The Short-term Effect of Air Purification on Lung Function and Blood Pressure among Asthmatics and their Households
Received: 04-Jul-2018 / Accepted Date: 17-Jul-2018 / Published Date: 20-Jul-2018 DOI: 10.4172/2161-0711.1000621
Keywords: Forced expiratory volume; Blood pressure; Asthma; Air pollution, Indoor; Air pollutants; Particulate matter
Introduction
In developed nations, humans spend most of their life indoors. Recently, buildings are being constructed to be more air-tight and energy efficient, which results in the accumulation of indoor pollutants and irritants [1]. Air filtration is a possible solution to improve indoor air quality. Public awareness of indoor air pollution and its impact on health are increasing. Outdoor ambient air is the principal source of indoor pollutants [2]. Other sources include second-hand smoke [3], mold, dampness [4,5], chemicals (e.g., personal care products) [2,6] and particles generated by cooking and heating [6].
The impact of indoor air on health ranges in severity (e.g., unwanted odor, irritation, allergy, respiratory chronic illnesses and cancer) [7] and can be divided into three categories: i) complaints related to a subjective feelings, such as thermal discomfort, dry or dusty air, and bad odors [8]; ii) building-related illnesses caused by microbial agents, such as Legionnaire's disease [9], and humidifier fever; and iii) acute symptoms related to the building environment and the time spent indoors, known as sick building syndrome (SBS). They are often used to evaluate office environments and to assess employees’ productivity [10]. Symptoms of SBS can be divided into general symptoms (e.g., headache, dizziness, and fatigue), mucous membrane symptoms (e.g., eye, nose or throat irritation), and flu-like symptoms, which are the most frequent [11,12].
Bronchial asthma prevalence is 11% among the National Guard residential city population. It is the second most common health condition among the National Guard population and the most common among the children [13]. It has been suggested that indoor air irritants increase the occurrence of asthma [14]. For reducing the exposure to indoor pollutants, a group of measures known as environmental control practices (ECPs) has been recommended [1]. Some of these practices depend on building remediation or modification of the internal environment, while others depend on modifying the occupant’s practices, such as smoking cessation, changing of mattresses, and avoiding pets. Air filtration is an easy-toapply and low-cost practice, which can be provided either as whole house filtration (through an air conditioning system) or as single room filtration (by portable air cleaners). Both filtration methods have been examined and shown to have beneficial effects on the occupant’s health [15].
To our knowledge, in Saudi Arabia, no studies have addressed indoor air pollution and its effect on health. Although a few studies have assessed indoor air quality at schools [16] and hospitals [17], the air quality in houses has not been examined, nor have the effects of air filtration on the households’ health.
Here we aim to measure the short-term effect of air purification (intervention) on lung function and blood pressure among asthmatics and their households living at National Guard residential city in Jeddah, Saudi Arabia. In addition to measure the effect of indoor air quality of the families’ houses.
Materials and Methods
Study sample
A total of 174 participants were recruited in the study. The sample size was calculated using Epi Info for Interventional Studies, with a significance level (alpha) of 0.05 and 90% power. Hypothetical percentage of not exposed (not applying the intervention) with the outcome by 40% and least expected percentage of exposed (using the intervention) giving the outcome by 60%. The previous hypothetical percentages were used depending on a similar study where the effect shown in approximately 100% of the exposed houses, that the air filtration applied [18]. The following flowchart shows the epi info calculation results (Table 1).
| Sample Size: Clinical Trials | |||
|---|---|---|---|
| Two-sided significance level(1-alpha): | 95 | ||
| Power(1-beta, % chance of detecting): | 90 | ||
| Ratio of sample size, unexposed/exposed: | 1 | ||
| Percent of unexposed with outcome: | 40 | ||
| Percent of exposed with outcome: | 60 | ||
| Odds ratio: | 2.3 | ||
| Risk/Prevalence ratio: | 1.5 | ||
| Risk/Prevalence difference: | 20 | ||
| Kelsey | Fleiss | Fleiss with CC | |
| Sample size - exposed | 132 | 130 | 140 |
| Sample size-nonexposed | 132 | 130 | 140 |
| Total sample size | 264 | 260 | 280 |
Table 1: The epi info calculation results.
The study participants were recruited from 29 families living at the National Guard residential city, which is located in Jeddah, Saudi Arabia. Families were recruited randomly to the study using cluster sampling, targeting families with at least one asthmatic member to examine the effect of air purification on asthma patients and their relatives who have a history of atopy (family history of asthma). Sealed opaque envelopes were used to randomly allocate the participating families (cluster) into intervention or control groups. There were 13 households in the intervention group and 16 families in the control group. The study was conducted at the houses of the participants. The participating families are living at National Guard Residential City in Jeddah, Saudi Arabia, which is a special residential city for the families of the workers at the National Guard of Saudi Arabia, located in the center of Jeddah city and divided into five geographical districts.
There are 1235 residential buildings in the city, similar in the number of the rooms, size, and infrastructure. The families who have at least one asthmatic patient were determined using the Ministry of National Guard Community Health Survey (MNGCHS)-2013. This survey is made to assess different health conditions among the population of the National Guard. The survey shows that bronchial asthma is the second most common health condition among the National Guard population and the most common among the children [13].
Study design
A randomized controlled repeated-measures design was conducted to evaluate the short-term effect of air purification on indoor air quality and household health using portable self-standing air filters indoors for a week. During home visits, pre- and post-measurements of the study outcome were taken from the participants. The whole period of data collection lasted 4 weeks.
The intervention (air filtration) was made using a commercial electrostatic air purifier (3M Filtrete Ultra Clean Air Purifier FAP03). The same air purifier has been used in a similar study and shown beneficial results [18]. Two air purifiers were used at each participating house on each floor in at least two rooms. The air purifier device was placed at one corner of the room and kept working without interruption for at least 2 hours, every day of the interventional week.
The room of the asthmatic patient and the living room downstairs were included in the intervention. Families assigned to the control group were asked to ventilate the house by opening at least four windows in each floor completely for two consecutive hours per day to allow natural outdoor air ventilation, every day during intervention week.
Instruments
The study outcomes were lung function and blood pressure among all the participants, and indoor air quality among their houses. Lung function was assessed for all family members regardless of their health conditions using portable spirometers. The assessment followed standard guidelines [19]. The portable spirometers used height, weight, and age data to calculate the expected values for each participant.
A trained assistant nurse showed each subject how to use the spirometer to give an accurate result at each home visit. Every member made the test three times in each set; the highest reading was used in the analyses. Blood pressure was assessed in the sitting position using a standard mercury sphygmomanometer. Mothers of the participating families were interviewed by a questionnaire that was constructed to assess the house environment and possible sources of indoor pollutants.
For indoor air quality, multiple devices were used. MultiRAE is a portable multi-gas detector and monitor and was used to measure CO2 and total volatile organic compounds (TVOC) levels and to detect aldehyde levels indoors. The temperature and humidity were assessed using a portal device (THWD-10W).
A 4-IN-1 Air Detector (WP6912) was used to measure the level of particulate matter (PM2.5 and PM10). All of the tools needed take, at most, 30 s to give stable readings. An average reading was calculated of indoor air measurements that were taken from four rooms, two upstairs and two downstairs. All of the measurements were taken by the investigator, a qualified nurse or the researcher’s assistants
Statistics
Data were coded and entered using Statistical Package for Social Sciences (SPSS) v.23. Demographic and clinical data were analyzed using descriptive statistics, including means, standard deviations, and frequencies. Demographic and clinical data were analyzed using descriptive statistics, including means, standard deviations, and frequencies. To test for significance, a paired t-test was used for lung function, blood pressure measurements, and the indoor air parameters. This study used an alpha level of 0.05 for statistical significance. Important results of this study are presented using tables.
Ethical consideration
The study was approved by the Saudi Board Community Medicine Residency Program Scientific Committee, and data collection tools and devices were approved by the King Abdullah International Medical Research Center (KAIMRC) Ethics and Scientific Committee.
All of the study population received detailed information regarding the purpose and nature of the study and provided informed written consent before enrollment. The participants were told about their right to withdraw from the study at any time.
Results
The mean (SD) number of family members was 7 (2). The mean age group of the participant was 23 (16) with a large variation, where the youngest was 4-years-old, and the oldest was 62-years-old. The majority of participants were female (58%). There was great variation in the level of education; however, almost one third 30.5% had elementary school education.
Since the study was conducted among asthmatics and their families, the prevalence of asthma was high. Forty-three of 174 individuals reported that they had been diagnosed by a physician with bronchial asthma (24.7%). The prevalence of dermatitis (11.5%) and allergic rhinitis (12.6%) was also high. This was expected since the study was conducted at houses occupied by asthmatics; the high prevalence of allergic diseases has contributed to the history of atopy in the family.
Smoking prevalence was low, with about 69% of families having no smokers; which was expected since the majority of the participants were children and females, and therefore a low prevalence of secondhand smoke was detected (19%).
Characteristics of households’ indoor environment
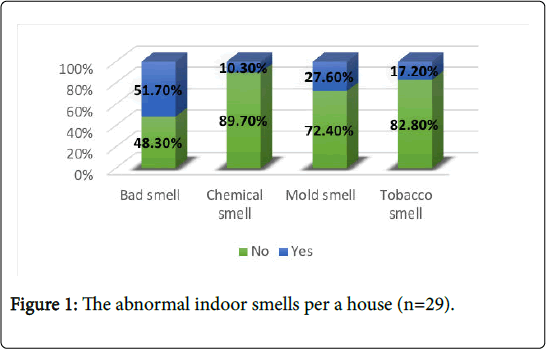
The majority of households have no smokers (69%). However, 20.7% of families have at least one smoker who smokes daily in-house. More than half of households (55.2%) exposed to coal that used for incense burn 3-4 times a week, and 24% exposed to it on daily basis. Using of insecticides daily was reported in 17.2 % of the homes, whereas daily using of chemical was reported in 75.9%. More than half of the households (51.7%) have mentioned that there was a bad smell at their house and 27.6% reported existing of mold smell. Tobacco smell and chemical smell was reported in low percentages 17.2% and 10.3% receptively (Figure 1).
The damp stain was observed on majority of houses (75.9%), Thus, 41.4% of houses have at least one room/bathroom with damp stain, and 20.7% have more than two rooms/bathrooms with damp stain. Whereas the mold spots have been less observed, 27.6% of houses have at least one room/bathroom with mold spots, and 6.9% have more than two rooms/bathrooms with mold spots.
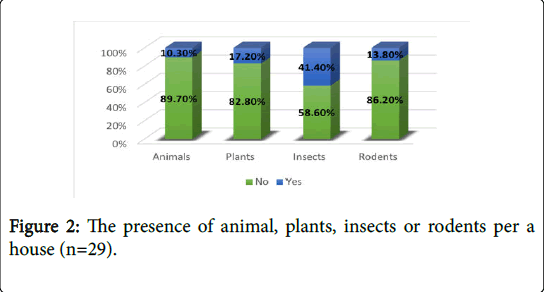
Very few households have been raising animals (10.1%), and some have plants (17.2%); however, insects spreading were reported in 41.1% of houses, and rodents in 13.8% of houses (Figure 2).
Recent renovation (wall painting mainly) have been performed on 24.1% of homes. Air filter was not available for all dwellings. Almost half of the households (48.3%) mentioned that they rarely open their house windows for outdoor air supply.
Effect of air filtration on lung function and blood pressure
A paired samples t-test was used to test the difference in the lung function measurements (FEV1 and FVC), pre- and post-air filter intervention. Table 2 shows that there was a significant difference in FEV1 (p=0.02). The mean FEV1 had increased post-air filter intervention from 2.19 to 2.24.
| Paired differences | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Std. Error | Lower | Upper | t | df | P value | |
| FEV1 | -0.05 | 0.15 | 0.02 | -0.09 | -0.01 | -2.42 | 53 | 0.02* |
| FVC | -0.02 | 0.25 | 0.03 | -0.09 | 0.05 | -0.58 | 51 | 0.57 |
| *The significance level (a) was set at P<0.05 | ||||||||
Table 2: Comparing lung function test scores pre- and post-air filter intervention (n=54).
A paired samples t-test was used to test the difference in blood pressure (systolic and diastolic) pre- and post-air filter intervention. It showed that there were no significant differences in blood pressure in relation to pre- and post-air filter intervention.
Effect of air filtration on indoor air quality
We detected a significant difference in aldehyde level (p=0.03) when comparing pre- and post-air filter intervention (paired samples t-test. The mean value of most air quality measurements decreased (improved) after air filter intervention, although these did not reach statistical significance (Table 3).
| Mean | Std. Deviation | Std. Error Mean | |
|---|---|---|---|
| CO2 pre Air Filter | 844.3 | 234.8 | 60.6 |
| CO2 post Air Filter | 761.6 | 180.8 | 46.7 |
| VOC pre Air Filter | 372.9 | 596.2 | 153.9 |
| VOC post Air Filter | 126 | 66 | 17 |
| PM2.5 pre Air Filter | 153.6 | 291.1 | 75.2 |
| PM2.5 post Air Filter | 124.5 | 219.9 | 56.8 |
| PM10 pre Air Filter | 156.6 | 274.1 | 70.8 |
| PM10 post Air Filter | 127.7 | 213.2 | 55.1 |
| Aldehyde pre Air Filter | 0.1 | 0.1 | 0 |
| Aldehyde post Air Filter | 0 | 0.1 | 0 |
Table 3: Descriptive information of the air quality measurements pre- and post-air filter intervention (n=15).
Effect of outdoor air ventilation on lung function and blood pressure
We detected no significant differences when comparing lung function measurements (FEV1 and FVC) pre and post opening windows intervention (paired samples t-test, FEV1, p=0.063; FVC, p=0.57). Comparing blood pressure (systolic and diastolic) pre and post open windows intervention, we detected no significant differences.
Effect of outdoor air supply on indoor air quality
Comparing the difference in air gas measurements pre and post opening windows intervention, we detected differences in CO2 (p<0.001) and VOC (p=0.03) measurement (paired samples t-test, Table 4).
| Paired differences | 95% CI | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Std. Error | Lower | Upper | t | df | P value | |
| CO2 | 165.3 | 156 | 36.8 | 87.8 | 242.9 | 4.5 | 17 | 0.00* |
| VOC | 471.1 | 822.5 | 193.9 | 62 | 880.1 | 2.4 | 17 | 0.03* |
Table 4: The differences of indoor air quality pre and post opening windows intervention.
Discussion
A randomized controlled repeated-measure design was carried out to evaluate the short-term effect of air purification on lung function and blood pressure among asthmatics and their households living at National Guard residential city in Jeddah. We targeted the houses that are occupied by at least one asthma patients. Because according to recent literature, indoor air pollutants and suspended particles are higher at asthmatic children’s houses in comparison to homes without asthmatics [14]. In addition to that, asthma patients are the most affected by poor indoor environment. Asthma admission is significantly higher in the presence of elevated levels of PM2.5, PM10, NO2, and Ozone [20]. Mold and home dampness are contributing to exacerbation of asthma [4]. An interventional study examined the effect of remediation activities to remove mold from the houses, found a significant decline in asthma symptoms in comparison to controls [21]. For the study population, who are living at National Guard Residential city in Jeddah, asthma considered a priority since it is the most common chronic disease among their children [13].
Here we detected a significant improvement in FEV1 (p=0.02), but not FVC, after the use of an air filter. The opening of windows had no effect on respiratory lung functions (FEV1, p=0.063; FVC, p=0.57). In general, our findings suggest that indoor air filters substantially reduce indoor levels of pollutes, resulting in an improvement in lung function. Air pollutes known to have adverse effects on respiratory health, cause inflammation in the lungs and oxidative stress [15,21].
Weichenthal et al. [18] reported similar findings in their crossover study done over 20 houses with 37 participants. Weichenthal et al. reported a statistically significant improvement in FEV1 and PEFR for the majority of cases (FEV1: 158 ml, 95%CI: 5.8, 321; PEFR: 544 ml, 95%CI: 113, 1203). The randomized crossover design was an important strength in this study. A Chinese study involving 35 health students showed the beneficial effects of using air filters on overall lung function, which resulted in a decrease in decreased biomarkers of airway inflammation [22]. On the contrary, a study conducted in Denmark, which included 27 houses (48 participants) reported different results [23]. The air filters used failed to improve lung functions significantly, although they did reduce the concentration of particles from 7669 to 5352 particles/cm3with an associated decrease of aerodynamic diameters ≤ 2.5 μm (PM 2.5) from 8 to 4 mg/m3. The limitation of this study is the limited statistical power and the heterogeneous population, where some of them are taking cyclooxygenase inhibitors and cardiovascular medications.
We detected no significant differences in blood pressure in relation to pre- and post-air filter intervention, with a mean of systolic blood pressure of 117 mmHg and diastolic of 79 mmHg pre- and post-air filter intervention. Additionally, there were no significant differences in blood pressure concerning pre- and post-opening windows. Allen et al. [24] reported similar results in a study conducted with 45 health participants, with no significant changes in BP after using air filters. Additionally, another crossover study of 21 non-smoking couples detected no significant effects on blood pressure with the use of air filters, regardless of the fact that different air particles were reduced [25].
However, many other studies have reported a significant reduction in BP after using air filters [22,26-28] These findings might be due to the associated reductions in PM2.5, which were absent in our study. Chang et al. performed a study in Taiwan based on personal measurements of PM2.5 with monitoring of BP, which showed that a 10 μg/m3 increase in PM2.5 was associated with significant increases in SBP (by 0.81 mmHg, 95%CI: 0.19-1.43 mmHg) and in DBP by 0.63 mmHg (95%CI: 0.17-1.10 mmHg) [29].
Comparing pre- and post-air filter intervention, we detected a significant difference in aldehyde level (p=0.03). Also, the mean of most air quality measurements decreased (improved) after air filter intervention, although these did not reach statistical significance. Additionally, comparing levels before and after using air filters, using the Wilcoxon signed ranks test, we detected a significant difference in air pollution (p=0.025). Moreover, there were significant differences in CO2 (p<0.001) and VOC (p=0.03) measurements when comparing pre- and post-opening windows interventions, as well as significant difference in air pollution (p=0.014).
However, our findings also indicate that the use of indoor air filters might be insufficient to reduce indoor particulate matter (PM) levels to values similar to outdoor concentrations; mostly due to smoking or other bad habits.
In fact, Health Canada’s most recent guidance document on indoor PM2.5 recommends that indoor levels be kept lower than outdoor values [30]; therefore, the best cost-effective means of decreasing indoor PM2.5 is to eliminate smoking and other bad habits before considering the use indoor air filters. Although we have a low smoking rate, this approach has the added benefit of reducing other air pollutants associated with cigarette smoking, which are not removed by the air filter.
Our study has strengths. First, this randomized controlled design facilitated causal inferences of air purification, reduction of air pollutants, and improved health indicators. Second, we measured many indicators of cardiorespiratory health, which enabled a more systematic assessment of the potential health benefits of reducing indoor air pollution.
Third, the experimental environment was well controlled thus exposure measurement error was minimized. Finally, because this intervention period was completed over one week, we avoided potential temporal confounding caused by seasonal changes and changes in participant behavior.
Our study has limitations. First, the study included only 147 participants who might have missed some potentially important but modest differences attributable to the relatively small sample size. Second, following up the study sample was laborious and timeconsuming. Multiple trials needed to just get an initial approval and with some of the participants didn’t show up during the home visits (especially males due to work duties).
Conclusions
This interventional study detected significant cardiopulmonary benefits of indoor air purification filters, with some improvement in respiratory function, particularly the FEV1 parameter. On the contrary, blood pressure was unchanged by the interventions.
Based on our findings, we recommend the use of commercial filters inside homes, if available, but necessitate the control of indoor sources of air pollution and, in particular, the need for a multisector approach for major changes to reduce the permanent exposure to indoor dampness and mold at houses of the National Guard in residential city.
Future studies should evaluate the potential health benefits of longterm air purification among more vulnerable populations, such as children, older adults or people with cardiopulmonary diseases.
Author Contributions
Conceptualization, Reem Alnemari and Badr Aljasir; Data curation, Amina Bargawi; Formal analysis, Reem Alnemari and Amina Bargawi; Investigation, Reem Alnemari and Alaa Alnemari; Methodology, Reem Alnemari, Amina Bargawi and Alaa Alnemari; Project administration, Badr Aljasir; Resources, Reem Alnemari; Supervision, Fadel Kamal; Validation, Fadel Kamal and Badr Aljasir; Visualization, Reem Alnemari; Writing-original draft, Reem Alnemari; Writing-review & editing, Fadel Kamal, Badr Aljasir, Amina Bargawi and Alaa Alnemari.
Acknowledgment
We want to thank everyone helped in data collection for their valuable cooperation: from Community and Preventive Medicine Center, National Guard Health Affairs, also the students volunteered from King Abdul-Aziz University, Faculty of Medicine and Al-Farabi Colleges and all participants in this research. We would like to gratefully acknowledge support from preventive medicine department of National Guard-Health Affairs, that provide all the instruments needed for the measurements and the intervention.
References
- Allen JG, MacNaughton P, Satish U, Santanam S, Vallarino J, et al. (2016) Associations of cognitive function scores with carbon dioxide, ventilation, and volatile organic compound exposures in office workers: A controlled exposure study of green and conventional office environments. Environ Health Perspect.
- Bernstein JA, Alexis N, Bacchus H, Bernstein IL, Fritz P, et al. (2008) The health effects of non-industrial indoor air pollution. J Allergy Clin Immunol 121: 585-591.
- (1994) Environmental tobacco smoke. Health effects and prevention policies. Council on scientific affairs, american medical association. Arch Fam Med 3: 865-871.
- Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J (2011) Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ Health Perspect 119: 748-756.
- Vesper SJ, McKinstry C, Yang C, Haugland RA, Kercsmar CM, et al. (2006) Specific molds associated with asthma in water-damaged homes. J Occup Environ Med 48: 852-858.
- Kim KH, Pandey SK, Kabir E, Susaya J, Brown RJ (2011) The modern paradox of unregulated cooking activities and indoor air quality. J Hazard Mater 195: 1-10.
- Seppänen OA, Fisk WJ (2004) Summary of human responses to ventilation. Indoor Air 14: 102-118.
- Christine A (2004) Erdmann MGA. Mucous membrane and lower respiratory building related symptoms in relation to indoor carbon dioxide concentrations in the 100-building BASE dataset. Indoor Air 14: 127-134.
- Johanning E (2004) Indoor moisture and mold-related health problems. Eur Ann Allergy Clin Immunol 36: 182-185.
- Wargocki P, Wyon DP, Baik YK, Clausen G, Fanger PO (1999) Perceived air quality, sick building syndrome (SBS) symptoms and productivity in an office with two different pollution loads. Indoor Air 9: 165-179.
- Norbäck D (2009) An update on sick building syndrome. Curr Opin Allergy Clin Immunol 9: 55-59.
- Joshi SM (2008) The sick building syndrome. Indian J Occup Environ Med 12: 61-64.
- Region W, Region W (2013) National guard community health survey ( NGCHS ) 2013 king faisal residential city-Jeddah.
- Kumar R, Nagar JK, Goel N, Kumar P, Kushwah AS, et al. (2015) Indoor air pollution and asthma in children at Delhi, India. Pneumonol Alergol Pol 83: 275-282.
- Sublett JL (2011) Effectiveness of air filters and air cleaners in allergic respiratory diseases: A review of the recent literature. Curr Allergy Asthma Rep 11: 395-402.
- El-Sharkawy (2014) Study the indoor air quality level inside governmental elementary schools of Dammam city in Saudi Arabia. Int J Environ Health Eng 3: 22.
- El-Sharkawy MF, Noweir MEH (2014) Indoor air quality levels in a university hospital in the eastern province of Saudi Arabia. J Family community Med 21: 39-47.
- Weichenthal S, Mallach G, Kulka R, Black A, Wheeler A, et al. (2017) A randomized double-blind crossover study of indoor air filtration and acute changes in cardiorespiratory health in a first nations community. Indoor Air 23: 175-184.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. (2005) Standardisation of spirometry. Eur Respir J 26: 319-338.
- Wargocki P, Sundell J, Bischof W, Brundrett G, Fanger PO, et al. (2002) Ventilation and health in non-industrial indoor environments: Report from a European multidisciplinary scientific consensus meeting (EUROVEN). Indoor Air 12: 113-128.
- Norbäck D, Nordström K (2008) Sick building syndrome in relation to air exchange rate, CO2, room temperature and relative air humidity in university computer classrooms: An experimental study. Int Arch Occup Environ Health 82: 21-30.
- Chen R, Zhao A, Chen H, Zhao Z, Cai J, et al. (2015) Cardiopulmonary benefits of reducing indoor particles of outdoor origin: A randomized, double-blind crossover trial of air purifiers. J Am Coll Cardiol 65: 2279-2287.
- Karottki DG, Spilak M, Frederiksen M, Gunnarsen L, Brauner EV, et al. (2013) An indoor air filtration study in homes of elderly: Cardiovascular and respiratory effects of exposure to particulate matter. Environ Health 12: 116.
- Allen RW, Carlsten C, Karlen B, Leckie S, Eeden S van, et al. (2011) An air filter intervention study of endothelial function among healthy adults in a woodsmoke-impacted community. Am J Respir Crit Care Med 183: 1222-1230.
- Bräuner EV, Forchhammer L, Møller P, Barregard L, Gunnarsen L, et al. (2008) Indoor particles affect vascular function in the aged: An air filtration-based intervention study. Am J Respir Crit Care Med 177: 419-425.
- Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, et al. (2002) Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation 105: 1534-1536.
- Tsai D-H, Riediker M, Wuerzner G, Maillard M, Marques-Vidal P, et al. (2012) Short-term increase in particulate matter blunts nocturnal blood pressure dipping and daytime urinary sodium excretion. Hypertension 60: 1061-1069.
- Pieters N, Koppen G, Van Poppel M, De Prins S, Cox B, et al. (2015) Blood pressure and same-day exposure to air pollution at school: Associations with nano-sized to coarse pm in children. Environ Health Perspect 23: 737-742.
- Chang LT, Chuang KJ, Yang WT, Wang VS, Chuang HC, et al. (2015) Short-term exposure to noise, fine particulate matter and nitrogen oxides on ambulatory blood pressure: A repeated-measure study. Environ Res 140: 634-640.
- Government of Canada (2012) Guidance for fine particulate matter (PM2.5) in residential indoor air. Canada.
Citation: Alnemari R, Kamal FMS, Aljasir B, Bargawi A, Alnemari A (2018) The Short-term Effect of Air Purification on Lung Function and Blood Pressure among Asthmatics and their Households. J Community Med Health Educ 8: 621. DOI: 10.4172/2161-0711.1000621
Copyright: © 2018 Alnemari R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3821
- [From(publication date): 0-2018 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 2913
- PDF downloads: 908