenhalgh T (2001) Complexity science: complexity and clinical care. BMJ 323: 685-688.
- Plsek PE, Greenhalgh T (2001) Complexity science: The challenge of complexity in health care. BMJ 323: 625-628.
- Plsek PE, Wilson T (2001) Complexity, leadership, and management in healthcare organisations. BMJ 323: 746-749.
- Spruit MA, Augustin IM, Vanfleteren LE, Janssen DJ, Gaffron S, et al. Differential response to pulmonary rehabilitation in COPD: multidimensional profiling. Eur Respir J 46: 1625-1635.
- Bodenheimer T, Lorig K, Holman H, Grumbach K (2002) Patient self-management of chronic disease in primary care. JAMA 288: 2469-2475.
- Wagner EH (1998) Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract 1: 2-4.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 6: 297-305.
Citation: Augustin IML, Wouters EFM (2017) Process of Pulmonary Rehabilitation and Program Organization. J Card Pulm Rehabil 1: 109.
Copyright: © 2017 Augustin IML, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 9723
- [From(publication date): 0-2017 - Aug 17, 2025]
- Breakdown by view type
- HTML page views: 8643
- PDF downloads: 1080