Referral to Cardiac Rehabilitation among Rural Heart Failure Patients
Received: 04-Oct-2017 / Accepted Date: 18-Oct-2017 / Published Date: 23-Oct-2017
Abstract
Purpose: Determine how rural heart failure patients are referred for outpatient cardiac rehabilitation. This study examined individual and system challenges to cardiac rehabilitation referral.
Methods: This was a prospective study from a single site tertiary care hospital. The primary outcome was to determine how study subjects were referred to cardiac rehabilitation. A secondary outcome was the elicited individual characteristic differences among subjects.
Findings: Sixty-one patients were included in the study, 43 males and 18 females (67 ± 9.37 y). There was a statistically significant difference in who initiated the referral to cardiac rehabilitation depending upon diagnosis code (p<0.001). If CAD or heart surgery was the diagnosis code utilized, mid-level providers initiated the referral; however, if heart failure was the primary, cardiac rehabilitation staff initiated the referral. Secondary findings demonstrated not all heart failure patients were managed by cardiologists, low socioeconomic status, and illiteracy.
Conclusions: A multidisciplinary approach is warranted, especially inpatient cardiac rehabilitation staff, to ensure referral to outpatient cardiac rehabilitation among rural heart failure patients.
Keywords: Health disparities; Health services research; Geography
Abbreviations
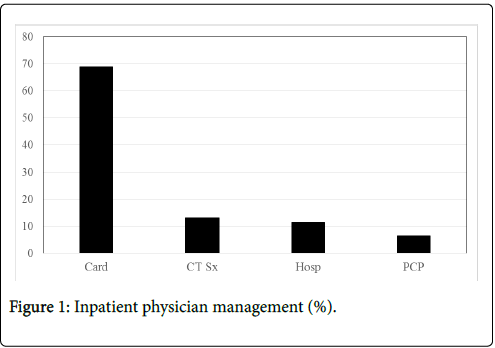
Card: Cardiologist; CT Sx: Cardiothoracic Surgery; Hosp: Hospitalist; PCP; Primary Care Physician
Introduction and Statement of Purpose
Heart failure (HF) is currently the leading discharge diagnosis among adults over the age of 65 [1]. Further, the prevalence of HF is projected to increase by 46% by 2030 [2] given the current numbers and projected increases in HF, cardiac rehabilitation utilization should follow suit. The HF ACTION Trial was paramount in the approval of cardiac rehabilitation (CR) in Medicare and Medicaid patients [3]. After the approval notice, CR professionals were concerned with what to do with the large influx of patients into their programs [4]. Unfortunately, the large influx in participation has not come to fruition.
In a recent analysis of a national registry, HF patients are referred to CR 10% of the time [5]. Possible reasoning for low referral to outpatient cardiac rehabilitation could be use of other diagnosis codes (e.g., heart surgery, percutaneous intervention, or myocardial infarction) [5]; patient management, practitioner may not be aware of the benefits of CR [6,7] socioeconomic and insurance status, reduced income and lack of insurance may lead to fewer healthcare services offered [8] or inpatient cardiac rehabilitation staff, staff could be uncomfortable getting orders for HF patients [4]. Rural patients may be at a further disadvantage as they are less likely to be referred for CR [9].
The purpose of this study was to determine how rural HF patients are referred to outpatient CR. To determine how patients were referred, their referral diagnosis code, what entity initiated the referral (e.g., nurse, mid-level provider, CR staff, or physician), and physician management were tracked. The intention for tracking diagnosis code for referral and initiation of the order was to determine if there was a different impetus for a given diagnosis code– i.e. a system issue. To this point, this was the first study focused solely upon rural heart failure patients and their respective referral process into outpatient CR services.
Methods
The primary outcome of the study was how the referral for CR was acquired. A secondary outcome was to determine sociodemographic and clinical characteristics of the rural HF sample. The following variables were collected on subjects: age, gender, socioeconomic status (household income), race, ability to read, insurance status, inpatient management, outpatient CR order initiation, outpatient CR order diagnosis, and distance to CR. Ability to read was determined by the subject asking the researcher to read materials due to their inability to read.
Human subjects and institutional review board
All methodologies were approved by Southern Illinois University Carbondale’s Human Subjects Committee. Further, the methodology was also approved by Southern Illinois Healthcare Intuitional Review Board. In order to locate appropriate HF patients eligible for the study, the researcher worked with inpatient CR staff to determine what patients had an ejection fraction of less than or equal to 35%. Consent was obtained via discussion and consent authorization form with potential subjects while hospitalized. Special attention was taken to ensure potential subjects were made aware their participation or nonparticipation would not have any impact on their current or future healthcare. All hard copy survey materials were kept in a locked office and locked file cabinet. Survey answers were transferred, by the primary researcher, into a password protected Microsoft Excel® document.
Subjects
Data were collected prospectively from hospitalized systolic HF patients that met the criteria for outpatient CR services by Medicare guidelines; stable heart failure with an ejection fraction of less than or equal to 35%, New York Heart Association class II to IV symptoms, despite being on optimal therapy for at least six weeks [10]. Exclusion criteria for participation in the study were cognitive deficits, institutionalized, or undergoing dialysis. Sixty-one subjects were enrolled into the study over a 3-month period.
Statistical analysis
Frequencies and descriptive statistics were used for all variables. A chi-square test (2 × 3) was performed on outpatient CR order initiation and outpatient CR order diagnosis variables with an alpha of 0.05 to determine significance. CR order initiation was coded into two levels, mid-level provider (i.e., physician assistant or nurse practitioner) and cardiac rehabilitation staff (i.e., exercise physiologist). CR order diagnosis was coded into three levels; systolic heart failure, coronary artery disease (e.g., myocardial infarction, percutaneous intervention, or stable angina), and heart surgery (e.g., coronary artery bypass grafting, aortic valve replacement, and/or mitral valve replacement); however, all subjects had systolic heart failure defined as an ejection fraction less than or equal to 35%. All data were analyzed using Statistical Package for the Social Sciences (SPSS Version 25; IBM Corp., Armonk, New York).
Results
Socioeconomic, demographic, and clinical characteristics are located (Table 1). Physician management is located (Figure 1). Descriptive sociodemographic and clinical data found subjects were mostly Caucasian males of Medicare age and managed by various physicians. To determine differences between primary diagnosis code for CR and CR order initiation, a chi-square statistic was conducted. CR order initiation was significantly different depending upon diagnosis code (χ2=29.73, df=2, N=61, P<0.001). A primary diagnosis of HF was mostly initiated by CR staff; conversely, a primary diagnosis of CAD and heart surgery was mostly initiated by mid-level providers (Table 2).
| All Subjects (n=61) | |
|---|---|
| Gender | |
| Male | 43 (70.5%) |
| Female | 18 (29.5%) |
| Age, y | 67 ± 9.37 |
| Race | |
| Caucasian | 47 (67.1%) |
| African American | 14 (22.9%) |
| SES, No. below poverty line | 17 (27.9%) |
| Distance to CR, miles | 11.97 ± 10.32 |
| Illiterate | 15 (24.6%) |
| Insurance status | |
| Medicare | 37 (60.7%) |
| Medicaid | 12 (19.6%) |
| Private | 12 (19.6%) |
| Inpatient management | |
| Cardiologist | 42 (68.9%) |
| CT surgery | 8 (13.1%) |
| Hospitalist | 7 (11.5%) |
| Primary care | 4 (6.5%) |
| OP CR diagnosis | |
| HF | 38 (63.3%) |
| CAD | 16 (26.7%) |
| Heart surgery | 6 (10.0%) |
| CR order initiation | |
| CR staff | 39 (63.9%) |
| PA/NP | 22 (36.1%) |
SES: Socioeconomic status; CR: Cardiac rehabilitation; CT: Cardiothoracic; OP: Outpatient; HF: Heart failure; CAD: Coronary artery disease; PA: Physician assistant; NP: Nurse practitioner.
Table 1: Subject characteristics.
| CR order initiation | HF (%) | CAD (%) | Heart surgery (%) |
|---|---|---|---|
| NP/PA | 3 (7.7%) | 13 (81.3%) | 3 (50%) |
| EP | 36 (92.3%) | 3 (18.8%) | 3 (50%) |
CR: Cardiac rehabilitation; HF: Heart failure; CAD: Coronary artery disease; NP: Nurse practitioner; PA: Physician assistant; EP: Exercise physiologist.
Table 2: Chi-Square Test Results (2 × 3).
Discussion
All of the subjects had a diagnosis of systolic HF; however, diagnosis codes used for entry into CR were varied. Two incidental findings were nearly one third of subjects were below the poverty line, and nearly one fourth of the subjects required the primary researcher to read materials to them due to their inability to read.
The results of the present study allude to the importance of inpatient CR staff as the gatekeepers to outpatient CR services for rural HF patients. An inherent challenge for HF patients was the varied physician management. CR orders have historically been ordered by cardiologists, but in the present study, not all HF patients were managed by a cardiologist–corroborating the notion that practitioners may not be aware of the benefits of cardiac rehabilitation [6,7]. A possible concern, specifically for hospital physicians (e.g., hospitalist), would be the lack of follow up as an outpatient. Since the hospital physician does not follow the patient outside of the hospital, perhaps there is a lack of comfort in ordering outpatient services. Further, as suggested by Golwala et al. [5] HF patients could be referred to CR under varying diagnoses. It is imperative to note all subjects in the current study have a diagnosis of systolic HF; however, there is a high likelihood of concomitant conditions or procedure codes from which to select. As an example, if a patient presented with an acute myocardial infarction (MI), had a percutaneous coronary intervention (PCI), and has systolic HF sequelae–the practitioner has a choice of which diagnosis code to attach to the CR order. Logically, selecting the MI/PCI would be the best as there is no wait period like in HF.
Referral to CR among rural HF patients is a complex endeavor. Locating appropriate patients can be challenging–thus, inpatient CR staff is pivotal for finding patients. A secondary issue is acquiring an order from practitioners. HF patients were not always managed by a cardiologist; therefore, other practitioners will need to be educated on the importance of CR on the management of HF patients. The best education to provide is simply stating exercise in stage C HF patients is a class 1 recommendation now–the same class recommendation as an evidence based beta blocker [11] Another concern brought to light by the present study is just how complex, logistically, rural HF patients may be. Patients may have barriers to CR and general care due to lack of money, underinsured, and/or the inability to read. A multidisciplinary approach to care is the best way to overcome barriers for patients with intrapersonal issues. Education by CR staff should be in terms patients can understand, further, providing images may aid in an understanding of material. Case managers and social workers should be used in instances where patients require assistance.
The study has some limitations that must be addressed. First, the study was performed at a single site. To further produce generalizability, studies of multisite locations are recommended. A secondary limitation is the current study took place in hospitalized HF patients only. Since HF patients are managed by other physicians, studies addressing the use of primary care and outpatient HF services are warranted.
References
- Page RL, O’Bryant CL, Cheng D, Dow TJ, Ky B, et al. (2016) Drugs that may cause or exacerbate heart failure. Circulation 134: 1-38.
- Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, et al. (2013) Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ Heart Fail 6: 606-619.
- O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, et al. (2009) Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 301: 1439-1451.
- Keteyian SJ, Squires RW, Ades PA, Thomas RJ (2014) Incorporating patients with chronic heart failure into outpatient cardiac rehabilitation: Practical recommendations for exercise and self-care counseling–a clinical review. J Cardiopulm Rehabil Prev 34: 223-232.
- Golwala H, Pandey A, Ju C, Butler J, Yancy C, et al. (2015) Temporal trends and factors associated with cardiac rehabilitation referral among patients hospitalized with heart failure. Findings from get with the guidelines – heart failure registry. J Am Coll Cardiol 66: 917-926.
- Aragam KG, Dai D, Neely ML, Bhatt DL, Roe MT, et al. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol 65: 2080-2088.
- Riley J (2014) Practical issues in acute heart failure management. Br J Card Nurs 9: 18-23.
- Dracup K, Moser DK, Pelter MM, Nesbitt TS, Southard J, et al. (2014) Randomized, controlled trial to improve self-care in patients with heart failure living in rural areas. Circulation 130: 256-264.
- Brual J, Gravely-Witte S, Suskin N (2010) Drive time to cardiac rehabilitation: At what point does it affect utilization? Int J Health Geogr 9: 1-11.
- Centers for Medicare and Medicaid Services. Decision memo for cardiac rehabilitation (CR) programs – chronic heart failure (Memo No. CAG-00437N).
- Yancey CW, Jessup M, Bozkurt B (2013) ACCF/AHA guidelines for the management of heart failure: Executive summary: A report from the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. JACC 62: 1495-1539.
Citation: Beck A (2017) Referral to Cardiac Rehabilitation among Rural Heart Failure Patients. J Card Pulm Rehabil 1: 115.
Copyright: © 2017 Beck A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 5025
- [From(publication date): 0-2017 - Nov 19, 2025]
- Breakdown by view type
- HTML page views: 4041
- PDF downloads: 984