Public Health Hazards Due to Unsafe Drinking Water
Received: 30-Mar-2018 / Accepted Date: 11-May-2018 / Published Date: 18-May-2018
Abstract
A safe and easily accessible potable water supply is essential for good health. About a billion people in developing countries have not had a safe and sustainable water supply for several decades. Water is said to be safe to drink and usable for domestic purposes, when it is free from pathogenic agents, harmful chemical substances, and pleasant to taste. A drinking water quality may be acceptable when it is treated in a treatment plant. Using unsafe drinking or bathing water can impose serious risks to human health. Microbial contamination of groundwater due to sewage outfalls, and agricultural runoff can be a serious threat. Globally, the most commonly occurring diseases transmitted through drinking of unsafe water are infectious hepatitis, cholera, bacillary dysentery, typhoid, paratyphoid, salmonellosis, colibacillosis, giardiasis, cryptosporidiosis, and amoebiasis. Contaminated water may also cause many more bacterial, viral, and parasitic diseases. Majority of the diarrheal deaths occurred worldwide are mainly associated with unsafe water drinking, inadequate sanitation, and poor hygiene. This condition indicated that water supply, and sanitation interventions can play an important role in combating the incidence of waterborne diseases among children. The prevention of waterborne diseases may include improving access to safe water, improving water quality at the source, treating household water and storing it safely, improving access to adequate sanitation facilities, and encouraging good hygiene practices, particularly proper hand washing with antiseptic solution. Water sources, such as household connection, public standpipe, and borehole condition, protected dug well, protected spring, and rainwater collection should be safe and accessible. Regular monitoring of drinking water for various infectious agents should be applied as it will certainly reduce the incidence of waterborne diseases
Keywords: Drinking unsafe water; Hazard; Public health; Waterborne diseases; Water sources
Introduction
According to the WHO definition, improved drinking water sources are sources that are protected from outside contamination, in particular from contamination with fecal matter by nature of its construction or through active intervention [1]. WHO reported about 9.1% of the global burden of disease and 6.3% of all deaths are due to unsafe water, inadequate sanitation, and poor hygiene [2]. Microbial contamination is very common affecting all water source types including piped supplies in many developing countries [3]. It is mentioned that approximately, 780 million people in the world were without access to safe drinking water in 2012 [4]. As the global population is arising from time to time rapidly, availability of water will lowers down steadily, and it is estimated that by 2020 countries, such as India will become a water-stressed nations. According to Millennium Development Goals 2008, 1.6 billion people in the world live in water scarcity, with limited access to water. Within The Millennium Development Goal, the 7th goal indicates about water crisis. Within this goal, there are several specific targets such as the reduction of the percentage of the global population without access to safe water and sanitation by half. It was reported in 2012 that the first few Millennium Development Goals had been met.
Waterborne disease outbreak is said to happen if two or more persons experience a similar illness after consumption or use of water intended for drinking; and epidemiologic evidence showed the water as the source of the illness [5]. Around the globe, around 1.8 billion people use unsafe source of water that is polluted by feces signified by 53% and 35% incidence in Africa and South-East Asia, respectively [3]. It has been estimated that every year, nearly 1 million people die due to waterborne diseases. In addition, around 37.7 million are affected by waterborne diseases, 1.5 million children are estimated to die of diarrhea alone, and 73 million working days are lost due to waterborne disease annually [6]. In countries with low and middle-income, diarrhea-related diseases are the tenth leading causes of death [7]. Unsafe water and poor sanitation cause more than 500,000 infant deaths each year in the Pacific region of Asia [8].
Approximately, 11% of child deaths worldwide are attributed to a diarrheal disease and of these cases, 88% are caused by unsafe water or improper sanitation [9]. Therefore, the quality of drinking water cannot be overlooked when assessing the role of water in public health. A safe, affordable, and easily accessible potable water reserve is vital for a sound health [10]. However, for several decades, about a billion people in developing countries have not had a safe and sustainable water supply. It has been estimated that a minimum of 7.5 liters of water per person per day is required in the home for drinking, preparing food, and personal hygiene, the most basic requirements of water. At least 50 liters of water per person per day is needed to ensure all personal hygiene, food hygiene, domestic cleaning, and laundry needs [11]. To fulfill all these basic requirements and to avoid water stress, about 1,000 cubic meters of freshwater per capita per year is essential [12].
Water is considered ‘safe’ when it is free from pathogenic agents, free from harmful chemical substances, and pleasant to taste, i.e., ideally free from color and odor, and usable for domestic purposes [13]. A drinking water system’s water quality may be acceptable when the water just leaves a treatment plant. However, various physical, chemical, and biological contaminations can happen while the water travels through a distribution system. The most common diseases that can be transmitted through water are diarrheal diseases such as bacillary dysentery, typhoid, paratyphoid, cholera, salmonellosis, colibacillosis, amoebiasis, giardiasis, and cryptosporidiosis. There are many emerging waterborne diseases, such as cryptosporidiosis, cyclosporidiosis, fascioliasis, fasciolopsiasis, and giardiasis, which may also be acquired by food. Contact of the skin or mucous membranes with animal urine contaminated water or bathing in contaminated water (pond, canal, and stream) can result in Leptospira infection in humans [14,15].
Diarrhea alone kills more children than malaria and tuberculosis together worldwide [16]. Hence, water quality is a critical issue to ensure public health. Since water is closely associated with daily human activities, providing safe drinking water is one of the important public health priorities [3]. Adequate access to safe water, improving quality of water source, treating household water, and storing it safely, adequate sanitation facilities, and encouraging good hygiene practices, especially hand washing can prevent waterborne diseases [17]. Recent reports have revealed, however, the evidence based regarding water sanitation system (WSS) interventions, especially with regard to sanitation, is extremely weak [18-20]. Therefore, this review paper is aimed on discussing the implications of consumption, and usage of unsafe water from public health point of view.
Sources of water contamination
There are various environmental factors, such as landscape, weather, and a season that affect the occurrence of foodborne pathogens in water samples. Different irrigation systems in agriculture have been correlated with increased incidence of foodborne infections [21]. In surface waters, Esherichia coli , Listeria monocytogenes , Salmonella are found more frequently in areas where agriculture is practiced along with animal husbandry [22,23]. Listeria monocytogenes was detected from surface water that was in proximity to dairy farm [24].
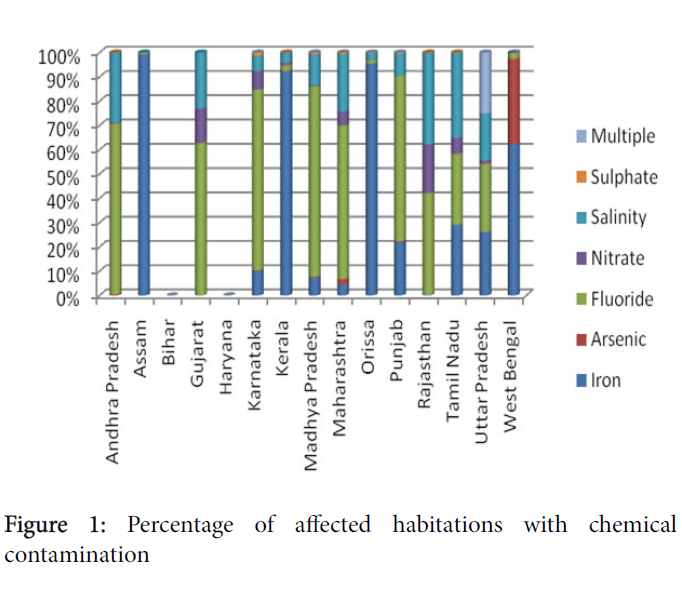
Leakage or seepage in septic tanks or inappropriate sewage treatments results in pollution of groundwater. Bacteria from these sources enter wells that are either open at the land surface or not watertight. When there is any natural disaster, water is the first to be affected. Rodents, insects, animals or plant parts entering the well are other sources of contamination [25]. Wells not having water-tight sheath can be contaminated by bacteria infiltrating to the water through the soil near the well. Human and animal fecal wastes, agricultural products, such as pesticides and fertilizers, improper disposal of chemicals, natural occurring floods, and other disastrous events can contaminate drinking water [26]. These agricultural compounds have degraded the quality of surface water resources by causing nitrate contamination. Heavy metals like cadmium, lead, mercury and zinc are being reported in groundwater in different areas of India [27] (Figure 1).
Drinking water is contaminated with toxic pathogens, and chemicals; at last count over 4,000 chemicals have been found. Wastes from animals and humans, papers, pulp plants, and tanneries are discharged into water bodies, and the organic materials decomposed by using large quantities of oxygen from water. Among the different wastes, human and animal feces are the most common cause of water contamination.
Diarrheal diseases, such as E. coli infection, giardiasis, and typhoid fever are the very common diseases that happen due to using unsafe water [28]. Different groups of individuals with low immunity are more susceptible to waterborne diarrheal diseases [26]. For example, children and infants due to the improperly developed immune system are more vulnerable to pathogen related to water borne diseases, and other toxic contaminants. It is well known that diarrheal disease is one of the leading causes of illness and death in young children in developing countries, especially Bangladesh and most countries of South Asia [29]. Individuals that are more susceptible to diarrheal diseases include cancer patients, HIV/AIDS patients, and transplant patients [28] (Figure 1).
Drinking water can carry a diverse range of pathogens that may be bacteria, viruses, and parasites. Surface and ground water is usually layered by bacteria and viruses; however, parasites/protozoa appear mostly in surface water.
Bacteria
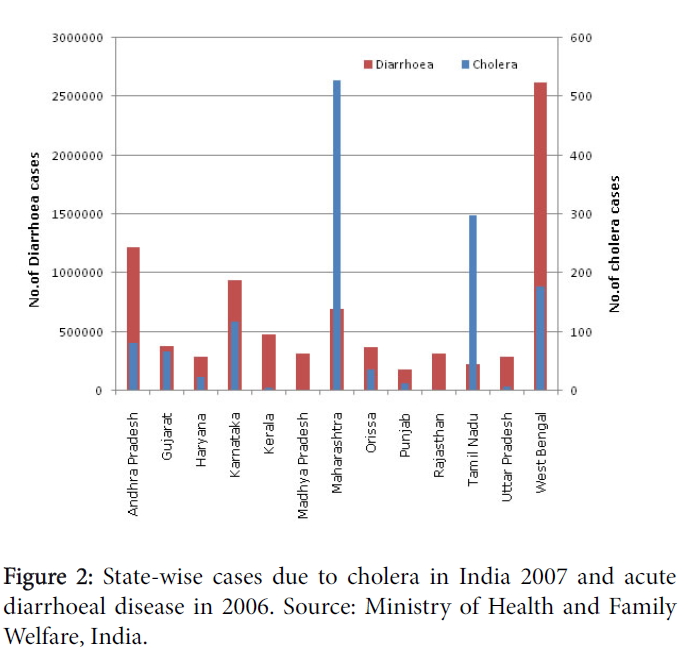
Bacteria can be naturally present in the environment including water bodies and coliforms are among the possibly harmful bacteria that may be present in water. Enterococci and Escherichia coli are commonly present in ocean water as well as fresh recreational water [30]. However, the World Health Organization recommends that water with any amount of fecal coliforms should not be consumed [31]. Fecal indicators that indicate human or animal wastes in water causing cramps, nausea, diarrhea, headaches are Enterococci or coliforms. Sometimes contamination of water due to bacteria causes hemolytic uremic syndrome, a serious kidney disease with potential lifelong complications [32]. Other such bacteria are Vibrio cholerae , Salmonella typhii and several species of Shigella normally causing serious diseases such as cholera, typhoid fever and bacillary dysentery, respectively (Figure 2). Infection with Campylobacter jejuni causes campylobacteriosis with symptoms of abdominal cramps, diarrhea, fever, and pain. Natural water and drinking water distribution systems also contain Mycobacterium avium complex (MAC) [33,34]. The most frequent Mycobacterium species present in potable water and hospital water distribution systems are M. avium, M. chelonae, M. fortuitum, M. gordonae, M. kansasii, and M. xenopi that cause nosocomial infections [35-37]. Using some modern technology, developed nations have largely buried waterborne bacterial pathogens, however, the developing world still trying to end with these public health challenges. Another cyanobacteria Anabaena circinalis living in freshwater reservoirs mainly Australia, Europe, Asia, New Zealand, and North America are the producers of neurotoxins causing respiratory arrest, followed by death. The neurotoxin producing anabaena caused an outbreak in the 1950’s through the drinking water supply causing a series of mass die-offs at cattle farms across the U.S. [38].
Viruses
Viruses are very small organisms that can pass through filters, which retain bacteria. Enteric viruses, such as hepatitis A, polioviruses, Norwalk virus, rotavirus, echoviruses, and coxsackie viruses are excreted in the feces of infected individuals as they harbor them in their intestine, and may contaminate water intended for drinking. Viruses that are excreted in urine like polyoma viruses, and cytomegalovirus can potentially be spread through water [39,40]. Enteric viruses that are transmitted through water infect the gastrointestinal or respiratory tracts and cause diarrhea, fever, hepatitis, paralysis, meningitis in humans [41]. Rotavirus is the leading cause of severe acute diarrhea in children under the age of five, resulting in over half a million deaths annually worldwide [42]. There are many factors responsible for the survival of viruses in water, such as temperature, light, pH, salinity, organic matter, suspended solids or sediments, and air-water interfaces. At low temperatures, hepatitis A, adenoviruses and parvoviruses can survive for a long time [43]. Viral infections are usually self-limiting in healthy individuals but can cause serious effects under immune-compromised conditions. They can cause greater morbidity in children under the age of five, the elderly, immunocompromised people, and pregnant women [44]. In developing countries with large populations, waterborne viral diseases are very likely to occur.
Parasites
Parasites mainly protozoa are among the most common pathogens that can present in environmental samples. They have multistage life cycles, consisting of an active trophozoite stage, and a resistant phase (oocyst or cyst) excreted in feces that are capable of infecting new hosts [45]. Unlike bacteria and viruses, parasites generally have unique features, which often make them remarkably suited for survival in the environment including water. Majority of these parasites are difficult to detect and control in humans. Many of them have the potential to cause severe public health problems, while others are capable of inflicting considerable losses to thelivestock sector [46]. Dracunculiasis, also known as Guinea worm disease, is a preventable infection caused by the parasite Dracunculus medinensis , which is commonly found in water. This helminthic disease is close to being eradicated completely, as there were only 126 cases globally in 2014 with a re-emerging nature in developing countries [47]. This infection affects poor communities in remote parts that do not have access to safe water to drink [48]. As to the reports of WHO, Cryptosporidium parvum oocysts and Giardia lamblia cysts are introduced to waters all over the world by fecal pollution. In developing countries, infection with C. parvum is highly prevalent during the first two years of life, when up to 45% of children experience the disease [49].
Cryptosporidium is considered as a major threat to the US water supply because it is highly infectious, resistant to chlorine, and because of its small size that makes it difficult to filter. The cysts of Giardia have been found on many vegetables, such as coriander, carrots, mint, radishes, and potatoes that were irrigated with untreated wastewater [50,51]. The resistant nature of these parasites permits them to persist in surface waters and makes these microorganisms resistant to normal drinking water chlorination [52]. Free-living amoebae (FLA) of Balamuthia, Naegleria, Sappinia, and Acanthamoeba genus are human pathogens causing encephalitis, keratitis, pneumonitis, and dermatitis [53,54] over the globe, and the infection routes are mostly from the environment. The systems that filter water before presented for consumption may successfully remove many protozoan parasites. In addition to waterborne diseases, there are also water-related diseases that can be transmitted through skin contact with parasites that have a part of their life cycle in water. The typical example is schistosomiasis, a disease caused by a flatworm parasite. Out of parasitic diseases, schistosomiasis is considered to be the second biggest threat to public health after malaria.
Impact on health
Most of the diarrheal diseases commonly occur through oral-fecal or hand-to-mouth transmission, and can be facilitated by water [55]. Other health risks that are caused by chemical contamination of drinking water include skin lesions, vascular, and cardiac problems, and cancer of the bladder, lungs, or skin, liver, and kidney damage, damage to the nervous system, suppression of the immune system, and birth defects [29]. Contamination and pollution of water causes both public health and economic implications. These losses may include human deaths, health expenditures, loss of man-days, and reduction in agricultural output, reduction in fish population etc. River pollution has been quite alarming in recent years as a result of waste discharges from industries, sewage outfall from townships, pilgrimage centers etc. Chemical manufacturing units are the major polluters of the river [56], and health related problems including skin diseases, stomach and intestinal ailments, and bronchial problems. It also affects the livestock based economy.
Water Quality
The quality of drinking water is an influential environmental determinant of health. Quality of water is determined considering three major categories i.e., physical, chemical, and microbiological properties. Physical and chemical properties indicate the presence of heavy metals; some organic compounds, total suspended solids (TSS), and turbidity. Microbiological parameters include coliform bacteria, E. coli , and specific pathogenic species of bacteria (such as choleracausing Vibrio cholerae ), viruses, and protozoan parasites. Most of the time, chemical parameters cause a chronic health risk through the slow and constant accumulation of heavy metals although some components like nitrates/nitrites and arsenic can have a more immediate impact. On the other hand, physical parameters affect the aesthetics and taste of the drinking water, and may complicate the removal of microbial pathogens. As far as drinking water quality is concerned, it is necessary to consider susceptible populations that are more prone to exposures, including children, immune-suppressed individuals, and the old ones. Newborns, for example, are especially at risk for enteroviruses [57].
Contact with unsafe drinking or bathing water can impose serious risks (both acute and delayed) to human health [58]. Water fecal contamination can be determined by checking for the presence of coliform bacteria, a convenient marker for a class of harmful fecal pathogens. If fecal coliforms such as E. coli are found in water, it serves as an indication of contamination by sewage. Further, microbial pathogenic parameters are typical of greatest concern because of their immediate health risk. Generally, the most commonly known contaminant of water sources is human excreta, particularly faecal pathogens, and parasites. In the developing countries, the only sources of water are from small streams often directly contaminated by sewage. Hence, there is a need to have access to clean water in adequate quantity, water purification technology, and accessibility and distribution systems for water.
Treating Drinking Water
Water sources that include household pipesystem, public standpipe, borehole condition, protected dug well, protected spring and rainwater collection should be safe and accessible. The accessibility to safe water should be collateral with improved sanitation facilities such as connection to public sewer, connection to the septic system, or a pit latrine or water seal.
It is pertinent that water intended for drink require a system of treatment before use, even water from deep wells or springs. The treatment procedure mainly depends on the source of the water. The type and amount of water treatment can vary depending on the type of bacteria/viruses present. In difficult situations that compromise conventional treatment systems, waterborne pathogens may be killed or inactivated by boiling [59], but this requires a facility to store boiled water in sterile conditions.
Other techniques like filtration, chemical disinfection, and exposure to ultraviolet radiation have been validated in an array of randomized control trials to appreciably reduce levels of water-borne diseases among users in low-income countries [60], but these also may have some problems, such as absence of required facilities. The most commonly used forms of disinfection technologies include use of ultraviolet light, chlorine, chloramines, and ozone. Since viruses are so small, conventional treatment, including filtration, is ineffective at physically removing viruses. UV technology has been proved to be beneficial and gaining popularity for water treatment. Ozone is also an effective water treatment commonly used to reduce color, taste, and odor.
The routine treatment of water for bacteria/viruses is using chlorine, but this is not common for protozoa, mostly when applied to low turbidity water. Chloramine, a reaction product of chlorine and ammonia, which is less potent than chlorine may be used sometimes to successfully reduce Legionella counts. The efficacy of disinfectants is calculated by concentration (C) in mg/l, as well as time (T) in minutes (CT value,) necessary to attain the desired logs of disinfection under the temperature, and pH conditions. Bacteriophages act as good indicator organism, and their use as virus indicators to monitor human enteric viruses in waters, is applied [43]. Desalination is another type of water treatment that is used mainly in dry areas with access to large bodies of saltwater. However, monitoring for all pathogens still remains impractical [43]. Regardless of the disinfectant applied at a drinking water utility, cross-contamination can occur throughout the water distribution system due to cavitations; therefore, the use of secondary disinfectants in distribution systems is required [44].
Prevention
Any water origin disease outbreak should immediately be notified to healthcare officers. Detection should be done through routine reporting conditions, bacterial isolate sub-typing, and molecular analysis in the laboratory, consumer complaints, and systematic surveillance systems. The procedure might include calling potentially exposed groups, sending alerts, requesting specimens from laboratories, or issuing a media alert. Any type of water based illnesses associated with harmful toxicants, such as algal blooms should also be noted. It is important to mention that epidemiological investigation should be done to identify causes, and to apply preventive measures. Samples should be transported to public health laboratories to confirm an etiologic agent, if necessary [61] and to implement public health measures to prevent further spread. Other simple measures can be taken to prevent contracting the disease, such as wearing gloves and shoes when in contact with water, boiling water that is used to wash dishes and clothes, and discouraging children from swimming in bodies of water [62,63].
Conclusion
Ensuring water quality and safety requires active participation of all stake holders with the medical community. However, the majority of health care professionals have received limited training in the evaluation of waterborne diseases. Lack of safe water to meet daily needs is a reality for many people around the world, and has serious health consequences. The situation is getting worse due to population growth, urbanization, and increased domestic and industrial water use. To overcome the water scarcity and other health issues, research is required in three main areas: increasing efficiency of domestic water use, developing technology for implementing and monitoring safe water reuse, and economic policies to promote effective water conservation. Practicing recycle and reuses strategies for wastewater and solid wastes should be the first option. The main challenge in detection of any waterborne disease outbreak is significant number of people may not consult a doctor so that it goes unnoticed. Globally, there were many waterborne disease outbreaks with several hundred or a thousand people affected, which are discovered more or less accidentally. Moreover, even with a good surveillance system waterborne outbreak detection is difficult. Therefore, Waterborne Disease and Outbreak Surveillance System (WBDOSS) should be established in each country mainly in developing countries. This system collects data on waterborne diseases, and outbreaks associated with recreational water, drinking water, environmental, and undetermined water exposures. Besides, there is a need to develop improved ways for better water treatment, and hygienic handling and management of water.
Acknowledgement
The authors are very grateful to Prof. Dr. R. K. Narayan for going through the manuscript and giving his suggestions. Thanks are also due to Anubha for computer help.
References
- Wright J, Gundry S, Conroy R (2004) Household drinking water in developing countries: a systematic review of microbiological contamination between source and point of use. Trop Med Int Health 9: 106-117.
- Pruss-Ustun A, Bos R, Gore F, Bartram J (2008) Safer water, better health: costs, benefits and sustainability of interventions to protect and pro mote health. World Health Organization, Geneva.
- Bain R, Cronk R, Hossain R, Bonjour S, Onda K, et al. (2014) Global assessment of exposure to faecal contamination through drinking water based on a systematic review. Trop Med Int Health 19: 917-927.
- WHO (2012) Global costs and benefits of drinking-water supply and sanitation interventions to reach the MDG target and universal coverage. World Health Organization, Geneva.
- Levine WC, Stephenson WT, Craun GF (1990) Waterborne disease outbreaks, 1986-1988. Morbidity and Mortality weekly report: CDC Surveillance Summaries 1: 1-3.
- Kumar M, Muckerjee R (2014) Safe drinking water for rural populations in India: An effective service delivery model by Naandi Foundation. Field Actions Science Reports. Special Issue 12.
- Murray DR, Schaller M (2010) Historical prevalence of infectious diseases within 230 geopolitical regions. A tool for investigating origins of culture. J Cross Cult Psychol 41: 99-108.
- Hunter PR, MacDonald AM, Carter RC (2010) Water supply and health. PLoS Med 7: e1000361.
- Howard G, Bartram J (2003) Domestic water quantity, service level and health. World Health Organization, Geneva.
- Rijsberman FR (2006) Water scarcity fact or fiction. Agric Water Manag 80: 5-22.
- Park K (2011) Screening for disease. Park’s textbook of Preventive and Social Medicine (21stedn.). Bhanot Publishers, Jabalpur, India. pp: 116-118.
- Zuthi MF, Biswas M, Bahar MN (2009) Assessment of supply water quality in the Chittagong city of Bangladesh. J Eng Appl Sc 3: 73-80.
- Sikder MT, Kihara Y, Yasuda M, Mihara Y, Tanaka S, et al. (2013) River water pollution in developed and developing countries judge and assessment of physicochemical characteristics and selected dissolved metal concentration. Clean (Weinh) 41: 60-68.
- Rana AKMM (2009) Effect of water, sanitation and hygiene Intervention in reducing self-reported waterborne diseases in rural Bangladesh. Research and Evaluation Division, BRAC Research Report, Bangladesh.
- World Health Organization (2014) Joint Water Supply and Sanitation Monitoring Programme. Progress on drinking water and sanitation 2014 update. WHO, Geneva.
- Pattanayak SK, Dickinson KL, Yang JC, Patil SR, Praharaj P, et al. (2007) Promoting latrine use: Midline findings from a randomized evaluation of a community mobilization campaign in Bhadrak, Orissa, India. RTI Working Paper, Research Triangle Institute.
- Overbey L (2008) The health benefits of water supply and sanitation projects: A review of the World Bank Lending Portfolio (No. 43207). IEG Working Paper 2008/1.
- Waddington H, Snilstveit B, White H, Fewtrell L (2009) Water, sanitation and hygiene interventions to combat childhood diarrhoea in developing countries. International Initiative for Impact Evaluation, New Delhi.
- Steele M, Odumeru J (2004) Irrigation water as source of foodborne pathogens on fruit and vegetables. J Food Prot 67: 2839-2849.
- Edge TA, El-Shaarawi A, Gannon V, Jokinen C, Kent R, et al. (2012) Investigation of an environmental benchmark for waterborne pathogens in agricultural watersheds in Canada. J Environ Qual 41: 21-30.
- Falardeau J, Johnson RP, Pagotto F, Wang S (2017) Occurrence, characterization, and potential predictors of verotoxigenic Escherichia coli, Listeria monocytogenes, and Salmonella in surface water used for produce irrigation in the Lower Mainland of British Columbia, Canada. PloS one 12: e0185437.
- Lyautey E, Lapen DR, Wilkes G, McCleary K, Pagotto F, et al. (2007) Distribution and characteristics of Listeria monocytogenes isolates from surface waters of the South Nation River watershed, Ontario, Canada. Appl Environ Microbiol 73: 5401-5410.
- Skipton S, Jasa PJ, Varner DL, Hay D (1990) G90-989 Drinking Water: Bacteria. Historical Materials from University of Nebraska-Lincoln Extension 1: 1413.
- Herman G, Zaslow S (1996) Health effects of drinking water contaminants. North Carolina Cooperative Extension Service, Publication No HE-393.
- Sahoo NK, Rout C (2012) Ground water: Threats and management in India—A review. International Journal of Geotechnics and Environment 4: 143-152.
- Routledge D, Stewart D (1998) Water: Essential for existence. Explore Magazine 8: 5.
- Parashar UD, Bresee JS, Glass RI (2003) The global burden of diarrhoeal disease in children. Bull World Health Organ 81: 236.
- Haack SK, Fogarty LR, Wright C (2003) Escherichia coli and enterococci at beaches in the Grand Traverse Bay, Lake Michigan: sources, characteristics, and environmental pathways. Environ Sci Technol 37: 3275-3282.
- Ayeni AO (2014) Domestic water source, sanitation and high risk of bacteriological diseases in the urban slum: Case of cholera in Makoko, Lagos, Nigeria. Journal of Environment Pollution and Human Health 2: 12-25.
- Hrudey SE, Walker R (2005) Tragedy could have been prevented. Op Flow 31: 1-4.
- Glover N, Holtzman A, Aronson T, Froman S, Berlin OG, et al. (1994) The isolation and identification of Mycobacterium avium complex (MAC) recovered from Los Angeles potable water, a possible source of infection in AIDS patients. Int J Environ Health Res 4: 63-72.
- Von Reyn CF, Marlow JN, Arbeit RD, Barber TW, Falkinham JO (1994) Persistent colonisation of potable water as a source of Mycobacterium avium infection in AIDS. Lancet. 343: 1137-1141.
- Vaerewijck MJ, Huys G, Palomino JC, Swings J, Portaels F, et al. (2005) Mycobacteria in drinking water distribution systems: ecology and significance for human health. FEMS Microbiol Rev 29: 91-934.
- Genc GE, Richter E, Erturan Z (2013) Isolation of nontuberculous mycobacteria from hospital waters in Turkey. APMIS Supp 1121: 1192-1197.
- Maleki MR, Kafil HS, Harzandi N, Moaddab SR (2017) Identification of nontuberculous mycobacteria isolated from hospital water by sequence analysis of the hsp65 and 16S rRNA genes. J Water Health 15: 766-774.
- Dillenberg HO, Dehnel MK (1959) Toxic waterbloom in Saskatchewan. Can Med Assoc J 83: 1151.
- WHO (2011) Guidelines for drinking-water quality (4th edn.). WHO Press, Geneva, Switzerland.
- Cannon MJ, Hyde TB, Schmid DS (2011) Review of cytomegalovirus shedding in bodily fluids and relevance to congenital cytomegalovirus infection. Rev Med Virol 21: 240-255.
- American Water Works Association (1999) Manual of Water Supply Practices: Waterborne Pathogens (1st edn.). American Water Works Association, Denver.
- WHO (2008) Global networks for surveillance of rotavirus gastroenteritis, 2001-2008. Wkly Epidemiol Rec 83: 421-425.
- Bosch A (1998) Human enteric viruses in the water environment: a minireview. Int Microbiol 1: 191-196.
- Gall AM, Marinas BJ, Lu Y, Shisler JL (2015) Waterborne viruses: a barrier to safe drinking water. PLoS Pathogens 11: e1004867.
- Zarlenga DS, Trout JM (2004) Concentrating, purifying and detecting waterborne parasites. Vet Parasitol 126: 195-217.
- Macpherson CN (2005) Human behaviour and the epidemiology of parasitic zoonoses. Int J Parasitol Parasites 35: 1319-1331.
- Lawrence RJ, Fudge C (2009) Healthy Cities in a global and regional context. Health Promot Int 24: 111-118.
- Valentiner-Branth P, Steinsland H, Fischer TK, Perch M, Scheutz F, et al. (2003) Cohort study of Guinean children: incidence, pathogenicity, conferred protection, and attributable risk for enteropathogens during the first 2 years of life. J Clin Microbiol 41: 4238-4245.
- Thompson RA (2002) Presidential address: rediscovering parasites using molecular tools–towards revising the taxonomy of Echinococcus, Giardia and Cryptosporidium. Int J Parasitol Parasites 32: 493- 496.
- Fayer R, Dubey JP, Lindsay DS (2004) Zoonotic protozoa: from land to sea. Trends Parasitol 20: 531- 536.
- http://www.who.int/water_sanitation_health/GDWQ/Microbiology/Microbioladd/microadd5.htm
- Imam AM (2008) Blindness due to Acanthamoeba: first case report from Sudan. Int J Health Sci 2: 163.
- Walia R, Montoya JG, Visvesvera GS, Booton GC, Doyle RL, et al. (2007) A case of successful treatment of cutaneous Acanthamoeba infection in a lung transplant recipient. Transpl Infect Dis 9: 51-54.
- Zhang J (2012) The impact of water quality on health: Evidence from the drinking water infrastructure program in rural China. J Health Econ 31: 122-134.
- Mudrakartha S, Sheth J, Srinath J (2006) Unclogging the khari river: Stakeholders come together to halt pollution. Econ Polit Wkly 18: 587-590.
- Abzug MJ, Keyserling HL, Lee ML, Levin MJ, Rotbart HA, et al. (1995) Neonatal enterovirus infection: virology, serology, and effects of intravenous immune globulin. Clin Infect Dis 20: 1201-1206.
- Dwight RH, Fernandez LM, Baker DB, Semenza JC, Olson BH, et al. (2005) Estimating the economic burden from illnesses associated with recreational coastal water pollution—a case study in Orange county, California. J Environ Manage 76: 95-103.
- Clasen T, Schmidt WP, Rabie T, Roberts I, Cairncross S, et al. (2007) Interventions to improve water quality for preventing diarrhoea: systematic review and meta-analysis. Br Med JÂ 334: 782.
- Pal M, Anberber M (2014) Monograph on microbiology of drinking water. LAP LAMBERT Academic Publishers, Saarbruchen, Germany.
- Oluwasogo OA, Fagbemi OB (2013) Prevalence and risk factors of Schistosoma haematobium infections among primary school children in Igbokuta Village, Ikorodu North Local Government, Lagos State. J Nurs Health Sci 2: 62-68.
- Pal M, Hadush A (2017) Leptospirosis: An infectious emerging waterborne zoonosis of global significance. Air Water Borne Dis 6: 1-4.
Citation: Pal M, Ayele Y, Hadush M, Panigrahi S, Jadhav VJ (2018) Public Health Hazards Due to Unsafe Drinking Water. Air Water Borne Dis 7: 138.
Copyright: © 2018 Pal M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 21513
- [From(publication date): 0-2018 - Nov 21, 2025]
- Breakdown by view type
- HTML page views: 20112
- PDF downloads: 1401