Pattern of Sharps Injuries in Ophthalmic Practice
Received: 07-Apr-2013 / Accepted Date: 15-Jul-2013 / Published Date: 17-Jul-2013 DOI: 10.4172/2161-1165.1000128
Abstract
Sharps injuries are well known risk for health care workers in ophthalmology. The objective of this study is to describe the pattern of sharps injuries in ophthalmic practice. This 7 years prospective study revealed unique pattern of sharps injuries in ophthalmology. Forty-two HCWs were injured. Nurses sustained 50.0% of sharps injuries while technicians sustained 31% and doctors 19%. Theatre was the most common location for sharps injuries 54.8% followed by clinic 14.3% then wards and laboratory at 11.9% each.
Keywords: Sharps injuries; Ophthalmic Practice; Health Care Workers (HCW)
160359Introduction
The Sharps injuries in health care facilities are well-known risk for Health Care Workers (HCW). Blood born viruses are greatly transmitted through the percutaneous penetration of sharps. The fractions of blood born viral infection attributed to the sharps injuries in HCWs are 37%, 39% and 4.4% for HBV, HCV and HIV respectively [1].
The ophthalmology speciality consists of medical and surgical components with predominance of surgical components in eye specialist hospitals. In general, surgical injuries continued to increase during the period that nonsurgical injuries decreased significantly [2]. In addition to that, the microsurgery nature of ophthalmology increases the risk of sustaining sharps injuries [3]. An old retrospective study done by Mansour [4], to determine the needle-stick injury rate among employees of the department of ophthalmology versus the other departments found that ophthalmologists had the highest incidence per person of needle injuries among physicians [4]. In a German study done by Sabine Wicker et al. addressed the risk of needle-stick injuries from occupational medicine viewpoint found among his results that the frequency of needle-stick injuries in ophthalmology speciality was 28.6% [5]. Furthermore, the events of sharps injuries in ophthalmic practice are not fully reported. In one study, 50% of sharps injuries were not reported [6].
Although the rate of sharps injuries in ophthalmic practice is high in comparison to other medical specialties but a large proportion of the sharps injuries in ophthalmic practice is preventable. In one study up to 93% of Sharps injuries in ophthalmic practice can be or possibly be avoided [5].
Internationally published sharps injuries studies in ophthalmic practice are few. Locally to my knowledge no sharps injuries study in ophthalmic practice in Saudi Arabia has been done.
The objectives of this study are to describe the epidemiology of the sharps injuries in ophthalmic practice in Dhahran Eye Specialist Hospital (DESH) and to determine the annual incidence rate of the sharps injuries among Health Care Workers (HCWs) of the hospital.
Study Design
Prospective study of sharps injuries for 7 years from 2006-2012 among Health Care Workers (HCWs) of Dhahran Eye Specialist Hospital (DESH).
Materials and Methods
A prospective study of sharps injuries was begun in 2006 by the Infection Control Department (ICD) of Dhahran Eye Specialist Hospital (DESH), which is a 200-bed tertiary care eye hospital founded to receive referred eye patients from general hospitals. The infection control department performs the surveillance and management of sharps injuries. All technical employees (doctors, nurses, and technicians and allied workers) of Dhahran Eye Specialist Hospital (DESH) upon arrival to work are recorded in the files of infection control department for serologic screening of HBV, HCV and HIV and to receive immunization if indicated and to receive orientation program. The administrative employees are excluded from the program, as they are not involved in direct patient care and considered not at risk of sharps injuries. Once the injured HCW reported to infection control department; the infection control practitioner interview him/ her and complete the sharps injuries surveillance form and apply the post sharps injuries exposure protocol.
The post exposure protocol consists of serology tests and administration of immunoglobulin and hepatitis B vaccine to the unvaccinated or non- respondents and those with low level of anti- HBs (<10 mIU /ml). The previously vaccinated employees with adequate level of anti- HBs (≥ 10 mIU/ml) need no hepatitis B vaccine. The post exposure blood tests for HCV and HIV used to be done at 1, 3, and 6 months from the time of sharps injuries if the source blood which contaminated the sharp object was positive or the source blood is unknown but the victim was from high-risk groups. The post exposure blood test to HBV used to be done at 1 and 6 months of exposure if the source blood was positive or unknown and the victim was not immune.
The surveillance system defined sharps injury as percutaneous penetration of sharp object whether contaminated or not by blood or other bodily fluid. The surveillance collects data on the demography, the job category (doctor, nurse and technician and allied workers), and the place of injury, the site of injury, the tool of injury, and the tasks that were performed during the sharps injuries. The allied workers here are the cleaners who collect the medical waste.
Data entry and analysis were done by using Epiinfo 3.5.1.
Results
A total of 42 sharps injuries were recorded from Dhahran eye specialist hospital over the 7 years period from 2006 to 2012.
The mean age of injured HCWs in the study was 37.1 years. The males represented 52.4% (n = 22) of injured HCWs. Saudi national staff represented 47.6% (n = 20) while non-Saudi represented 52.4% (22) of injured HCWs.
The nurses sustained 50% (n = 21) of total sharps injuries. Nineteen per cent (n = 8) of sharps injuries were sustained by doctors while technicians and allied workers sustained 31% (n = 13) of the injuries (Table 1).
| Variable | Number | % of Injuries |
|---|---|---|
| Occupation | ||
| Doctor | 8 | 19 |
| Nurse | 21 | 50 |
| Technicians | 13 | 31 |
| Anatomical Site | ||
| Right hand | 25 | 59.5 |
| Left hand | 15 | 35.7 |
| Leg | 2 | 4.8 |
| Location | ||
| Theater | 23 | 54.8 |
| Laboratory | 5 | 11.9 |
| Ward | 5 | 11.9 |
| CSSD | 2 | 4.8 |
| ER | 1 | 2.4 |
| Clinic | 6 | 14.3 |
| Circumstances | ||
| Handling instrument | 20 | 47.6 |
| Procedural | 13 | 31.0 |
| Disposal & cleaning | 9 | 21.4 |
| Injury tool | ||
| Needle | 35 | 83.3 |
| Scalpel | 2 | 4.8 |
| Unspecified | 5 | 11.9 |
Table 1: Distribution of sharps injuries characteristics in Dhahran eye Specialist Hospital 2006-2012.
Most of the sharps injuries 60% (n = 25) occurred in the right hand of the victim while 35.7% (n = 15) of the sharps injuries occurred in left hand and only 4.8% (n = 2) of the sharps injuries occurred in the leg.
The operation room accounted for 54.8% (n = 23) of the sharps injuries locations. The clinic accounted for 14.3% (n =6) of the sharps injuries while each of the laboratory and the ward represented 11.9% (n = 5) of sharps injuries locations. The central sterilization department represented 4.8% (n = 2) of sharps injuries location and the emergency department represented 2.4% (n =1) of sharps injuries locations.
In operation room (OR) 39.1% (n = 9) of the injured health care workers were technicians. Twenty six percent (n = 6) of the injured HCWs were nurses and 34.8% (n = 8) were doctors (Table 2).
| Variables | Occupation | ||||||
|---|---|---|---|---|---|---|---|
| N | Doctor | Nurse | Technician | ||||
| Injury tool | N | % | N | % | N | % | |
| Needle | 35 | 6 | 17.1 | 21 | 60 | 8 | 22.8 |
| Scalpel | 2 | 1 | 50 | 0 | 0 | 1 | 50 |
| Others | 5 | 1 | 20 | 0 | 0 | 4 | 80 |
| Place of injury | |||||||
| Operation room | 23 | 8 | 34.8 | 6 | 26.1 | 9 | 39.1 |
| Clinic | 6 | 0 | 0 | 4 | 66.7 | 2 | 33.3 |
| Laboratory | 5 | 0 | 0 | 5 | 100 | 0 | 0 |
| CSSD | 2 | 0 | 0 | 0 | 0 | 2 | 100 |
| Ward | 5 | 0 | 0 | 5 | 100 | 0 | 0 |
| ER | 1 | 0 | 0 | 1 | 100 | 0 | 0 |
| Site of injury | |||||||
| Right hand | 26 | 3 | 11.5 | 13 | 50 | 10 | 38.5 |
| Left hand | 14 | 3 | 21.4 | 8 | 57.1 | 3 | 21.4 |
| Left leg | 2 | 2 | 100 | 0 | 0 | 0 | 0 |
| Circumstances | |||||||
| Handling instrument | 20 | 2 | 10 | 9 | 45 | 9 | 45 |
| Recapping | 11 | 1 | 9.1 | 7 | 63.6 | 3 | 27.3 |
| Passing instrument | 7 | 1 | 14.3 | 1 | 14.3 | 5 | 71.4 |
| Unpacking the set | 1 | 0 | 0 | 0 | 0 | 1 | 100 |
| Uncovering the needle | 1 | 0 | 0 | 1 | 100 | 0 | 0 |
| Procedural | 13 | 5 | 38.5 | 6 | 46.2 | 2 | 15.4 |
| Disposal & cleaning | 9 | 1 | 11 | 5 | 55.6 | 3 | 33.3 |
Table 2: Distribution of sharps injuries by job categories among HCWs. DESH 2006-2012.
Handling the instruments represented 47.6% (n = 20) of the sharps injuries circumstances while 31.0% (n = 13) of the sharps injuries occurred during the procedures and 21.4% (n = 9) occurred during the disposal and/or cleaning (Table 1). Of the handling injuries 55% (n = 11) were due to recapping of the needles. Thirty five percent (n = 7) of the handling injuries were due to passing the instrument. Each of Uncovering the needle and unpacking the set represented 5% of the handling injuries (n = 1) (Table 2).
Eighty-three percent (n = 35) of the sharps injuries were caused by needle while 4.8% (n = 2) of the sharps injuries were caused by scalpel and 11.9% (n = 5) of the sharps injuries were caused by unspecified tool (Table 1). Of the needle- injured HCWs, 60% (n = 21) were nurses and 22.8% (n = 8) were technicians while 17% (n = 6) were doctors (Table 2).
The Serology tests were done in 97.6% (n = 41) of the injured health care workers and none of them was found to be positive for any of HBV, HCV and HIV during the 6 months follow up period. We were able to identify and test the source of blood which contaminated the sharp object in 85.7% (n = 36) of events. All of the tested samples were negative for HBV, HCV and HIV. Six injuries were sustained with uncontaminated needles.
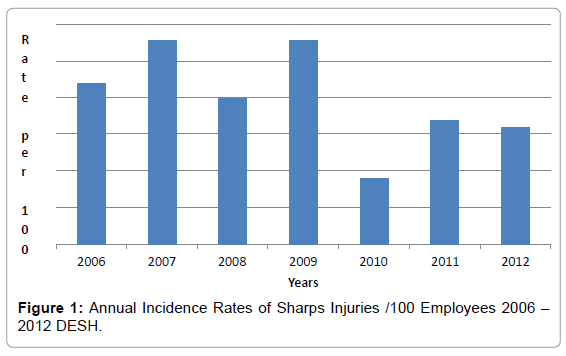
Over the 7 years period the annual incidence rate of sharps injuries per 100 employees showed variations from year to year with mean rate of 2.0 +/- 0.38 Standard Deviation (Table 3) (Figure 1). It ranged between 0.9-2.8 per 100 employees.
| Year | Employee | Sharps injuries | Rate % |
|---|---|---|---|
| 2006 | 229 | 5 | 2.2 |
| 2007 | 252 | 7 | 2.8 |
| 2008 | 297 | 6 | 2.0 |
| 2009 | 316 | 9 | 2.8 |
| 2010 | 337 | 3 | 0.9 |
| 2011 | 347 | 6 | 1.7 |
| 2012 | 368 | 6 | 1.6 |
| Mean | 2.0 | ||
| SD | 0.38 |
Table 3: Annual incidence rate of sharps injury per 100 employees (2006-2012) DESH.
Discussion
In this study, the majority of injured HCWs were nurses; a finding that has been repeatedly reported in all health care settings [2,3,7-11]. This is because the nurses constitute the major group of health care workers in all health care settings.
The operation room is the most common location where the sharps injuries took place. These findings are consistent with findings reported elsewhere about the sharps injuries in ophthalmic practice and surgical settings [3,12-14]. This is merely a reflection of the main function of the speciality as the surgical component dominates the workloads. The clinic is another common place for the occurrence of sharps injuries in ophthalmic practice due to the fact that some invasive procedures e.g. avastin injection are performed in the clinic. This finding is consistent with results of another sharps injuries study in ophthalmic practice [3].
Although the technicians were the majority of injured HCWs in operation room (OR) but the doctors (ophthalmologists) sustained the sharps injuries only in OR. This is because OR is the place where the ophthalmologists have greater exposure to varieties of instruments and sharps; they focus on small field of surgery and apply different techniques and maneuvers.
Most of the sharps injuries sustained by the technicians occurred during passing the instruments to others who will use them i.e. they are not the original user of the instrument or device. This finding was reported in surgical settings [2].
Overall, the right hand was the most frequent injured anatomical sites of HCWs. Although the nurses represented half of the right hand injured HCWs but the rate of right hand injury was greater in the technicians compared to the nurses. This is because the technicians sustained most of their sharps injuries during passing the instrument in which they use the right hand more often due to cultural reasons which advice using of the right hand for handling objects.
Because the instruments are handled by all HCWs before and after the procedures and involved several activities including recapping the needles, passing the instrument, unpacking the sets and uncovering the needles it ranked first of circumstances associated with the sharps injuries. Of handling the instruments recapping of the needle was the most common circumstances associated with the sharps injuries that is consistent with findings reported in other studies on sharps injuries [8,15].
The predominance of the nurses among HCWs injured by the recapping of the needle can be attributed to their greater exposure to needles in several places including laboratory, clinic, OR, ward, and ER as part of their jobs.
Although more nurses sustained the sharps injuries while performing the procedures but the rate of the sharps injuries during the procedures was greater in the doctors compared to the nurses or the technicians. The doctors usually spend time in each procedure and use more than one instrument resulting in prolonged exposure to the sharps during each procedure.
The disposal and/or cleaning of the waste was the least common in this hospital in contrast to the findings reported by another researcher in ophthalmic practice where the disposal of the waste was the most common circumstance for the sharps injuries [4]. This can be due to the underreporting of the sharps injuries by victims. The cleaners who collected and disposed of the waste are illiterate or semi-illiterate, non- local people and had misconception regarding job security if they notify injuries. This was discovered after the observation of covered injuries in the hands of some of them when they disclosed the reasons of no notification of their sharps injuries.
The needle whether suture needle or hollow-bore needle was strikingly the major injury tool which is consistent with finding in surgical and non- surgical health settings [2,7-10,12,16] where the needle was the most frequent injury tool. The needle was the most frequent injury tool among all groups of HCWs and the nurses comprised the majority of HCWs injured by needle due to the diversity of their work, which involves usage of needle in the ward, the theatre, the clinic and the laboratory.
The Limitations of the Study
The self- reporting system results in underreporting of events. This might be true for the repeated injuries to the same person but would be very unlikely for the first injury, as the injured HCW needs to alleviate anxiety and seek medical advice and post exposure measures.
The small size of the sample does not allow for detailed analysis with accuracy that can be generalized.
Conclusion
This study showed special pattern of sharp injury in ophthalmic practice different from what is known in general health care settings.
• The majority of the sharps injuries occurred in operation room (OR) during the handling of the instruments.
• In operation room, the technicians were the majority of injured HCWs and sustained most of their sharps injuries while passing the instruments.
• The ophthalmologists were exclusively sustained the sharps injuries while in operation room during performing the procedures.
• Outside OR the majority of the sharps injuries were among the nurses and the most common circumstance associated with the sharps injuries was the recapping of the needles.
• The frequency of the sharps injuries can substantially be reduced by target education to the technicians and the nurses [15,17-20].
• The ophthalmologists should evaluate methods to reduce sharps injuries in OR.
References
- Rapiti E, Pruss-Ustun A, Hutin Y, Campbell-Lendrum D (2005) Assessing the burden of disease from sharps injuries to health-care workers at national and local levels. Environmental Burden of Disease Series, World Health Organization Protection of the Human Environment.
- Jagger J, Berguer R, Phillips EK, Parker G, Gomaa AE (2011) Increase in sharps injuries in surgical settings versus nonsurgical settings after passage of national needlestick legislation. AORN J 93: 322-330.
- Ghauri AJ, Amissah-Arthur KN, Elsherbiny S (2011) Sharp injury in ophthalmic practice. Eye 25: 443-448.
- Mansour AM (1989) Needlestick injuries in ophthalmology. Ophthalmic Surg 20: 367-369.
- Sabine Wicker, Rene Gottschalk, Holger F Rabenau (2007) Risk of Needlestick Injuries from an Occupational Medicine and Virological Viewpoint. Dtsch Arztebl 104: A3102-A3107.
- Trottmann F, Mojon D (2013) Pattern of injuries to the surgical team during ophthalmosurgical interventions. Klin Monbl Augenheilkd 230: 150-156.
- Memish ZA, Almuneef M, Dillon J (2002) Epidemiology of needlestick and sharps injuries in a tertiary care center in Saudi Arabia. Am J Infect Control 30: 234-241.
- Jahan S (2005) Epidemiology of needlestick injuries among health care workers in a secondary care hospital in Saudi Arabia. Ann Saudi Med 25: 233-238.
- Peng Bi, Tully PJ, Boss K, Hiller JE (2008) Sharps injury and body fluid exposure among health care workers in an Australian tertiary hospital. Asia Pac J Public Health 20: 139-147.
- Ebrahimi H Khosravi A (2007) Needle stick Injuries among Nurses. J Res Health Sci 7: 56-62.
- Nagao Y, Baba H, Torii K, Nagao M, Hatakeyama K, et al. (2007) A long-term study of sharps injuries among health care workers in Japan. Am J Infect Control 35: 407-411.
- Lachowicz R, Matthews PA (2009) The pattern of sharps injury to health care workers at Witbank Hospital. 51: 148-151.
- Naghavi SH, Sanati KA (2009) Accidental blood and body fluid exposure among doctors. Occup Med (Lond) 59: 101-106.
- Hashmi A, Al Reesh SA, Indah L (2012) Prevalence of Needle-stick and Sharps Injuries among Healthcare Workers, Najran, Saudi Arabia. Epidemiol 2: 117.
- Mansour AM (1989) Needlestick injury in the OR: facts and prevention. Todays OR Nurse 11: 15-17.
- Adesunkanmi AK, Badmus TA, Ogunlusi JO (2003) Accidental injuries and cutaneous contaminations during general surgical operations in a Nigerian teaching hospital. East Afr Med J 80: 227-234.
- Yang YH, Liou SH, Chen CJ, Yang CY, Wang CL et al. (2007) The effectiveness of a training program on reducing needlestick Injuries/sharp object injuries among soon graduate vocational nursing school students in Southern Taiwan. J Occup Health 49: 424-429.
- Brusaferro S, Calligaris L, Farneti F, Gubian F, Londero C, et al. (2009) Educational programmes and sharps injuries in health care workers. Occup Med (Lond) 59: 512-514.
- Zafar A, Habib F, Hadwani R, Ejaz M, Khowaja K, et al. (2009) Impact of infection control activities on the rate of needle stick injuries at a tertiary care hospital of Pakistan over a period of six years: an observational study. BMC Infect Dis 9: 78.
- Parsons EC (2000) Successful reduction of sharps injuries using a structured change process. AORN J 72: 275-279.
Citation: Alshihry AM (2013) Pattern of Sharps Injuries in Ophthalmic Practice. Epidemiol 3:128. DOI: 10.4172/2161-1165.1000128
Copyright: © 2013 Alshihry AM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15483
- [From(publication date): 8-2013 - Nov 11, 2025]
- Breakdown by view type
- HTML page views: 10569
- PDF downloads: 4914