Research Article
MIBI SPECT Scan and Ultrasonography in Preoperative Imaging of Primary Hyperparathyroidism
| Nadia Abdulla Batawil* | |
| Department of Radiology, Division of Nuclear Medicine, King Abdulaziz University Hospital, Jeddah, Saudi Arabia | |
| Corresponding Author : | Nadia Abdulla Batawil Department of Radiology, Division of Nuclear Medicine King Abdulaziz University Hospital, P.O. Box 80215, Jeddah-21589, Saudi Arabia Tel: +966 2 640 8222 Fax: +966 2 640 8222 E-mail: nbatawil@kau.edu.sa |
| Received June 03, 2015; Accepted June 10, 2015; Published June 13, 2015 | |
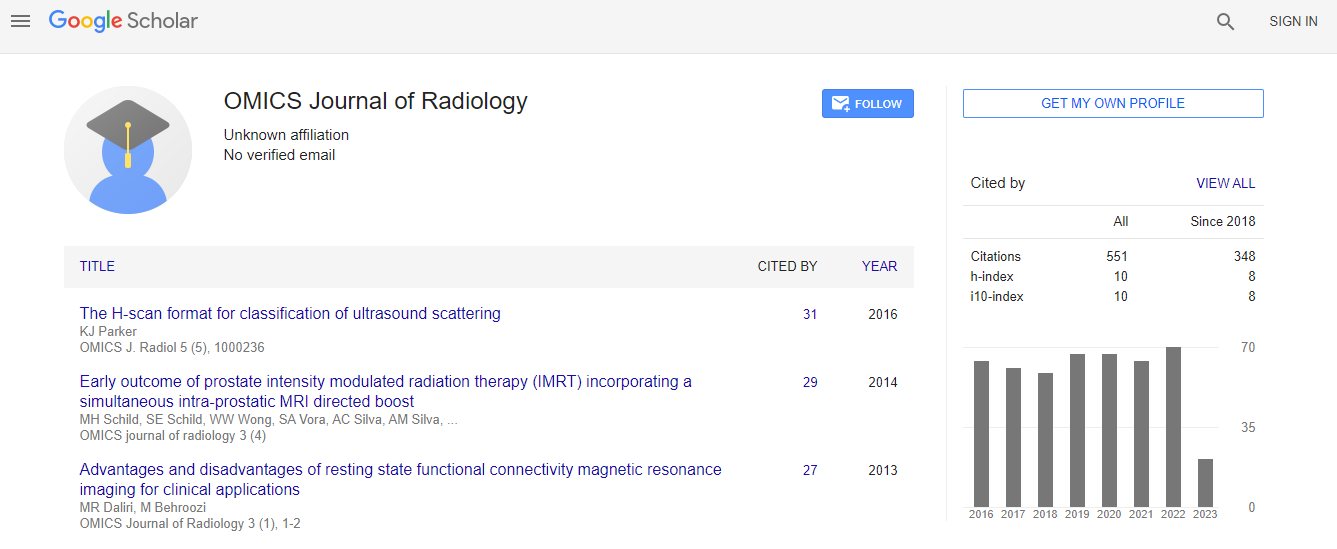
| Citation: Batawil NA (2015) MIBI SPECT Scan and Ultrasonography in Preoperative Imaging of Primary Hyperparathyroidism. OMICS J Radiol 4:188. doi: 10.4172/2167-7964.1000188 | |
| Copyright: © 2015 Batawil N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
Abstract
Objectives: In patients who have parathyroid adenoma, combination of ultrasonography and technetium Tc 99m sestamethoxyisobutylisonitrile scan (also called sestamibi or MIBI scan), which allows anatomic and functional information about parathyroid adenomas, is used commonly to maximize operative cure. The sensitivity of MIBI scan may be increased by adding single photon emission computed tomography (SPECT) and computed tomography (CT) as a combined MIBI-SPECT CT scan. We assessed the accuracy of ultrasonography and parathyroid MIBISPECT scan in detecting parathyroid adenoma and evaluated the potential benefit of the combined protocol of ultrasonography and MIBI-SPECT parathyroid scan.
Methods: In 58 patients who had biochemical evidence of primary hyperparathyroidism, we retrospectively reviewed the preoperative ultrasonography and MIBI-SPECT scans. The results of these studies were correlated with surgical findings.
Results: In the 58 patients, surgery showed that 43 patients (74%) had solitary parathyroid adenoma. The sensitivity, specificity and accuracy of MIBI-SPECT for parathyroid adenoma was (72%,80%,74%) and for ultrasonography (53%,60%,55%) respectively. The highest sensitivity is noted with the combination of MIBI-SPECT and ultrasonography (79%), . 9 adenomas (21%) were missed by both modalities. In the 20 adenomas that were missed by ultrasound 11 were detected by MIBI SPECT.
Conclusion: The MIBI-SPECT had better performance than ultrasonography for parathyroid adenoma localization. The combined MIBI SPECT and ultrasonography has the highest sensitivity for parathyroid adenoma detection (79%). An alternative strategy may be to use MIBI-SPECT initially, and to proceed to ultrasonography only in patients with negative MIBI- SPECT. This may avoid many ultrasonography procedures.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi