Case Report Open Access
Submucosal Lipiodol Injection to Guide Radiotherapy for Esophageal Cancer
Han Yao, Christian Boukaram and George Rakovich*George Rakovich, thoracic surgery, University of montreal, Canada
- *Corresponding Author:
- George Rakovich
thoracic surgery
University of montreal, Canada
Tel: 1-514-252-3400
E-mail: george.rakovich@umontreal.ca
Received date: July 30, 2014; Accepted date: October 17, 2014; Published date: October 24, 2014
Citation: Yao H, Boukaram C, Rakovich G (2014) Submucosal Lipiodol Injection to Guide Radiotherapy for Esophageal Cancer. J Gastroint Dig Syst 4:230. doi:10.4172/2161-069X.1000230
Copyright: © 2014 Yao H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Radiotherapy for esophageal cancer relies on cross-sectional imaging to identify the entire extent of tumor. Rarely, the exact limits of the tumor may be radiologically occult. Lipiodol is a contrast agent which has been used successfully to mark cancers of the bladder and lung for radiotherapy and surgical resection. We report a patient with an adenocarcinoma of the gastroesophageal junction with tiny tumor implants extending proximally along the length of the esophagus, which were not visible on standard cross-sectional imaging studies. The proximal extent of implants was marked endoscopically using a submucosal injection of lipiodol, and this provided for adequate planning and successful delivery of radiotherapy.
Abstract
Radiotherapy for esophageal cancer relies on cross-sectional imaging to identify the entire extent of tumor. Rarely, the exact limits of the tumor may be radiologically occult. Lipiodol is a contrast agent which has been used successfully to mark cancers of the bladder and lung for radiotherapy and surgical resection. We report a patient with an adenocarcinoma of the gastroesophageal junction with tiny tumor implants extending proximally along the length of the esophagus, which were not visible on standard cross-sectional imaging studies. The proximal extent of implants was marked endoscopically using a submucosal injection of lipiodol, and this provided for adequate planning and successful delivery of radiotherapy.
Keywords
Cancer; Esophagus; Contrast media; Radiotherapy
Case Presentation
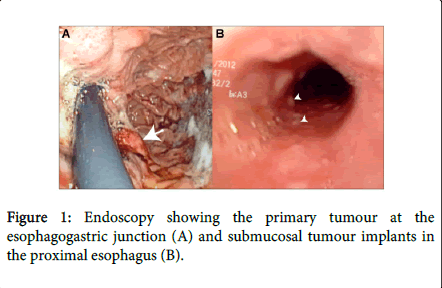
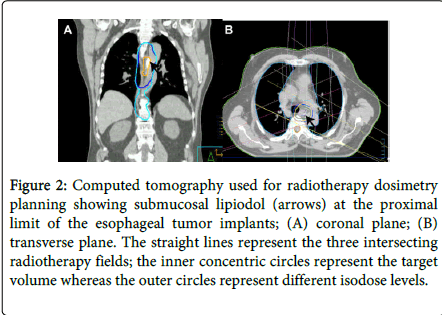
A 73 year-old man was evaluated for an adenocarcinoma of the gastro-esophageal junction. A workup consisting of computed tomography (CT), positron-emission tomography (PET) and endoscopic ultrasound had shown localized disease staged clinically as T3N0. However, endoscopy showed multiple tiny, biopsy-proven, submucosal tumor implants extending proximally over a distance of 12cm from the main lesion; these implants were not visible on other imaging studies, including PET scan, which only showed radiotracer uptake by the main tumor mass (Figure 1). The patient was judged to be medically inoperable and was thus referred for radical chemoradiotherapy. Since a precise delineation of tumor extent is necessary for adequate planning of radiotherapy, the patient underwent another endoscopy with a four-quadrant submucosal injection of lipiodol to mark the proximal limit of tumor implants. One ml of lipiodol was used per quadrant; given the viscosity of lipiodol, the injection pressure was somewhat higher than would have been necessary for standard saline solution. The lipiodol was clearly visible on subsequent CT and provided for adequate planning and successful delivery of radiotherapy (Figure 2).
Figure 2: Computed tomography used for radiotherapy dosimetry planning showing submucosal lipiodol (arrows) at the proximal limit of the esophageal tumor implants; (A) coronal plane; (B) transverse plane. The straight lines represent the three intersecting radiotherapy fields; the inner concentric circles represent the target volume whereas the outer circles represent different isodose levels.
Discussion
Considering the inability of CT to delineate the entire extent of tumor in our patient, our challenge was to choose a convenient method of marking the tumor implants that would be visible on CT in order to allow adequate planning of radiotherapy. Endoscopic clips have been used successfully to mark tumours of the GI tract and for image-guided radiotherapy for bladder cancer [1,2], but the tendency of the clips to dislodge or migrate in the short term would have required that the endoscopic procedure and the pre-radiotherapy evaluation be closely coordinated. This was not feasible due to current scheduling constraints at our institution.
Lipiodol is an iodinated contrast agent that was used in the 1970s-80s in CT scanning and lymphangiography [3,4]. Today, it is mostly used in transarterial chemoembolization (TACE) for hepatocellular carcinoma [5]. Tissue injection of lipiodol has previously been described as a marker for lesions of the bladder and lung as an aid to image-guided radiotherapy and surgical resection, respectively [6,7]. Successful injection of lipiodol has also been reported anecdotally in the 1980s to mark lesions of the esophagus prior to radiotherapy, in an era when early generation CT-scans still had significant limitations [8]. Lipiodol has the distinct advantage of persisting in tissue for prolonged periods, allowing marking and treatment to proceed at different times.
Complications following lipiodol use are very rare, and almost exclusively limited to TACE. These include acute liver failure, cerebral embolism and adult respiratory distress syndrome, and are specifically related to systemic embolization in this setting [9-11]. Animal studies on the intraperitoneal effects of lipiodol suggest a theoretical risk of local inflammation in the event of a transmural injection, but this has never been reported clinically [12]. Our patient did not develop any complications.
We find that endoscopic lipiodol injection can be a useful option to help with radiotherapy planning in the infrequent event that cross-sectional imaging alone is unable to identify the entire extent of an esophageal malignancy. The advantages of lipiodol include simplicity, minimal morbidity, and reliable persistence in tissue. Our case also highlights how an active collaboration between the endoscopist and the radiation oncologist can greatly facilitate the logistics of treatment planning.
References
- Kim SH, Milsom JW, Church JM, Ludwig KA, Garcia-Ruiz A, et al. (1997) Perioperative tumor localization for laparoscopic colorectal surgery. SurgEndosc 11: 1013-1016.
- Hulshof MC, van Andel G, Bel A, Gangel P, van de Kamer JB (2007) Intravesical markers for delineation of target volume during external focal irradiation of bladder carcinomas. RadiotherOncol 84: 49-51.
- Iwai K, Maeda H, Konno T (1984) Use of oily contrast medium for selective drug targeting to tumor: enhanced therapeutic effect and X-ray image. Cancer Res 44: 2115-2121.
- Long DM, Nielson MD, Mutter FK, Lasser EC, Liu MS, et al. (1979) Comparison of radiopaque perfluorocarbon and Ethiodol in lymphography. Radiology 133: 71-76.
- Ahrar K, Gupta S (2003) Hepatic artery embolization for hepatocellular carcinoma: technique, patient selection, and outcomes. SurgOncolClin N Am 12: 105-126.
- Pos F, Bex A, Dees-Ribbers HM, Betgen A, van Herk M, et al. (2009) Lipiodol injection for target volume delineation and image guidance during radiotherapy for bladder cancer. RadiotherOncol 93: 364-367.
- Kwon WJ, Kim HJ, Jeong YJ, Lee CH, Kim KI, et al. (2011) Direct lipiodol injection used for a radio-opaque lung marker: stability and histopathologic effects. Exp Lung Res 37: 310 -317.
- Tanaka Y, Sawada S, Yoshida M, Murata T (1985) Clinical evaluation of computed tomography images in esophageal cancer after submucosal injection of iodized oil. J ComputTomogr 9: 125-132.
- Jia ZZ, Tian F, Jiang GM (2012) Cerebral lipiodol embolism after transarterial chemoembolization for hepatic carcinoma: a case report. World J Gastroenterol 18: 4069-4070.
- Wu GC, Perng WC, Chen CW, Chian CF, Peng CK, et al. (2009) Acute respiratory distress syndrome after transcatheter arterial chemoembolization of hepatocellular carcinomas. Am J Med Sci 338 : 357-360.
- Chung JW, Park JH, Im JG, Han JK, Han MC (1993) Pulmonary oil embolism after transcatheter oily chemoembolization of hepatocellular carcinoma. Radiology 187: 689-693.
- Eisenberg AD, Winfield AC, Page DL, Holburn GE, Schifter T, et al. (1989) Peritoneal reaction resulting from iodinated contrast material: comparative study. Radiology 172: 149-151.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14939
- [From(publication date):
October-2014 - Aug 16, 2025] - Breakdown by view type
- HTML page views : 10303
- PDF downloads : 4636