Migration and Related Epidemiological Risk Factors Associated with Unavoidable Increments of Tuberculosis Morbid Indicators in Kuwait
Received: 21-Apr-2014 / Accepted Date: 26-Jul-2016 / Published Date: 30-Jul-2016 DOI: 10.4172/2161-1165.1000257
Abstract
“5 million lives can be saved between now and 2015 by fully funding and implementing the Global Plan to Stop TB 2011-2015” (WHO 2011). Introduction: Tuberculosis (TB) continues to be a major public health problem and is associated with worldwide demographic infra-structure changes, which can reflect the disease prevalence and mortality especially among foreign-born residents and new immigrants from TB-endemic regions. The World Health Organization (WHO) has considered tuberculosis to be a global, contagious, epidemic, public health emergency since 1993. Objective: This work assesses and retrospectively presents a descriptive analysis the epidemiological trends of tuberculosis morbid indicators and related fatality by gender and nationality which is associated with international migration into Kuwait. Methodology: Demographic data were obtained from the authorized Kuwaiti national records over a 29-year-period (1984-2012). Results: Non-Kuwaitis had higher TB morbidity and mortality rates than Kuwaitis and also male rates were comparatively higher than those of female. Since 2004 re-increment of all morbid trends was observed. Conclusions: TB became a disease of specific subgroups in Kuwait (low incidence country) which requires focused interventions on expatriates from various ‘at risk’ geographic localities. Overcoming higher rates of TB morbidity and mortality of non-Kuwaitis’ in comparison to those of Kuwaitis’ constitute a public health challenge that deserves urgent evaluation, developing a new health policy and re-structuring of the tuberculosis control program to reduce the burden of tuberculosis in Kuwait.
Keywords: Tuberculosis; Mortality; Morbidity; Migration
Introduction
Tuberculosis (TB) is a contagious and the highest bacterial disease (predominantly caused by Mycobacterium tuberculosis (MTB)) that is considered to be one of the deadliest infectious diseases worldwide. It is estimated that one third of the world’s population (two billions) are infected and carrying the causal agent airborne MTB bacillus in noneradicated intra-granulomatous foci as latent tuberculosis infection (LTBI). Tuberculosis major impacts and fatality on global health grasp international attention [1]. Tuberculosis remains one of the biggest killers of the human race resulting annually in 9.4 million new cases of active tuberculosis (including 3.3 million women) and 3 million TBrelated deaths representing an incidence of 137 cases per 100,000 population and 14 million cases in 2009 [2] .
Worldwide, TB characterized as disease of poverty and low income populations. Estimations of more than 90% (up to 8 million) of total TB cases and increase mortalities of more than half of all deaths (2 million) are occurring in Asia within the developing TB endemic countries mainly India and China [3]. But while TB has gradually disappeared from the health agenda of countries in the developed world, tuberculosis has re-emerged as a public health concern in highincome countries in the last few decades associated with migration [4]. For example the total population of Kuwait (nearly 3.6 million) is composed of Kuwaitis: non-Kuwaitis in ratio of 1:2.5, and is considered a good example of a non-endemic country with a TB incidence of 35 per 100,000 populations [5] provided that the WHO-Kuwait ‘National TB programme budget’ reached US$ 7 million [6].
Migration Impacts on Tuberculosis Morbidity and Mortality
All over the world, countries are exposed to voluntary migration for labor and/or family reunion migrations [7]. Mass migration from broken health system region directly changes the epidemiology of communicable infectious diseases and non-communicable conditions in the TB low-incidence countries [8,9]. Immigration demographic and ethnicity statistics reveals that Asians, Blacks, and Hispanics usually overcome the greatest burden of infectious diseases such as tuberculosis with predominance of anti-TB resistant strains in UK since 1999, where ∼40% were from Indian, Pakistani and Bangladeshi origins and ∼20% from black African ethnicity versus 29% from white ethnic groups[10].
Expatriates have outnumbered Kuwaiti nationals for the last decades [11] especially after six-month Gulf war during 1990-1991 [12]. Since 1975 the central reason for non-Kuwaitis’ predominance (outnumbering) is participation in the labor force. Kuwait's overall populations are Arabs (60% including both Kuwaiti and non-Kuwaiti Arabs), 35% are Asian (mostly from the Indian subcontinent) [11,13].
Strengths and Limitations of Kuwait Registration Policy System
Kuwait an open country to immigrants with daily average of 500 to 700 newly entering and should be registered before the end of onemonth temporary viza. Strict and high-quality notification system with high coverage system and notification rates through legal laws allows any suspected infectious disease such as TB case to be only diagnosed and managed in the official governmental hospital routes without missing or losing TB cases, which is comparable to most developed countries [14].
ates (CDR’s) of TB which equals the proportion of notified new and relapse cases reaches 100% in 2009 [15] and 88% in 2012 [6] compared to only 70% in the South East Asia Region[16,17] or to 63% (only 5.8 million) TB notified cases in 2009 worldwide [2].
Limitations appear because of the absence of a central database able to differentiate newly diagnosed (incident) cases from old re-admitted cases i.e. re-admission is considered as a new case.
Under-estimation and under-notification negative impacts due to TB stigmatization lead to the preference of some residents, even Kuwaitis, to be managed outside the country, and such cases are missed with absent diagnosis in the issued death certificate. Wrong diagnosis due to language barriers and miss-diagnosis are faced e.g. in prison or desert field workers.
Aims and Objectives
Assess the morbidity and mortality indicators of tuberculosis disease and related migration risk factors of all residents in Kuwait during the last three decades.
Methodology
Tuberculosis data between 1984 and 2012 were collected from the annual publications of the National Center for Health Statistics (NCHS). Morbidity and mortality rates were calculated accordingly using Microsoft Office Excel 2013 (©Microsoft Corp etc) and figures were drawn using Microsoft Office Excel 2007 (©Microsoft Corp etc).
The direct indicators of the burden of tuberculosis are morbidity or prevalence (indicating the number of people suffering from the disease at a given point of time) and mortality or death rate (indicating the number dying in population at risk each year).
Both of these rates represent the TB health status and health service burden in Kuwait population which can be targeted for control programmes. Therefore indirect indicators were calculated of tuberculosis morbidity as percentages of; 1-tuberculosis hospital discharges per 1,000 hospital discharges, and as percentages of tuberculosis mortality; 1-tuberculosis deaths per 1,000 hospital discharges and their related 2-case fatality rate (equals ratio of number TB deaths to number of TB diagnosed (or discharged) cases).
Population morbidity and mortality in Kuwait can be identified through study of all residents who are influenced by infectious diseases and by the endemic tuberculosis of the foreign migrant’s according to the geographic distributions and related socio-demographic backgrounds. Tuberculosis case admission is taken according to the disease defining characteristics for any individual within a time period, where the hospital occurs for implementation of diagnostic-relatedprocedures.
Tuberculosis morbidity rates representing tuberculosis prevalence over a 29-year-period (1984-2012) in Kuwait were calculated as percentages of tuberculosis hospital discharges per 1,000 population (almost equal to prevalence) and tuberculosis hospital discharges per 1,000 hospital discharges (which represents the burden on hospitals). All rates been tested for two demographic population characteristics (gender and nationality), and were calculated as represented as the following;
Results
Kuwait shows a similar worldwide picture for all TB mortality and morbidity trend results for non-endemic countries, representing the TB burden and overloads on Ministry of Health and Kuwait population.
During the 29-years period studied from governmental hospital records, total TB discharges were 12,866 (out of average 3,957,797 total hospital discharges) and total TB deaths were 564 (out of average 108,660 TB discharges). The average rates of TB declined steadily for the last three decades among all Kuwait population; males, females, natives, and immigrants.
Since 1991 the estimated TB morbidity and mortality rates reveal non-Kuwaiti’s predominance, and only declined at a slow rates similar to worldwide and the South East Asian region [15,18]. Contrary the case fatality rates show Kuwaiti’s increment and Kuwaiti males override in particular [19].
Trends in tuberculosis morbidity
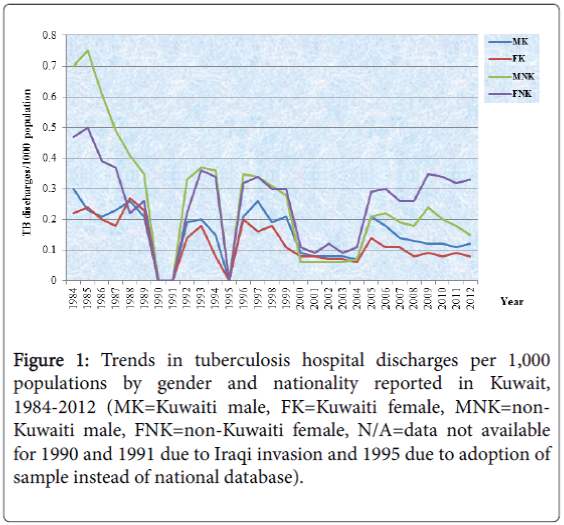
Tuberculosis hospital discharges per 1,000 total populations during a 29-year-period (1984-2012): The overall morbidity trends of TB discharges per 1,000 populations have declined gradually from 0.49 in 1984 to 0.29 in 1989. Post Iraqi invasion a steady continuous fluctuation trend reaching average of 0.26 until 1999, then declined to 0.08 per 1,000 populations until 2004 is observed.
A sudden increase in the TB morbidity trend has occurred since 2005 (0.22 per 1,000 populations) and continued almost at the same rate until 2009.
The highest calculated rate after invasion was 0.29/1000 population in 1993, 1996 and 1997, whereas, the lowest value rate of 0.07/1000 population was demonstrated in 2001, 2003 and 2004.
Another respective stable decrement was revealed since 2010 (0.2), 2011 (0.19) and 2012 (0.18). In general, males and non-Kuwaitis’ rates were predominantly higher than those of their counterparts (Figure 1).
Figure 1: Trends in tuberculosis hospital discharges per 1,000 populations by gender and nationality reported in Kuwait, 1984-2012 (MK=Kuwaiti male, FK=Kuwaiti female, MNK=non- Kuwaiti male, FNK=non-Kuwaiti female, N/A=data not available for 1990 and 1991 due to Iraqi invasion and 1995 due to adoption of sample instead of national database).
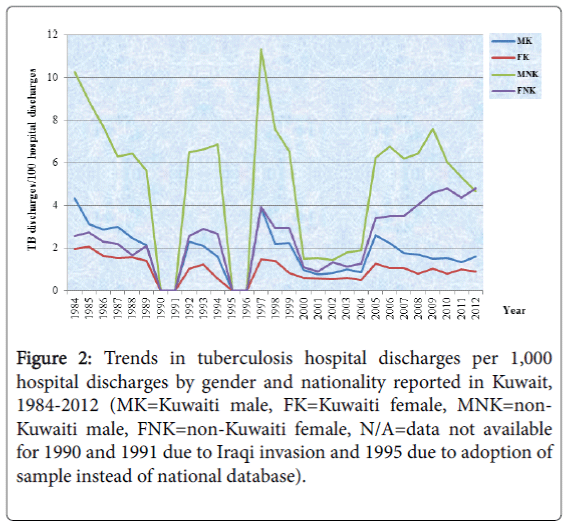
Tuberculosis hospital discharges per 1,000 total hospital discharges during a 29-year-period (1984-2012): In general there was a decline between 1984 and 2004, with two steady periods; the first was between 1989 and 1996 and the second one, at a lower level, between 2000 and 2004. Then the trend sharply increased until 2012. All non-Kuwaitis’ rates have been continuously rising since 2005, where males reached 7.59 and females 4.61 in 2009, compared with average rates of only 1.5 for Kuwaitis. Non-Kuwaitis always had higher rates (nearly double) than those of Kuwaitis and also male rates were comparatively higher (nearly double) than those of females. The highest calculated rates after the invasion were 4.54 in 1997 compared with the lowest rate of 0.89 in 2001, whereas sudden increments to average rates of 3.1 since 2005 until 2012 was noticed (Figure 2).
Figure 2: Trends in tuberculosis hospital discharges per 1,000 hospital discharges by gender and nationality reported in Kuwait, 1984-2012 (MK=Kuwaiti male, FK=Kuwaiti female, MNK=non- Kuwaiti male, FNK=non-Kuwaiti female, N/A=data not available for 1990 and 1991 due to Iraqi invasion and 1995 due to adoption of sample instead of national database).
Trends in tuberculosis mortality (1984-2012)
Tuberculosis mortality status representing the tuberculosis deaths over a 26-years-period in Kuwait. All rates been tested also for two demographic population characteristics (gender and nationality), and were calculated as represented as the following:
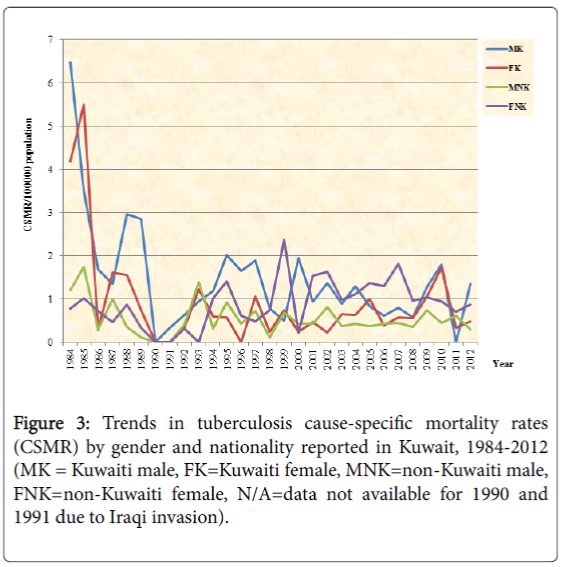
Tuberculosis cause-specific mortality rate per 100,000 populations (TB CSMR/100 000 population) during a 29-years-period (1984-2012): Tuberculosis cause-specific death rate is defined as the annual total number of deaths from tuberculosis per 100,000 mid-year population at risk.
The overall mortality trends reveal tremendous sharp declines of TB cause-specific mortalities per 100,000 populations in all CSMR annual rates from 2.63 in 1984 to 0.64 in 1989. Post-1990 a steady continuous fluctuating trend reached averages of less than 1 until 2009. A sudden reversal with of double increase in TB morbidity trends has occurred since 2008 from 0.56 to 1.76 in 2011 for Kuwaitis’ mortalities and 0.54 to 0.85 for non-Kuwaitis per 1,000 populations. The highest calculated rate after invasion was 1.76/100 000 populations in 2010, whereas the lowest value of 0.39/100,000 populations was calculated in 1998. Non- Kuwaiti female rates averaged around one/100,000 populations after no cases in 1993. In general, male and Kuwaitis’ rates were predominantly higher than those of their counterparts (Figure 3).
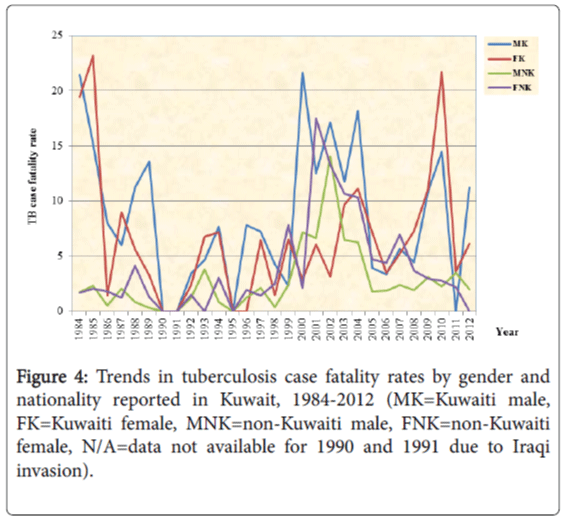
Tuberculosis case fatality rate (TB deaths per 100 tuberculosis hospital discharges; TB deaths/100 TB hospital discharges) during a 29-years-period (1984-2012): On average, the overall trends of TB case fatality rates were below 5% of discharges during the 29-years-period, with intervene by a sharp incline of average 10% between 2000 and 2004, followed by decline to rates below 5%. Kuwaiti’s suffered higher case fatalities than non-Kuwaitis. There was a sharp increase in Kuwaiti fatalities from 5.56% in 2008 to 17.39% in 2010 then to 9.17 during 2012, compared with a 0.5% increase for non-Kuwaitis (from 2.65% in 2008 to 3.06% in 2009). Males Kuwaiti’s have markedly higher case fatalities than females (Figure 4).
Discussion
Globalization of international public health threats and associated re-emerging human TB is associated with population mobilities due to contact-exposure phenomenon [20]. ‘’Fear of TB infection’’ has serious socioeconomic and negative health consequences from seeking treatment in low social class people [21].
Tuberculosis disease is still unable to be eradicated due to ‘continued’ immigration and international travel such as tourism, students, asylum seekers or economic laborers [22]. Reliable information and improved TB surveillance system through obligatory reporting of any suspected MTB case such as in Kuwait plays a role in development of national and international health policies for prevention and control, through reliable diagnostic and management activities [23]. Each country needs defining the local epidemiological demographics to benefit from their local TB control programs. The total morbidity and mortality rates (including the incidence and prevalence rates) increased in the last decade especially in the Kuwaiti groups without actually known cross-transmission routes, which might be due to new exposures to different risk factors, and similar findings were recently achieved [24,25].
Trend decrements
Decline of all tuberculosis morbidity and mortality indicators were in general due to international concerns to tackle TB pandemic and the extraordinary progress in the knowledge of infectious disease in addition to the discovery of effective anti-TB therapy and effective vaccines before four decades with widespread researches toward MTB biology. Decrement of TB incidence is predominantly due to decline in recent MTB transmissions correlated to different molecular epidemiology MTB strains [25,26]. At Kuwait community levels and through international collaborations a coordination and translation of National Plan and Strategies within all health facilities/services play a role in lower TB morbid catastrophe. Efficiency of health care system through raising knowledge and experience of trained personnel in medical care with high index of suspicion for rapid case detection and TB disease diagnoses. In Kuwait, through strict legislative case notifications of effective immigrant screening and development of electronic reporting systems within a developed and availability and affordability (free diagnosis and therapy) of the health care service could reach highest case detection levels of TB diagnoses and management follow-ups such as CDR reaches 100% compared to only mild reduction in the ‘estimated TB indicators’ per 100,000 population in majority of endemic regions [5]. Improved living conditions both in country of origin and newly occupied regions (especially in the first few years) and the strict use of antibiotics in the 20th Century add to the decline in the global TB pandemic decrease the incidence of TB [22].
Worldwide improved socio-economic conditions and human life expectancy would add to substantial rate decrements [27] in addition to advances of population general hygiene and preventive measures with lower overloads of health services in comparison to underdeveloped countries still facing higher TB prevalence’s and therapy resistance due to ineffective health services and cultural incorporations [28]. TB incidence fall as people growing in urban areas [29]. Internationally, the slow decrements in all TB rate indicators largely attributed to attributed to persistence of latent inactive and active TB in foreigners’, foreign-born populations and racial and ethnic minorities [18].
Trend increments
Worldwide facing problem is lack of screening and wrong assumptions of normal and free immigrants from infectious diseases in addition to delayed presentation with under-reporting of TB cases in the over-burden health sectors play a role in incidence slow declines followed by new increments due to TB transmission/spreads which necessitate raising education and TB awareness. Improvements in laboratory MTB diagnostic specificity can be directly related to increased TB incidence [30-32], or reflecting increased public awareness rather than increased occurrence due to deteriorating socioeconomic or living conditions [33].
Raised TB mortalities in Kuwait exploring waves of ongoing global uncontrolled immigrations. Foreign-born immigrants from Asian countries develop TB re-activations within shorter time of less than five years compared to those from other regions with lower TB prevalence [34]. After the Iraqi invasion during 1990-1991, detected growth in non-Kuwaiti’s residential foreigners and majority are coming from most vulnerable–rural populations of TB endemic regions such Asian (India, Bangladesh, Indonesia and Philippines) and African countries (Ethiopia) [11]. Also in Kuwait a new phenomenon of living in settlement with small closed flats increased since the 1990’s, and each house with at least one housemaid with predominance from Asian endemic countries (India, Indonesia, Bangladesh, Nepal, Sri Lanka, Philippine) exposing the population sectors to inadequate fresh air is continuously associated with total population rate increments [33]. Environmental conditions and proximity with contagious index case (>8 hours) complicates TB control programs’ [35,36]. Human movement and migration are both important risk factors for transmitting airborne infectious particles [37].
Even with improvements in the political, economical and community efforts (e.g. researches), still TB remains a worldwide unresolved global health problem. TB is associated with low income countries and deprived regions were overcrowding, poverty and malnutrition are known. Also TB morbid rates are increased in developed countries due to immigrations and social inequalities related to co-existing risk factors such as smoking, DM, cardiovascular diseases, alcohol/drug addiction and HIV infections [38]. Associated risk-factors for development of pulmonary tuberculosis are interrelating and contributing to risk of TB infection and others with progression to TB disease. Differences of population geographic and their direct-and indirectly-related epidemiologic and demographicrelated risk factors, including:
Socio-economic-cultural factors
TB disease is directly related to community socio-economic conditions and threatens low-income populations. Transmission of TB is well established with societal forces such as poverty and social deprivation, urbanization with overcrowded (exposure) living conditions, migration and unemployment (low socioeconomic conditions) with reduced health literacy, malnutrition and tobacco as TB endemic regions complicated with self-treatment and further nosocomial spreads e.g. Sub Saharan Africa and South East Asia [39].
Changes in demographic infra-structure and risk factors such as gender, place of birth, occupation and ethnic origins. As strong association between aging and TB development with common excess of TB morbid indicators [40,41]. Increased age is also at risk for TB infection with 100-fold higher than non-exposed healthy people [32]. Age is still not a major epidemiological risk factor in Kuwait, as diagnosed latent TB/TB cases are still very low. Older age reveals significant results of positive IGRAs testing, and TB is considered infectious killer of reproductive age women worldwide (annual 750,000 deaths) [42], because of higher trends in high risk groups and waning of immunity such as the elderly (particularly men) is associated with LTBI/TB longevity-reactivation and difficulties in diagnosis (e.g. non-specific presentations) added to non-compliance to treatments [18,39]. Also age is known infection social marker for children and directly affected by both community internal exposures e.g. close contact to same household and parent TB index case with/ without external exposures due to mobility outside households e.g. inside school or playground [43].
Stigmatization and socio-cultural factors such as perception and personal beliefs concerning the risks of TB evaluation and treatment have influenced by familial socio-economic structures [21]. Parent education and employment are another significant risk factor for TB infection and detected more in BCG positively vaccinated compared to non-vaccinated people [44]. Gender inequities and under-notification of women due to social, religious and financial constraints noticed in the low income countries added to higher TB morbid rates during the reproductive life period aggravate diagnostic barriers [19].
Behavioral factors
Even though years of education and higher in rural region and correlated with smoking and drinking is negatively associated with smoking and TB incidence [38,40]. Smoking is the major behavioral and occupational risk factor that is increasing all over the world and Kuwait [42]. Duration and type of smoking (bidis more risky than cigarette) is also related to higher PTB and new EPTB occurrences [40]. Passive smoking is significantly associated with increased risk for clinical TB and children exposed to passive smoking exhibit more positive TST results mainly those living with smoker households [41,45,46]. Alcohol and drug abuse is forbidden in Kuwait to be a direct related risk factor and easily the predicted epidemiological impact as the case in TB low income regions [42].
Cardiovascular diseases and diabetes mellitus and tobacco smoking habits in Kuwait increases 3-fold risk of MTB re-activation and bacterial infection/transmissions [47,48]. Diabetes mellitus is considered in Kuwait the 7th all over the world which is increasing without control and is directly impairs both innate and adaptive immune responses necessary to resist MTB proliferation. Diabetesnutrition wise revealed rises in the annual number of active TB cases in people with diabetes by 46% from 163,000 in 1998 to 224,000 in 2008, and the corresponding TB incidence per person with diabetes by 24% (one million) [29,47]. Nutrition, body mass index, ethnicity, employment and family history of TB are all related [16]. Other accompanied health condition such as pregnancy and under-nutrition add risks toward female fatality predominance. Smoking is associated with active tuberculosis treatment non-adherence and tuberculosis infection relapses and delays in recovery [49].
Biological-physiological factors
Host-related genetic factors vary between cases and community controls has been validated through family-based association studies to improve understanding of biology and MTB transmission which explain various risk factors like; 1-source of infectivity, 2-intensity of TB infection, and 3- infection susceptibility [50].
Morbid indicators were higher in males due to frequent and recent contacts inside (household) and frequent outside (non-household) environments and various levels of exposures [19]. Raised mortality and fatality can be related to the predominance of foreign-born genotypic and drug-resistant strains related to differences in clinical picture in which the Kuwaiti people are sensitive and developing pulmonary TB primarily than extra-pulmonary complications [9].
In Kuwait reversal (shift) of male predominance to female since 1999 having higher mortality and fatality rates might be due to predominance of female immigrants employed for in-house occupation (job) as housemaid and cooker with overcrowding and prolonged exposure-contacts stigma-social anti behavior [9,21,51] in contrast to male predominance all over the world revealed by Neyrolles and Ouintana-Murci study [52] which can be as research recommendations for the needs of Kuwaiti’s environment to household immigrants.
TB prevention and control programmers require linked coordination’s among scientists such as epidemiologists and governmental funding supports such as researches [38]. Clinicians should elicit a migration history is important if correlated to exposure in their country of origin, will facilitate early detection and treatment of LTBI/TB infections [53]. Genetic susceptibility as various geographic difference and rural-urban cluster strains and related innate response differences which would complicate TB managements and elimination for Kuwaiti patients should be investigated [33].
Conclusion
Kuwait infrastructure has changed substantially and awareness of socio-demographic changes may speed-up diagnosis of tuberculosis. The annual rise and TB burdens of non-Kuwaiti population are overloading the health care system and medical service. Overcoming higher rates of TB morbidity of non-Kuwaitis’ in comparison to those of Kuwaitis’ population constitute a serious public health threat that deserves urgent evaluation and re-structuring of the tuberculosis control program through qualified surveillance system and strict quantifying and minimizing TB stigmatization.
Recommendations
Declining and increment advances in the overall national TB rate coupled with the persistence of disproportionately high TB rates among foreign-born non-Kuwaitis’ suggest the need for a re-doubling of public health efforts aimed at the eradication of TB in Kuwait through verification of new screening guidelines for new cost-effective diagnostic tests to control and reduce both the incidence and prevalence of TB disease, both nationally and locally, public health professionals must urgently and effectively target high-risk subpopulations through:
Screening of immigrants for TB upon arrival to Kuwait need to be improved. Public health efforts and re-enforcing awareness of TB risks, transmission, diverse manifestations and can limit diagnostic delays in the health services and improve TB control.
Policy makers should consider expansion of immigrants screening programs especially at entry points.
Reduction of structural and behavioral barriers in health systems by filling the gap of lack of knowledge regarding migrants' exposure to risk factors, morbidity, and psychosocial needs.
Using Kuwait electronic health records (EHRs) is feasible and promising for prospective TB surveillance and even detection of latent TB infection such as high-risk population.
References
- LoBue PA, Enarson DA, Thoen CO (2010) Tuberculosis in humans and animals: an overview. Int J Tuberc Lung Dis 14: 1075-1078.
- WHO (2009) Global Tuberculosis Control: epidemiology, strategy, financing. WHO report?.
- WHO (2010a) Communicable Diseases Tuberculosis TB in South-East Asia (Global Tuberculosis Control; WHO Reports: 2001-2008).
- Long Q, Li Y, Wang Y, Yue Y, Tang C, et al. (2008) Barriers to accessing TB diagnosis for rural-to-urban migrants with chronic cough in Chongqing, China: a mixed methods study." BMC Health Services Research 8:202.
- Svensson E, Millet J, Lindqvist A, Olsson M, Ridell M, et al. (2011) Impact of immigration on tuberculosis epidemiology in a low-incidence country. Clinical Microbiology and Infection 17: 881-887.
- Crofts JP, Gelb D, Andrews N, Delpech V, Watson JM(2008) Investigating tuberculosis trends in England. Public Health 122: 1302-1310.
- NCHS (1984-2009) HEALTH, KUWAIT: annual publications 1984-2012. National Center for Health Statistics-Ministry of Health.
- Behbehani N, Abal A, Al-Shami A, Enarson DA (2002) Epidemiology of tuberculosis in Kuwait from 1965 to 1999. Int J Tuberc lung Dis 6: 465-469.
- Shah NM (2007) Migration to Kuwait: Trends, Patterns and Policies. Migration and Refugee Movements in the Middle East and North Africa. The Forced Migration and Refugee Studies Program. The American University in Cairo 23-25.
- Horne NW (1984) Problems of tuberculosis in decline. British Medical Journal 288: 1249-1251.
- Pakasi TA, Karyadi E, Dolmans WM, van-der-Meer JW, Velden K (2009) Malnutrition and socio-demographic factors associated with pulmonary tuberculosis in Timor and Rote Islands, Indonesia.Int J Tuberc Lung Dis 13: 755-759.
- Jassal MS, Bishai WR (2010) Epidemiology and challenges to the elimination of global tuberculosis. Clinical Infectious Diseases 3: 156-164.
- Holmes CB, Hausler H, Nunn P (1998) A review of sex differences in the epidemiology of tuberculosis. Int J Tuberc Lung Dis 2: 96-104.
- McCarthy OR (1984) Asian immigrant tuberculosis-the effect of visiting Asia. British Journal of Diseases of the Chest 78: 248-253.
- Courtwright A, Turner AN (2010) Tuberculosis and stigmatization: pathways and interventions. Public Health Reports 125: 34-42.
- Scotto G, Fornabaio C, Prato R, Saracino A, Tartaglia A, et al. (2009) Tuberculosis and immigrants: a SIMIT (Italian Society of Infectious Diseases) clinical, epidemiological multicentric research investigation. New Microbiologica 32: 39-47.
- Schneider D, McNabb SJ, Safaryan M, Davidyants V, Niazyan L, et al. (2010) Reasons for delay in seeking care for tuberculosis, Republic of Armenia, 2006-2007. Interdisciplinary Perspectives on Infectious Diseases.
- Lim LKY, Li-Hwei S, Wah W, Bin-Eng ChC, Li-Yang H, et al. (2013) Molecular Epidemiology of Mycobacterium tuberculosis Complex in Singapore, 2006-2012. PLoS One 8: e84487.
- Suwanpimolkul G, Jarlsberg LG, Grinsdale JA, Osmond D, Kawamura LM, et al. (2013) Molecular epidemiology of tuberculosis in foreign-born persons in San Francisco. American Journal of Respiratory and Critical Care Medicine 187: 998-1006.
- Iñigo J, García-de-Viedma D, Arce A, Palenque E, Herranz M, et al. (2013) Differential findings regarding molecular epidemiology of tuberculosis between two consecutive periods in the context of steady increase of immigration. Clinical Microbiology Infections 19:292-297.
- Horsburgh CR,O'Donnell M, Chamblee S, Moreland JL, Johnson J, et al. (2010) Revisiting rates of reactivation tuberculosis: a population-based approach. American Journal of Respiratory and Critical Care Medicine 82: 420-425.
- Oxlade O, Schwartzman K, Behr MA, Benedetti A, Pai M, et al. (2009) Global tuberculosis trends: a reflection of changes in tuberculosis control or in population health?. The International Journal of Tuberculosis and Lung Disease 13: 1238-46.
- Dye C, Trunz BB, Lonnroth K, Roglic G, Williams BG (2011) Nutrition, diabetes and tuberculosis in the epidemiological transition. PLoS ONE 6: e21161.
- Hardy AB, Varma R, Collyns T, Moffitt SJ, Mullarkey Cet al. (2010) Cost-effectiveness of the NICE guidelines for screening for latent tuberculosis infection: the QuantiFERON-TB Gold IGRA alone is more cost-effective for immigrants from high burden countries. Thorax 65: 178-180.
- Legesse M, Mamo GAG, Medhin G, Bjune G, Abebe F (2011) Community-based cross-sectional survey of latent tuberculosis infection in Afar pastoralists, Ethiopia, using QuantiFERON-TB Gold In-Tube and tuberculin skin test. BMC Infectious Diseases 11:89.
- Pai M, Gokhale K, Joshi R, Dogra S, Kalantri S, et al. (2005) Mycobacterium tuberculosis infection in health care workers in rural India: comparison of a whole-blood interferon gamma assay with tuberculin skin testing. The Journal of the American Medical Association 293: 2746-2755.
- Ladefoged K, Rendal T, Skifte T, Andersson M, Soborg B, et al. (2011) Risk factors for tuberculosis in Greenland: case-control study. The International Journal of Tuberculosis and Lung Disease 15: 44-49.
- Mulder C, Klinkenberg E, Manissero D (2009) Effectiveness of tuberculosis contact tracing among migrants and the foreign-born population. Euro Surveillance.
- Al-Jahdali H, Memish ZA, Menzies D (2003) Tuberculosis in association with travel. International Journal of Antimicrobial Agents 21: 125-130.
- Demkow U, Broniarek-Samson B, Filewska M, Lewandowska K, Maciejewski J, et al. (2008) Prevalence of latent tuberculosis infection in health care workers in Poland assessed by interferon-gamma whole blood and tuberculin skin tests. Journal of Physiology and Pharmacology 6: 209-217.
- Leung WT, Sze-To GN, Chao CY, Yu SC, Kwan JK (2013) Study on the interzonal migration of airborne infectious particles in an isolation ward using benign bacteria. Indoor Air 23: 148-161.
- Millet JP, Moreno A, Fina L, del Baño L, Orcau A, et al. (2013) Factors that influence current tuberculosis epidemiology. European Spine Journal 4: 539-48.
- Neilson AA, Mayer CA (2010) Tuberculosis-prevention in travelers. Australian Family Physician 39: 743-750.
- Gajalakshmi V, Peto R (2009) Smoking, drinking and incident tuberculosis in rural India: population-based case-control study. International Journal of Epidemiology 38: 1018-1025.
- Kolappan C, Gopi PG, Subramani R, Narayanan PR (2007) Selected biological and behavioural risk factors associated with pulmonary tuberculosis. The International Journal of Tuberculosis and Lung Disease 11: 999-1003.
- Rao VG, Gopi PG, Bhat J, Yadav R, Selvakumar N, et al. (2011) Selected risk factors associated with pulmonary tuberculosis among Saharia tribe of Madhya Pradesh, central India. European Journal of Public Health pp: 271–327.
- Langenskiold E, Herrmann FR,Luong BL, Rochat T, Janssens JP (2008) Contact tracing for tuberculosis and treatment for latent infection in a low incidence country. Swiss Medical Weekly 138: 78-84.
- Soysal A, Millington KA, Bakir M, Dosanjh D, Aslan Y, et al. (2005) Effect of BCG vaccination on risk of Mycobacterium tuberculosis infection in children with household tuberculosis contact: a prospective community-based study. Lancet 366: 1443-1451.
- Kolappan C, Gopi PG (2002) Tobacco smoking and pulmonary tuberculosis. Thorax 57: 964-966.
- Lin HH, Ezzati M, Murray M (2007) Tobacco smoke, indoor air pollution and tuberculosis: a systematic review and meta-analysis. PLoS Medicine 4: e20.
- Jeon CY, Murray MB (2008) Diabetes mellitus increases the risk of active tuberculosis: a systematic review of 13 observational studies. PLoS Medicine 5: e152.
- Wen CP, Chan TC, Chan HT, Tsai MK, Cheng TY, et al. (2010) The reduction of tuberculosis risks by smoking cessation. BMC Infectious Diseases 10: 156.
- Lin HH, Ezzati M, Chang HY, Murray M (2009) Association between tobacco smoking and active tuberculosis in Taiwan: prospective cohort study. American Journal of Respiratory and Critical Care Medicine 180: 475-480
- Lienhardt C, Fielding K, Sillah JS, Bah B, Gustafson P, et al. (2005) Investigation of the risk factors for tuberculosis: a case-control study in three countries in West Africa. International Journal of Epidemiology 34: 914-923.
- Juniarti N, Evans D (2010) A qualitative review: the stigma of tuberculosis. Journal of Clinical Nursing 20: 1961-1970.
- Neyrolles O, Quintana-Murci L (2009) Sexual inequality in tuberculosis. PLoS Medicine 6: e1000199.
- McCarthy AE, Weld LH, Barnett ED, So H, Coyle C, et al. (2013) Spectrum of illness in international migrants seen at GeoSentinel clinics in 1997-2009, part 2: migrants resettled internationally and evaluated for specific health concerns. Clinical Infectious Diseases 56: 925-933.
Citation: AL-Harbie A, Sadek A, Picozzi K, Thrusfield M, Welburn SC (2016) Migration and Related Epidemiological Risk Factors Associated with Unavoidable Increments of Tuberculosis Morbid Indicators in Kuwait. Epidemiology (Sunnyvale) 6:257. Doi: 10.4172/2161-1165.1000257
Copyright: © 2016 AL-Harbie A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 12035
- [From(publication date): 7-2016 - Apr 27, 2024]
- Breakdown by view type
- HTML page views: 11267
- PDF downloads: 768