Research Article
Patient Specific Characteristics Are an Important Factor That Determines the Risk of Acute Grade ≥ 2 Rectal Toxicity in Patients Treated for Prostate Cancer with IMRT and Daily Image Guidance Based on Implanted Gold Markers
Xiaonan Liu1, Jing Li1, Teresa Wu1, Steven E Schild2, Michael H Schild2, William Wong2, Sujay Vora2 and Mirek Fatyga2*
1School of Computing, Informatics, Decision Systems Engineering, Arizona State University, Tempe Arizona, USA
2Department of Radiation Oncology, Mayo Clinic Arizona, Phoenix Arizona, USA
- *Corresponding Author:
- Mirek Fatyga
Department of Radiation Oncology
Mayo Clinic Arizona, Phoenix Arizona
Phoenix, AZ 85054-4502, USA
Tel: 480- 301-5979
E-mail: fatyga.mirek@mayo.edu
Received Date: April 20, 2016; Accepted Date: June 07, 2016; Published Date: June 13, 2016
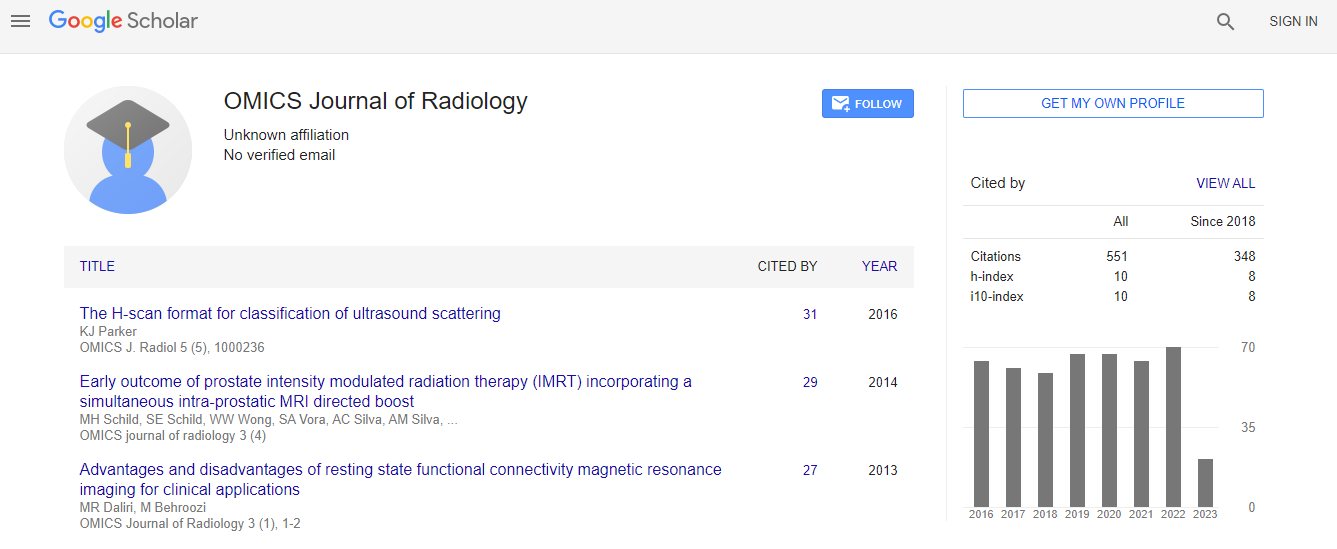
Citation: Liu X, Li J, Wu T, Schild SE, Schild MH, et al. (2016) Patient Specific Characteristics Are an Important Factor That Determines the Risk of Acute Grade ≥ 2 Rectal Toxicity in Patients Treated for Prostate Cancer with IMRT and Daily Image Guidance Based on Implanted Gold Markers. OMICS J Radiol 5:225. doi:10.4172/2167-7964.1000225
Copyright: © 2016 Liu X, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To model acute rectal toxicity in Intensity Modulated Radiation Therapy (IMRT) for prostate cancer using dosimetry and patient specific characteristics.
Methods: A database of 79 prostate cancer patients treated with image guided IMRT was used to fit parameters of Lyman-Kutcher-Burman (LKB) and logistic regression Normal Tissue Complications Probability (NTCP) models to acute grade ≥ 2 rectal toxicities. We used a univariate regression model to find the dosimetric index which was most correlated with toxicity and a multivariate logistic regression model with machine learning algorithm to integrate dosimetry with patient specific characteristics. We used Receiver Operating Characteristics (ROC) analysis and the area under the ROC curve (AUC) to quantify the predictive power of models.
Results: Sixteen patients (20.3%) developed acute grade≥2 rectal toxicity. Our best estimate (95% confidence interval) of LKB model parameters for acute rectal toxicity are exponent n=0.13 (0.1-0.16), slope m=0.09 (0.08–0.11), and threshold dose TD50=56.8 (53.7-59.9) Gy. The best dosimetric indices in the univariate logistic regression NTCP model were D25% and V50Gy. The best AUC of dosimetry only modeling was 0.67 (0.54, 0.8). In the multivariate logistic regression two patient specific variables were particularly strongly correlated with acute rectal toxicity, the use of statin drugs and PSA level prior to IMRT, while two additional variables, age and diabetes were weakly correlated. The AUC of the logistic regression NTCP model improved to 0.88 (0.8, 0.96) when patient specific characteristics were included. In a group of 79 patients, 40 took Statins and 39 did not. Among patients who took statins, (4/40)=10% developed acute grade ≥2 rectal toxicity, compared to (12/39)=30.8% who did not take statins (p=0.03). The average and standard deviation of PSA distribution for patients with acute rectal toxicity was 5.77 2.27 tox PSA = ± and it was 9.5 7.8 notox PSA = ± for the remainder (p=0.01).
Conclusions: Patient specific characteristics strongly influence the likelihood of acute grade ≥ 2 rectal toxicity in radiation therapy for prostate cancer.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi