Sub-acute Care Unit for Elderly Patients as an Alternative Model to Acute Conventional Hospitalization: An Experience in a Geriatric Center of the Camp de Tarragona
Received: 21-Feb-2015 / Accepted Date: 30-Mar-2015 / Published Date: 02-Apr-2015 DOI: 10.4172/2161-1165.S1-003
Abstract
Objective: To explore if direct admission from the emergency department to Sub-acute Care Unit of elderly adults with reactivated chronic diseases might be an alternative clinical pathway to conventional acute hospitalization.
Methods: A retrospective cohort study that examined geriatric patients aged 65 or over transferred directly from the emergency department to the Sub-acute Care Unit of the Hospital Sociosanitario Francolí in the initial 3-year period of implementation, from 1 January 2011 to 31 December 2013. We examined the sociodemographics characteristics, main medical di agnoses, and outcomes at discharge elaborated by Chronic Care Programme within the new Health Plan for Catalonia 2011-2015.
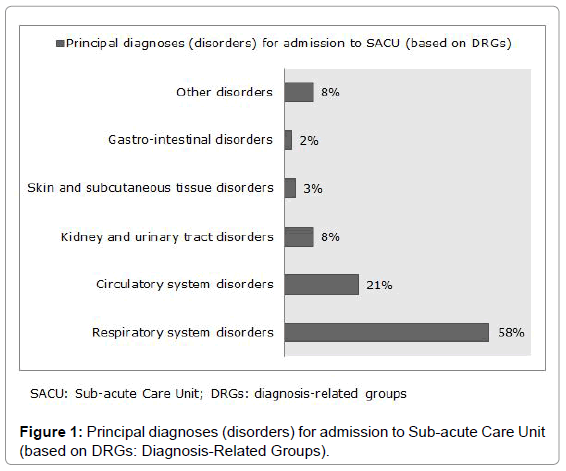
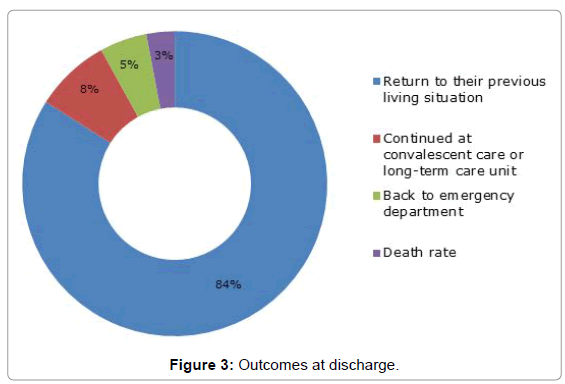
Results: We included 689 patients who were discharged to the Sub-acute Care Unit during the time period of the study. Mean age ± standard desviation=81.5 ± 8.5 years, 52% were women. The principal diagnoses for admission were respiratory system disorders (58%) and circulatory system disorders (21%). Global mean sub-acute length of stay was 16.3 days. All predefined quality standards were met in terms of outcomes at discharge, with among 80% were return to their own home.
Conclusion: From our results, direct admission to sub-acute care unit might represent a potential alternative to acute hospitalization for selected elderly patients.
Keywords: Chronic care programme; Chronic diseases; Elderly patients; Emergency; Sub-acute care
167026Introduction
The prevalence and incidence of chronic diseases (CD) in presentday society is very high. In Catalonia, the majority of morbidity/ mortality cases are due to chronic health problems [1,2]. In 2009, circulatory system diseases, tumors, respiratory system diseases, nervous system diseases and mental disorders accounted for 78% of deaths [1,2]. Moreover, the impact of CD is also very high in terms of the health system resources consumes [1,2]. It is estimated that more than 50% of resources are allocated to the treatment of CD or acute care episodes associated with them [1,2]. Therefore it is necessary to make changes to the healthcare model in order to better response to chronicity.
It has been introduced a new Chronic Care Program within the new Health Plan for Catalonia (CCPHPC) 2011-2015 [3]. Substituting acute conventional hospitalizations by alternatives, such as sub-acute facilities, is one of the main important instruments elaborated by CCPHPC for complex chronic patients (CCP) [3]. Sub-acute Care Unit (SACU) is comprehensive in patient care designed for someone who has an acute illness or exacerbation of a chronic disease process.
The SACU was established in the Hospital Sociosanitario Francolí (HSSF) (Tarragona, Catalonia, Spain) in January 2011. It is goaloriented treatment rendered instead of acute hospitalization in the University Hospital Joan XXIII of Tarragona (HJXXIII), to treat one or more active complex medical conditions, in the context of a person´s underlying long-term conditions and overall situation. The HSSF is a geriatric center with a capacity of 156 beds (for convalescent, palliative and long-term care program). The SACU was established as a separate unit with a capacity of 15-beds licensed by the Department of Health of Catalonia.
The study thus aims to examine the clinical impact and to evaluate the fulfillment of quality standards of sub-acute model care elaborated by CCPHPC after the implementation of SACU in our center.
Methods
Design and setting
This was a retrospective cohort study that examined geriatric patients transferred directly from the Emergency Department (ED) of the reference acute hospital of Tarragona HJXXIII to the SACU of our geriatric center HSSF in the initial 3-year period of implementation, from 1 January 2011 to 31 December 2013.
Inclusion criteria
Patients were carefully selected for transfer to the SACU after fulfilling the inclusion criteria: patients aged 65 years or over, clearly diagnosed, who were considered medically stable, that requires medical treatment a few days for exacerbation or decompensation of any chronic illness, who were considered independent or relatively independent (eating, dressing, personal hygiene, and mobility), that requires no complex additional tests, and necessary of social support to return to the habitual residence after overcoming the acute disease.
Predefined quality standards
We evaluated the compliance with predefined quality standards elaborated by CCPHPC: mean sub-acute length of stay (LOS)<12 days, and outcomes at discharge: return to their previous living situation (home) > 70%, continue at convalescent or long-term care unit of our center <15%, back ED of acute hospital < 10%, and death rate < 10%.
Measurements
We examined the socio-demographics characteristics, main medical diagnoses and outcomes at discharge of patients admitted at SACU in this period.
Statistical analysis
We obtained data from medical records. Statistical analysis was performed on SPSS 15.0 statistical program for windows (SPSS, Chicago, IL, USA).
Results
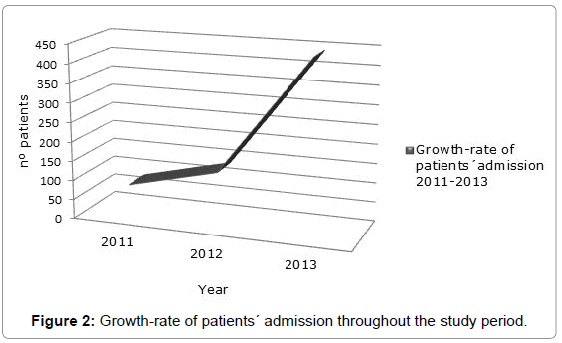
We included 689 patients who were discharged from the ED to the SACU during the time period between 1st Jan 2011 to 31st Dec 2013. Mean age ± standard deviation=81.5 ± 8.5 years, 52% were women. We admitted 80, 137, and 443 patients in 2011, 2012, and 2013 respectively.
The main categories of reasons (principal diagnoses) for these patients’ admission to the SACU, based on diagnosis-related groups (DRGs), included disorders of: respiratory system (58%), circulatory system (21%), kidney and urinary tract (8%), skin and subcutaneous tissue (3%), gastro-intestinal (2%), and others disorders (8%). Four hundred eighty-three patients (70%) had up to 4 co-morbidities (additional diagnoses). Figures 1 and 2 shows the principal diagnoses of patients at admission.
Global mean sub-acute length of stay (LOS) was 16.3 days (19, 18, and 12 days in 2011, 2012, and 2013 respectively).
Five hundred seventy-nine patients (84%) were discharged to their previous living situation (own home), 55 (8%) continued at convalescent care or long-term care of our geriatric center, 34 (5%) back to ED of acute hospital, and 20 (3%) died. All predefined quality standards elaborated by CCPHPC were met in terms of outcomes at discharge (Table 1). The statistics of the patients’ conditions can be observed from Figure 3.
| Predefined quality standards elaborated by CCPHPC | Forecast of predefined quality standards elaborated by CCPHPC | Compliance with predefined quality standards elaborated by CCPHPC | |
|---|---|---|---|
| Mean sub-acute LOS | < 12 days | 2011 | 19 days |
| 2012 | 18 days | ||
| 2013 | 12 days | ||
| Return to their previous living situation (own home) | > 80% | 84% | |
| Continued at convalescent care or long-term care unit of our center | < 15% | 8% | |
| Return to emergency ward of acute hospital | < 10% | 5% | |
| Deathrate | < 10% | 3% | |
CCPHPC: Chronic Care Program within the Health Plan for Catalonia; LOS: Length of Stay
Table 1: Predefined quality standards elaborated by CCPHPC, forecast and compliance.
Discussion
In Catalonia we are facing new challenges with a deep ageing process of population comparing with other European countries. Nowadays, we have 17% and 4.4% population over 65 and 80 years old [1,2]. In 2050 over 30% and 12% population will be over 65 and 80 years old respectively [1,2]. As a consequence an increasing number of people with CD will increase very intensively. Therefore it is necessary to create SACU dedicated to provide appropriate interventions to avoid unnecessary and frequent hospitalizations. SACU is a relativelynew and rapidly-growing medical care service in the early 1980s. The definition of this model has been developed by the American Health Care Association (AHCA), the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), and the Association of Hospital- Based Skilled Nursing Facilities [4]. It is generally more intensive than traditional nursing facility care and less intensive than acute care [4]. Subacutecare patients are more younger, have less cognitive impairment, and have a better rehabilitation potential and more favorable functional outcome, compared with nursing home patients [4,5].
We described a sub-acute model of geriatric care based on the HSSF experience. To our knowledge, this is the most extensive series of sub-acute care for elderly patients reported in literature. The profile of our patients in the presente study was predominantly octogenarians and polypathological, with slightly high prevalence of the female sex. Among 70% of patients, the main diagnoses at admission were exacerbation of chronic obstructive pulmonary disease, followed by decompensation of chronic heart failure. Others disorders, in frequency order, were urinary tract infection, cellulitis, acute gastro-enteritis, and fluid and electrolyte disturbances. We observed a marked growth-rate of patients´ admission throughout the study period, especially in 2013. Our SACU fulfilled the predefined quality standards elaborated by CCPHPC in terms of outcomes at discharge. We demonstrated that the majority of them could be discharged back into the community. Global mean sub-acute LOS was higher than the predefined by CCPHPC. However, we observed gradual decrease of the LOS over the years of the study, probably because patients were more carefully selected. Our results were similar to those previously reported [6,7].
In summary, the results of our study suggest that the model of sub-acute care for older people (≥65 years), independent or relatively independent, with stable and clearly diagnosed medical disorders (reactivated chronic diseases) can play an important role in care of the frail elderly, leads to a higher probability of living at home after discharge y and can avoid unplanned acute hospital admission [6,7].
The limitations of this study are mainly due to the type of retrospective study and to the lack of: scale to identify patients at risk of negative health outcomes, data about readmission after discharge, and cost-utility analyses. Therefore, tools are required to identify highrisk elderly people in ED. Identification of Seniors at Risk (ISAR) is a short self-report questionnaire that can be systematically employed and quickly identify elderly patients in the ED at increased risk of several adverse health outcomes (death, unplanned readmission) and those with current disability, that can increase their LOS (Table 2) [8]. ISAR is a user-friendly score and one of the best-validated screening tools in clinical decision-making [6]. Patients with a score of 2 or more on the ISAR are more likely at risk of negative health outcomes [8]. Regarding patients´ readmission, we aim at determining incidence and risk factors for readmission during the first 30 days after discharge to home. This identification of risk factors (lack of self-management among older people, socio-economic deprivation, lack of integration of primary and social care, etc.) might be relevant to design strategies (multidisciplinary therapy and tele-monitoring for frail older, hospital at home, increase continuity of primary care, etc.) to reduce avoidable hospital readmission [9]. Nowadays, our main objective is to admit patients directly from primary health care teams to avoid acute hospital readmission. In our study, this model of care allowed the patient to spend 16.3 (mean) patient bed-days in the SACU, hence allowing the acute care beds to be used for emergency cases. However, detailed cost-effectiveness or cost-utility analyses is required to evaluate more completely this model of care, given the complexity of needs of the frail elderly persons in a complex healthcare system [7,10,11].
| Question | Answer | Score |
|---|---|---|
| 1. Before the illness or injury that brought you to the Emergency, did you need someone to help you on a regular basis ? | Yes | 1 |
| No | 0 | |
| 2. Since the illness or injury that brought you to the Emergency, have you needed more help than usual to takecare of yourself ? | Yes | 1 |
| No | 0 | |
| 3. Have you been hospitalized for one or more nights during the past 6 months (excluding a stay in the Emergency Department) ? | Yes | 1 |
| No | 0 | |
| 4. In general, do you see well ? | Yes | 1 |
| No | 0 | |
| 5. In general, do you have serious problems with your memory ? | Yes | 1 |
| No | 0 | |
| 6. Do you take more than three different medication everyday ? | Yes | 1 |
| No | 0 |
Patients with a score of 2 or more on the ISAR are more likely at risk of negative health outcomes.
Table 2: Identification of Seniors at Risk (ISAR) questionnaire.
Finally, a true SACU provider should focus on training patients to achieve their highest level of independence as quickly as possible. Doctors, nurses, physical therapists, and other health professionals (pharmacists, psychologists, nutritionists and social workers) should all work in concert with the patient and his or her families to assure the most affordable and efficient care for the patient [12].
References
- Peiró S, Artells JJ, Meneu R (2011) Identification and prioritization of interventions to improve efficiency in the National Health System. GacSanit 2011; 25(2): 95-105
- Estrategiapara el abordaje de la cronicidad en el sistemanacional de salud (2012)Ministerio de Sanidad, ServiciosSociales e Igualdad. Madrid.
- Health plan for Catalonia. 2012 Government of Catalonia, Ministry pf Health. Barcelona 2012.
- Mistry PR (1999) Sandhu S, Hopkins M. Subacute care: which patients benefit? Cleve Clin J Med 66:443-446
- RodrÃguez C, Kergoat MJ, Latour J, et al. (2003) Admission criteria in short-term geriatric assessment units: a Delphi study. Can J Public Health 94: 310-314.
- Garasen H, Windspoll R, Johnsen R (2007) Intermediate care at a community hospital as an alternative to prolonged general hospital care for elderly patients: a randomised controlled trial. BMC Public Health 7: 68–77.
- Inzitari M, Espinosa Serralta L, Pérez Bocanegra MC, et al. Intermediate hospital care for subacute elderly patients as an alternative to prolonged acute hospitalization. GacSanit 2012; 26(2): 166-9
- McCusker J, Verdon J, Tousignant P, et al. (2001) Rapid emergency department intervention for older people reduces risk of functional decline: results of a multicenter randomized trial. J Am GeriatrSoc 49: 1272-81.
- Purdy S. (2010) Avoiding hospital admissions what does the research evidence say? 2010 The King´s Fund. London.
- Rubenstein LZ, Josephson KR, Wieland GD, et al. (1984) Effectiveness of a geriatric evaluation unit. A randomized clinical trial. N Engl J Med 311: 1664-1670.
- Chong MS, Empensando EF, Ding YY, et al. (2012) Asubacute model of geriatric care for frail older persons: the Tan Tock Seng Hospital experience. Ann Acad Med Singapore 41: 354-61
- Beswick AD, Rees K, Dieppe P, et al. (2008) Complex interventions to improve physical function and maintain independent living in elderly people: a systematic review and meta-analysis. Lancet 371: 725–735
Citation: Qanneta R, Moltó-Llarena E (2015) Sub-acute Care Unit for Elderly Patients as an Alternative Model to Acute Conventional Hospitalization: An Experience in a Geriatric Center of the Camp de Tarragona. Epidemiology S1:003. DOI: 10.4172/2161-1165.S1-003
Copyright: © 2015 Qanneta R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14868
- [From(publication date): 0-2015 - Aug 15, 2025]
- Breakdown by view type
- HTML page views: 10256
- PDF downloads: 4612