Research Article Open Access
Combating HIV/AIDS in Selected Sub-Saharan African Countries: Progress towards Millennium Development Goal 6
Anouk P Meijs1, Rob MPM Baltussen2, André JAM van der Ven3 and Gerhard A Zielhuis1*
1Department of Epidemiology, Biostatistics and HTA, Radboud University Nijmegen Medical Centre, Nijmegen, Netherlands
2Department of Primary and Community Care, Radboud University Nijmegen Medical Centre, Nijmegen, Netherlands
3Department of Internal Medicine, Radboud University Nijmegen Medical Centre, Nijmegen, Netherlands
- *Corresponding Author:
- Professor. GA Zielhuis
Department of Epidemiology
Biostatistics and HTA
Radboud University Nijmegen Medical Centre
133, PO Box 9101, 6500 HB Nijmegen, Netherlands
Tel: +31 24 3616975
Fax: +31 24 3613505
E-mail: g.zielhuis@ebh.umcn.nl
Received date: December 14, 2011; Accepted date: February 18, 2012; Published date: February 20, 2012
Citation: Meijs AP, Baltussen RMPM, van der Ven AJAM, Zielhuis GA (2012) Combating HIV/AIDS in Selected Sub-Saharan African Countries: Progress towards Millennium Development Goal 6. J Community Med Health Edu 2:125. doi:10.4172/jcmhe.1000125
Copyright: © 2012 Meijs AP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background:UN Millennium Development Goal six (MDG6) includes HIV/AIDS as an important target. As sub-Saharan Africa (SSA) accounts for the majority of the global HIV incidence and prevalence, the aim of this study is to describe how selected countries in SSA are on track towards reaching this goal.
Methods:Twelve countries with a generalized epidemic in SSA were selected and classified into four groups with either high or low HIV prevalence, and major or minor efforts made to realize MDG6. The five official indicators of MDG6 were used to measure progress and a comparison was made between the four groups.
Results: 1) HIV prevalence has stabilized in many countries, but this seems unrelated to the amount of efforts countries have made. 2) Access to antiretroviral therapy increased most in high prevalence countries, especially in countries that put much effort in HIV programmes. 3) School attendance was high for both orphans and non-orphans in most countries, and this was seemingly unrelated to the level of efforts. 4) Knowledge about HIV was low and hardly increased over time, although levels were higher in countries with high prevalence. 5) Condom use in high-risk sexual encounters was and remained low for most low prevalence countries. In high prevalence countries large differences in condom use between countries were observed, independent of the amount of efforts.
Conclusion:Antiretroviral therapy coverage has increased considerably over time, and several countries will reach the stated objective on this indicator. However, knowledge about HIV and promotion of safe sex is still lagging behind. A further increase of access to antiretroviral therapy seems a promising strategy to combat HIV/AIDS in the near future in SSA countries. Nevertheless, effort in educating the population can reduce the incidence of HIV by changing the population’s behaviour, which remains the best long-term strategy.
Keywords
HIV; AIDS; Millennium development goals; Sub- Saharan africa
Introduction
In the year 2000 delegates of the United Nations (UN) member states gathered at the UN headquarters to consider fundamental values essential for international relations in the twenty-first century. These values were translated into the Millennium Declaration that was signed by 189 countries [1]. The Millennium Development Goals (MDGs) originated from the Millennium Declaration in order to operationalize these values into actions for development and poverty eradication [2]. One of the eight goals is related to disease control (MDG6): combat HIV/AIDS, malaria and other diseases. For every goal, specific targets were set that should be met at the end of the year 2015. The two targets on HIV/AIDS are: have halted by 2015 and begun to reverse the spread of HIV/AIDS, and achieve, by 2010, universal access to treatment for HIV/AIDS for all those who need it. Furthermore, these targets were again divided into indicators in order to measure improvements over the years [3].
A year later, in June 2001, the United Nations General Assembly Special Session (UNGASS) on HIV/AIDS was held, resulting in the Declaration of Commitment on HIV/AIDS adopted by the same 189 UN member states. This Declaration was an additional consensus on the importance of combating HIV/AIDS, its aim is to improve the global response on AIDS and to facilitate progress towards MDG6. It consists of 25 indicators, overlapping with the ones of MDG6 [4]. An innovative partnership, the Joint United Nations Programme on HIV/ AIDS (UNAIDS), helps in managing and accomplishing this large task [5].
With 2.2 million adults and children newly infected in 2001 and 20.3 million people living with HIV by that year, sub-Saharan Africa (SSA) is the most heavily affected region in the world. Compared to an incidence of 3.1 million and a prevalence of 28.6 million globally, SSA accounts for around 70% of the total incidence and prevalence of HIV. Nevertheless, large differences in the epidemiology of HIV exist between countries. Southern Africa is the most heavily affected region bearing more than half of the total number of people living with HIV in SSA, whereas the HIV prevalence in Western Africa remains considerably low [6].
The most important routes of transmission of HIV in SSA are by unprotected heterosexual intercourse and by vertical transmission from mother to child during pregnancy and breastfeeding. Therefore, important aspects of constraining the virus is by promoting safe sexual behaviour, promoting medication during pregnancy, and making treatment available for all persons in need [6].
Although by the year 2009 the HIV prevalence in SSA has risen to 22.5 million persons, the incidence was reduced to 1.8 million. This value is considerably lower than the estimate of 2001, due to the impact of HIV prevention efforts and the natural course of the HIV epidemic. In 2009 1.3 million people in SSA died of AIDS related diseases, compared to 1.6 million during the mortality peak of the epidemic in 2004 [6]. This decrease in mortality is due to a combination of large scale availability of antiretroviral therapy and a decrease in incidence. Nevertheless, despite extensive progress, many countries will fail to achieve the goals of MDG6 according to the UNAIDS 2010 global progress report [6]. As the final year for establishing the MDGs comes closer, it is valuable to review what countries in SSA already have achieved, in the period since 2000.
The aim of this study is to describe in what way and to what extent HIV/AIDS control in selected countries in SSA is in accordance with the UN Millennium Development Goals of the year 2000. We evaluate progress against MDG6 indicators on HIV/AIDS in selected SSA countries distinguished by their level of prevalence and efforts made. We also predict the extent to which the specific targets will be realized in 2010 and 2015, under the condition that the rate of development remains the same.
Methods
Sub-Saharan Africa consists of approximately 50 countries that all have a different HIV epidemiology. Prevalence rates range between 25% in Swaziland and less than 2% in several countries in Western Africa [6]. Moreover, there are substantial differences between countries in the way their government takes action to combat the epidemic.
Contrasting countries were explored and classified into four groups; high prevalence, major effort; high prevalence, minor effort; low prevalence, major effort; and low prevalence, minor effort. With this division we aim to determine the influence of efforts resulting from MDG6 in selected SSA countries. Countries were selected based on four criteria:
1. Only countries with a generalized epidemic were selected in order to create homogenous groups. A generalized HIV epidemic is defined as an epidemic in which sexual networking of the general population is sufficient to maintain the epidemic, independent of subpopulations at higher risk. In contrast, in countries with a low level or concentrated prevalence the epidemic is mainly concentrated in specific risk groups, such as men who have sex with men, intravenous drug users, and sex workers [7].
2. The countries either have a high (>10%) or a low (<10%) HIV prevalence, based on data from 2009 compiled by UNAIDS and the World Health Organization (WHO). This was stated as the prevalence of HIV among adults aged 15-49 years, whether or not they had developed symptoms of AIDS, expressed as a percentage of the total population in that age group [8].
3. The countries have developed either major or minor efforts to treat and prevent HIV/AIDS. This criterion is based on the results of the second UNGASS indicator: Government HIV and AIDS policies, presented in the National Composite Policy Index (NCPI) [4]. The NCPI is a self-completed questionnaire and provides information on the overall policy, strategy, legal and programme implementation environments of the HIV response per country. It is divided into two parts, the first part comprises the government’s response and the second part the responses of nongovernmental sources (i.e. of civil society organizations, the United Nations and bilateral agencies). The indicator includes information on HIV prevention services and treatment (i.e. Prevention of Mother-to-child Transmission, Condom promotion, HIV testing and counselling, Harm reduction for intravenous drug users, Risk reduction for men who have sex with men, Risk reduction for sex workers, Access to antiretroviral therapy, AIDS treatment for paediatric patients, and HIV testing and counselling for patients with tuberculosis). The division in major and minor efforts was made based on the number of items scored per country.
4. The countries have freely available data on the internet on the relevant indicators, before, and especially after the year 2000 in order to be able to assess progress.
We used official indicators of MDG6 to measure the progress towards the targets on HIV/AIDS [9]:
1. HIV prevalence among population aged 15-24 years.
2. Condom use at last high-risk sex.
3. Proportion of population aged 15-24 years with comprehensive correct knowledge of HIV/AIDS.
4. Ratio of school attendance of orphans, to school attendance of non-orphans aged 10-14 years.
5. Proportion of the population with advanced HIV infection that has access to antiretroviral drugs.
UN reports and websites connected to the WHO or UNAIDS were used as data source. Only sources that provided information on the methods of data collection were used. As the definitions of the indicators are refined over time [4,10-12], the actual data that was collected could deviate from the computations mentioned in the handbook of MDG indicators [9]. If the information available was not sufficient to describe progress, similar indicators were used. When similar data was available from multiple sources, we chose the most reliable and complete data set.
Analysis
First, for all five indicators, we collected data and calculated trends over time, together with corresponding confidence intervals. We then displayed these data in graphs to show the progress over time from 1990 to 2010, drawing straight lines through the data. For every indicator a comparison was made between countries that made major and minor efforts. This was done separate for countries with high and low prevalence, in order to detect if there was a difference in progress towards the indicator depending on the amount of efforts made. When necessary, data was shown separately for men and women. The school attendance rate was shown for orphans and non-orphans separately. Finally, an estimation was made, based on the information available in the graphs, for the development of the indicators towards the year 2015.
Results
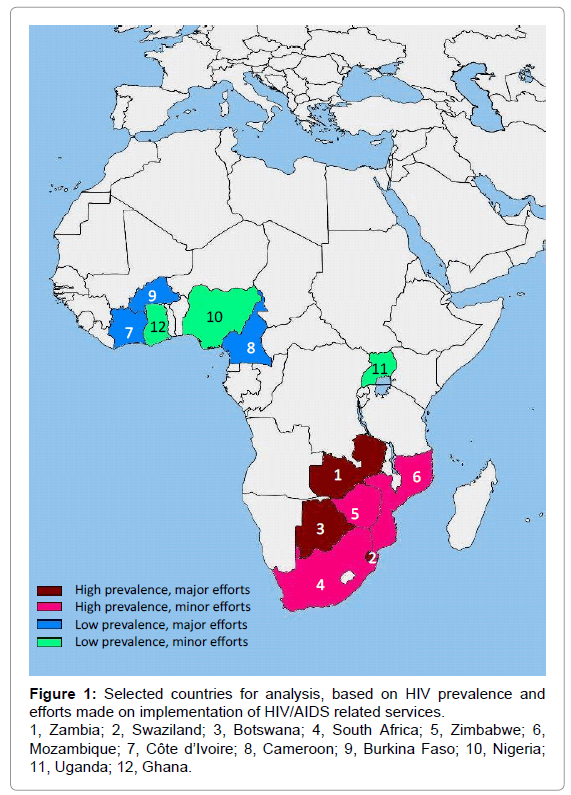
Based on the previously described criteria (generalized epidemic, high/low prevalence, major/minor efforts, and available information), 12 countries were selected for inclusion (Table 1). The countries with a high prevalence were clustered in the south of sub-Saharan Africa, whereas the countries with a low prevalence were mainly located in the north-western part of this region (Figure 1). The progress of the four groups is described per indicator:
| High prevalence | Low prevalence | |
|---|---|---|
| Major efforts | Zambia (13.5) Swaziland (25.9) Botswana (24.8) |
Côte d’Ivoire (3.4) Cameroon (5.3) Burkina Faso (1.2) |
| Minor efforts | South Africa (17.8) Zimbabwe (14.3) Mozambique (11.5) |
Nigeria (3.6) |
Table 1: Selected countries for analysis (based on HIV prevalence and the efforts made to treat and prevent HIV/AIDS), and their HIV prevalence as a percentage of the total population aged 15-49 in the year 2009.
HIV prevalence among population aged 15-24 years
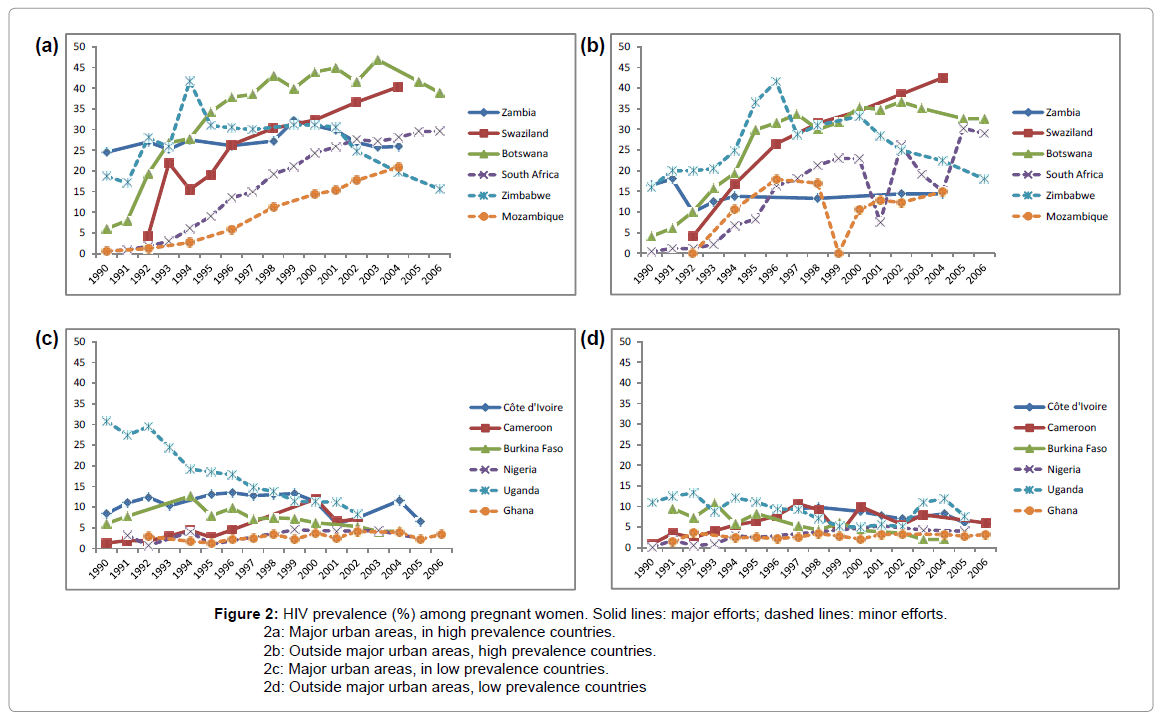
We measured this indicator as the number of pregnant women attending antenatal clinics (ANCs) in HIV sentinel surveillance sites whose blood samples tested positive for HIV, expressed as a percentage of all pregnant women whose blood was tested at ANCs in HIV sentinel surveillance sites [10]. This is in accordance with the MDG handbook except for the age limit (15-24 years) which was not specified in our data [9]. The results are shown separately for ‘major urban areas’ and ‘outside major urban areas’ (Figure 2a-2d).
Figure 2: HIV prevalence (%) among pregnant women. Solid lines: major efforts; dashed lines: minor efforts.
2a: Major urban areas, in high prevalence countries.
2b: Outside major urban areas, high prevalence countries.
2c: Major urban areas, in low prevalence countries.
2d: Outside major urban areas, low prevalence countries
In the countries with a high prevalence and major efforts, Zambia and Botswana showed a stabilization and small decrease in prevalence since 2000. In Swaziland no sign of stabilization was observed. When reviewing the NCPI (Table 2) Zambia had the most extensive HIV policy, it also was the only country where the prevalence was stable since 1990. Zimbabwe showed a strong decrease in prevalence as well, whereas the prevalence in the other two countries with minor efforts showed no signs of decrease yet.
| HIV Prevention Services Implementation | Treatment Implementation | |||||||||||||||||
| PMTCT | Condom promotion | HIV testing & counselling | Harm reduction IDU | Risk reduction men who have sex with men | Risk reduction sex workers | Antiretroviral therapy | Paediatric AIDS treatment | HIV testing & counselling TB patients | ||||||||||
| A† | B‡ | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | |
| Zambia | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Swaziland | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Botswana | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | - | ΓΆΒ?Β | - | ΓΆΒ?Β | - | - | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| South Africa | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β |
| Zimbabwe | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | - | - | - | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Mozambique | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | - | - | - | - | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? |
Abbreviations: PMTCT, Prevention of mother-to-child transmission; IDU, Intravenous drug users; TB, Tuberculosis.
* Data were derived from the UNAIDS 2010 global report. The NCPI comprises a series of questions on the progress in development and implementation of national HIV policies, strategies and laws. It is divided into two parts: one completed by government officials
(A) and one by civil society organizations and nongovernmental sources
(B). Questions are answered by yes ( ΓΆΒ?Β? ), no (ΓΆΒ?Β ), or not applicable ( - ) [4].
† A: The response by government officials on a subset of the questions on key policies, and on strategies of programmes on prevention, treatment, care and support of HIV.
‡ B: The response by civil society organizations, bilateral and multilateral organizations on key policies, and on strategies of programmes on prevention, treatment, care
and support of HIV.
Table 2: National Composite Policy Index (NCPI) results,* in high prevalence countries.
In most low prevalence countries the HIV prevalence in pregnant women was stable since 1990. For Uganda a decrease in prevalence was observed since the first survey in 1990. Little difference was noticed between the categories with major and minor efforts.
Proportion of population with advanced HIV infection with access to antiretroviral drugs
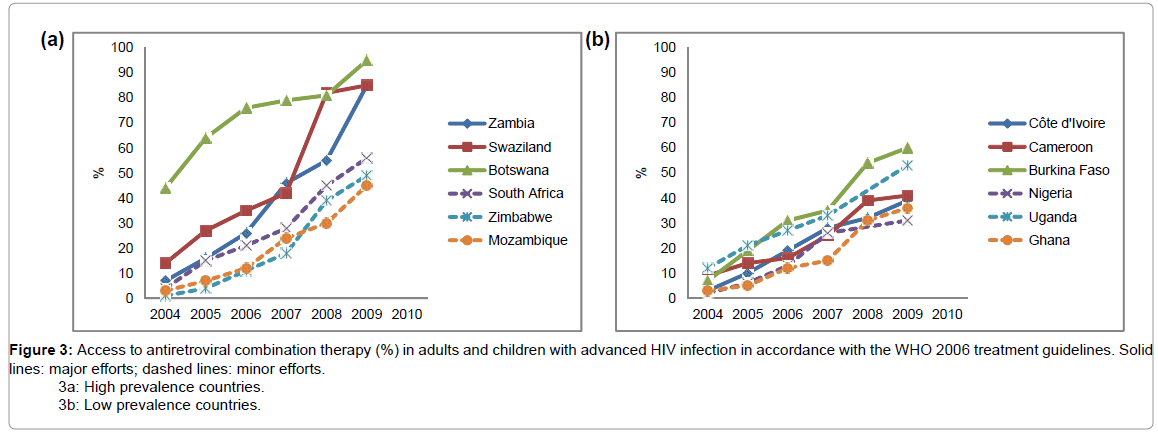
This indicator was computed as the percentage of adults and children with advanced HIV infection currently receiving antiretroviral combination therapy in accordance with the nationally approved treatment protocols (or WHO/UNAIDS standards) among the estimated number of adults and children with advanced HIV infection [4]. For all countries the WHO 2006 guidelines were used, stating that treatment should be started when CD4 cells are below 200 cells/mm3 [6,13].
In the countries with a high prevalence a large increase was observed in the access to ART (Figure 3a). All countries, except Botswana, started in 2004 with ART coverage less than 20%. In 2009, the difference in access between countries that made major and minor efforts had become larger. In all countries with major efforts more than 80% of persons in need had access to ART, compared to 40%-60% in the countries with minor efforts. NCPI data showed that ART services are implemented in all countries that made major efforts (Table 2). Of the countries with minor efforts, implementation of ART services was not completed in Zimbabwe and Mozambique, these two countries also had the lowest ART coverage.
The countries with a low prevalence also showed a large increase in access to ART since 2004, but there was less distinction between the countries that developed major and minor efforts (Figure 3b). All countries started with a 2%-12% ART coverage in 2004, and in 2009 this had increased to 31-60%. The NCPI showed that only Nigeria and Ghana lay behind on the implementation of ART services (Table 3), they also had the lowest coverage of 31% and 36%, respectively.
| HIV Prevention Services Implementation | Treatment Implementation | |||||||||||||||||
| PMTCT | Condom promotion | HIV testing & counselling | Harm reduction IDU | Risk reduction men who have sex with men | Risk reduction sex workers | Antiretroviral therapy | Paediatric AIDS treatment | HIV testing & counselling TB patients | ||||||||||
| A† | B‡ | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | |
| Côte d’Ivoire | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Cameroon | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | - | - | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Burkina Faso | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | - | ΓΆΒ?Β | - | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Nigeria | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? |
| Uganda | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | - | - | - | - | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? |
| Ghana | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | ΓΆΒ?Β? | - | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β | ΓΆΒ?Β | ΓΆΒ?Β? | ΓΆΒ?Β? |
Abbreviations: PMTCT, Prevention of mother-to-child transmission; IDU, Intravenous drug users; TB, Tuberculosis.
* Data were derived from the UNAIDS 2010 global report. The NCPI comprises a series of questions on the progress in development and implementation of national HIV
policies, strategies and laws. It is divided into two parts: one completed by government officials (A) and one by civil society organizations and nongovernmental sources
(B). Questions are answered by yes ( ΓΆΒ?Β? ), no ( ΓΆΒ?Β ), or not applicable ( - ) [4].
† A: The response by government officials on a subset of the questions on key policies, and on strategies of programmes on prevention, treatment, care and support of HIV.
‡ B: The response by civil society organizations, bilateral and multilateral organizations on key policies, and on strategies of programmes on prevention, treatment, care
and support of HIV.
Table 3: National Composite Policy Index (NCPI) results,* in low prevalence countries.
Ratio of school attendance of orphans to school attendance of non-orphans aged 10-14 years
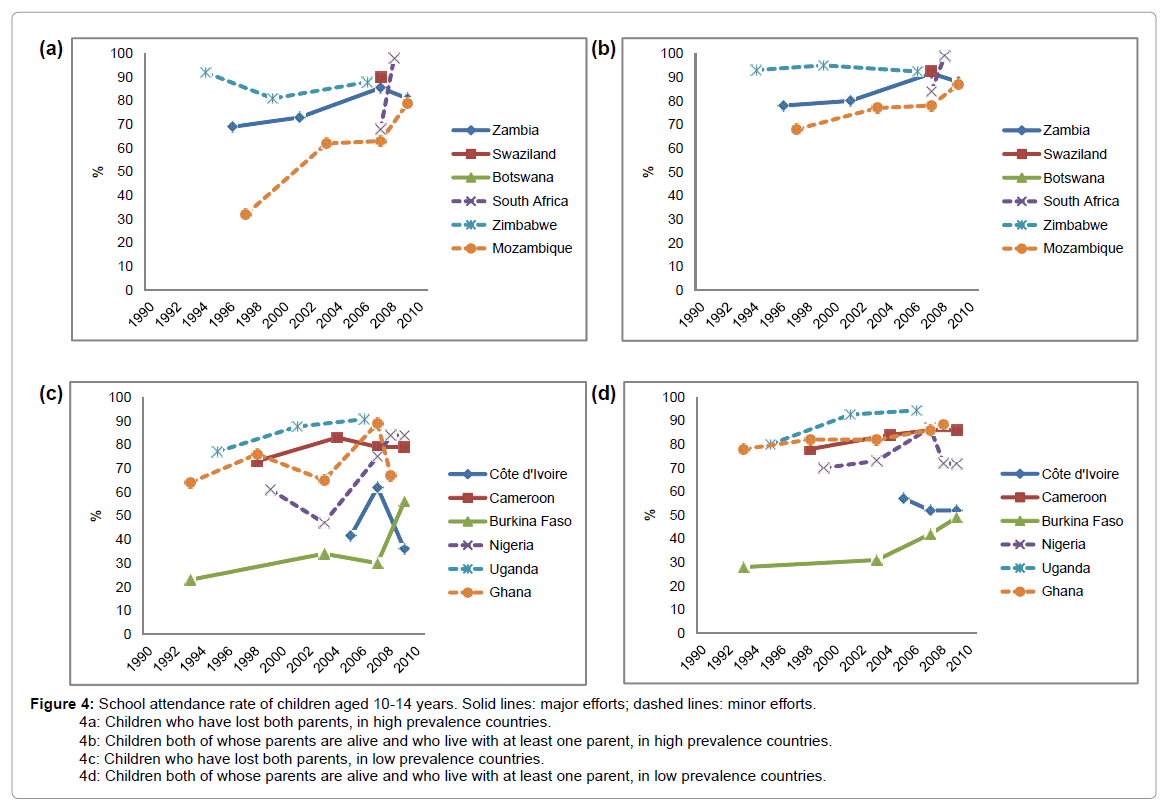
As recommended by the MDG indicator handbook, this indicator was measured as the current school attendance rate of children (aged 10-14) in a household survey who have lost both parents, divided by the current school attendance rate of children (aged 10-14 years) whose parents are both still alive and who live with at least one parent. This information alone is not thoroughly informative and potentially misleading since the ratio is high whenever the school attendance of orphans is similar to the school attendance of non-orphans (both at high or low levels). Therefore, we presented these rates separately. Differences between the sexes were small and as most information was available on both sexes combined, we only assessed the total group (Figure 4a-4d) [14].
4a: Children who have lost both parents, in high prevalence countries.
4b: Children both of whose parents are alive and who live with at least one parent, in high prevalence countries.
4c: Children who have lost both parents, in low prevalence countries.
4d: Children both of whose parents are alive and who live with at least one parent, in low prevalence countries.
In the high prevalence countries that made major efforts, only for Zambia sufficient data was available to assess progress. School attendance was high in both the orphans and non-orphans, though somewhat higher in the non-orphans, and the rate did not increase over the years (Figure 4a-4b). The high prevalence countries that made minor efforts also showed a higher school attendance in the non-orphans. The school attendance rate remained stable or increased in these countries; the limited data in South Africa even showed a tremendous increase of 30% between 2007 and 2008. Overall, there is no difference observed in school attendance between countries that made major and minor efforts.
For the countries with a low prevalence much more data was available (Figure 4c-4d). Burkina Faso and Côte d’Ivoire, both countries that made major efforts, had lower school attendance rates than the other four countries. These results were not consistent with the division of the groups, as the school attendance was higher in the countries that had a less extensive HIV/AIDS policy. Striking were the higher school attendance rates in high prevalence countries.
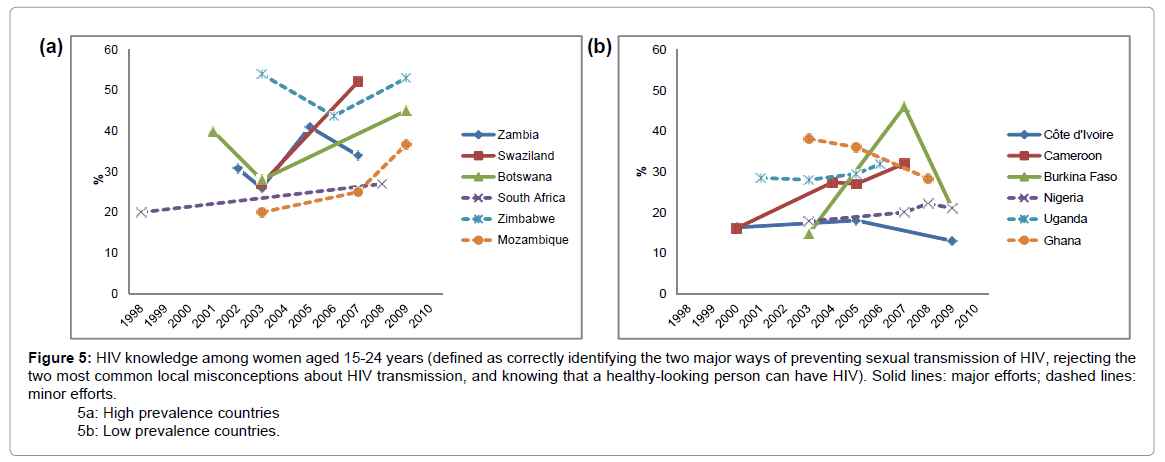
Comprehensive correct knowledge of HIV/AIDS among population aged 15-24 years
This indicator was measured as the number of respondents (women and men aged 15-24 years) who correctly answered all five questions on preventing sexual transmission of HIV and misconceptions about HIV transmission, of the total number of respondents aged 15-24 [14]. This description was in accordance with the recommended measurement method [9]. Only the data for women are presented, as they were comparable to the data for men but more complete (Figure 5a-5b). The following results on women therefore also apply to men to the same extent.
5a: High prevalence countries
5b: Low prevalence countries.
Since the year 2000, in the high prevalence countries the level of knowledge on HIV among the young population had either remained at the same level or improved. Nevertheless, in none of the countries more than 60% of the respondents correctly answered all five questions. No systematic differences between countries that made major and minor efforts were found.
For the low prevalence countries minor progress or even a decrease of knowledge was observed, which was independent of the amount of effort made. Furthermore, when the data of the countries with high and low prevalence were compared, the knowledge in the countries with a high prevalence was greater.
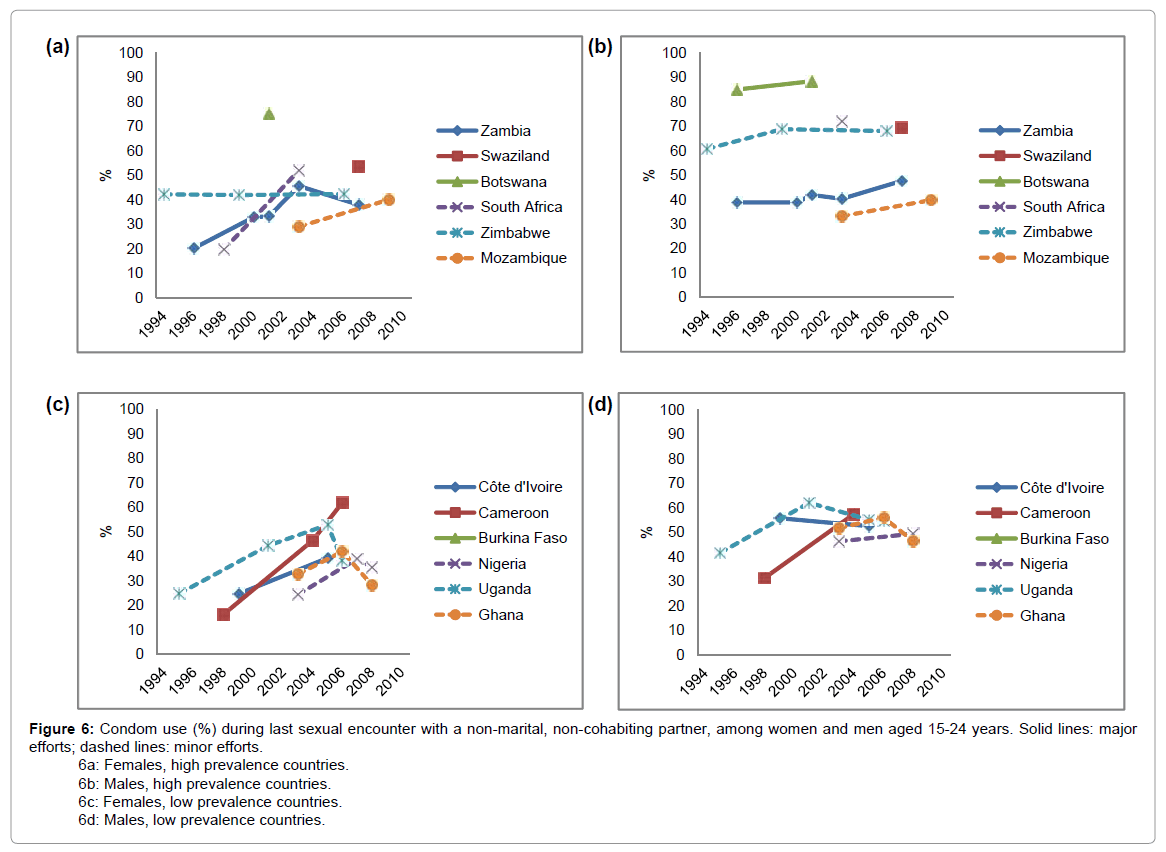
Condom use at last high-risk sexual encounter among population aged 15-24 years
This indicator was described as the number of respondents (persons aged 15-24 years) who said they used a condom the last time they had sex with a non-marital, non-cohabiting partner, as a percentage of all the respondents aged 15-24 who had sex with such a partner in the last 12 months, as measured by Population-based surveys [14].This is in accordance with the recommended measurement method [9]. Overall, available data was limited, making a comparison between countries that made major and minor efforts more problematic. It appeared that for all countries the condom use reported in men was higher than in women (Figure 6a-6d).
In the high prevalence countries, condom use in women was below or around 50%, only Botswana did better with 75% (Figure 6a-6b). With percentages above 80% condom use in Botswana was high in men as well. In Swaziland, South Africa and Zimbabwe men scored around 70%. In Zimbabwe this percentage differed greatly from condom use in women, which was only 42%. In the other countries this difference was less prominent. Condom services were implemented in all six countries according to the NCPI (Table 2). Nevertheless, increase over the years was small. The largest progress was observed in women in Zambia and South Africa, respectively 13% and 32%.
6a: Females, high prevalence countries.
6b: Males, high prevalence countries.
6c: Females, low prevalence countries.
6d: Males, low prevalence countries.
In the countries with a low prevalence relatively stable results over the years were found in men (Figure 6c-6d). Only Cameroon showed a large increase for both men and women, 26% and 46%, respectively. For women, the countries that made major efforts showed improvement in condom use compared to the countries that made minor efforts which showed a downward curve in the most recent years. However, the differences in condom use between the low prevalence countries were small, after the year 2000 condom use was between 30% and 60% in both sexes.
Discussion
In this study we assessed accomplishments in selected SSA countries related to the two targets of MDG6: the reduction of the spread of HIV/ AIDS and the increase of access to ART. For five specific indicators trends in time were assessed as well as the differences between countries that made minor and major efforts to combat HIV/AIDS, in both high and low prevalence SSA countries.
Overall, we noticed signs of improvement over time. For instance, the presumed educational gap between orphans and non-orphans has largely disappeared and school attendance is reasonably high in most countries. For the high prevalence countries the school attendance rate in orphans will be above 80% and probably even above 90% in nonorphans by 2010. School attendance rates above 80% should be feasible for most of the low prevalence countries as well, excluding Côte d’Ivoire and Burkina Faso. Surprisingly, countries that put more effort in this indicator did not do better than countries with less specific actions. Note only educational actions targeting on MDG6 were included and not the ones related to MDG2, which specifically aims at achieving universal primary education, this could explain the remarkable results [3].
Some of the high prevalence countries in Southern SSA have denied the severity of the HIV/AIDS epidemic in the past, but all high prevalence countries in this study have now been taking massive action. Partly as a result of the MDGs and the ‘3 by 5 initiative’, which focuses on the rapid increase of ART coverage [15], remarkable results in the access to ART have been accomplished in these countries. High prevalence countries that made major efforts had already achieved the objective of universal access (for at least 80% of the people in need) by 2009, whereas the countries that made minor efforts are very unlikely to reach the objective by 2010. In the low prevalence countries large improvements are made as well, although the objective will not be reached by most of these countries. In contrast to the results of the high prevalence countries, in low prevalence countries with major efforts ART coverage was comparable to the countries with minor efforts.
However, not all results were that promising. For instance, the objective for the indicator prevalence of HIV in pregnant women (a 25% reduction by 2010, compared to 1990) will not be reached by any of the high prevalence countries. Zambia and Zimbabwe were the only countries where the most recent prevalence rates were comparable to the rates in 1990, but for most other countries the prevalence increased substantially in the past twenty years. Nevertheless, in recent years several countries, in both the group with major and minor effort, developed stable rates.
Condom use in high-risk sexual encounters hardly increased over time in most countries, and countries with more specific actions did not show better results on this indicator. Condom use among women was in general lower than among men. Gender inequalities and gender based violence among women are still major problems in SSA countries [16]. Promoting condom use therefore provides little help for women vulnerable to sexually transmitted infections as condom use is mainly determined by the male partner [17]. Although in some high prevalence countries, especially Botswana, condom use was already high before 2000, only in Cameroon the efforts due to MDG6 have resulted in a scale up of condom use in both sexes. In other countries, not much improvement is to be expected before 2015, because the necessary behavioural change can only be accomplished by massive education and intensive campaigns. The same holds true for general knowledge on HIV and HIV prevention which was and still is substandard in most countries, irrespective of specific efforts made. Again, education is the key factor for improvement. The objective of this indicator for 2005 (correct answers on five simple questions by 90% of the respondents) was not reached by far by any of the countries. The objective for 2010 (correct answers on these questions by 95% of the respondents), is also highly unlikely to be reached.
Results of the recently published UN report on the MDGs [18] correspond well with our findings, which is not surprising since they were based on the same data. For instance, similar to our study, a 13- fold increase was reported of the number of people receiving ART for HIV/AIDS between 2004 and 2009. Apart from the reassurance that our results correspond to this and other UN reports, our study provided time trends for four distinguishable types of specific countries in SSA: countries with contrasting HIV prevalence rates and/or contrasting intensity of HIV related actions. With this approach we attempted to compare the effect of targeted policy interventions resulting from MDG6 in selected SSA countries between countries with a different epidemic course.
Of note is the fact that ‘effort made to achieve MDG6’ is measured by an indicator (the National Composite Policy Index - NCPI), that is estimated from a self-completion questionnaire focusing on political support and national strategies and policies. NCPI is designed specifically to assess progress in the development and implementation of legislation and policies related to national strategic plans, HIV prevention efforts, maintenance of human rights and provision of care and support. There may be problems in estimating the efforts in this way, including the following: (i) NCPI data collected through a selfcompletion questionnaire may have inherent subjectivity; (ii) NCPI data reflect effort made in health sector and may not include many determinants of progress that are outside the control of the health sector: this is especially important for indicators reflecting behavioural change and/or intersectoral collaboration; (iii) data availability and quality may be inadequate; (iv) The NCPI results used to classify countries into two groups based on the amount of effort put into accomplishing the targets, were a rough version of the total contents of this indicator [4]. These methodological limitations might have led to misclassification, resulting in indistinguishable differences between the two groups.
Because the UN represents almost all countries in the world and governments as well as (inter)national organizations are involved in data collection, the data for our study was fairly well standardized and of sufficient size. Nevertheless, the number of data points available was somewhat disappointing, as not all countries have reported on the MDG indicators as frequently as requested by the UN. The UN insists on continuous and comprehensive data collection in order to monitor trends, demonstrate progress and to keep countries and organizations motivated. Fortunately, with every measurement round more countries provide useful information, and the production of quality data is expanding. However, the countries under investigation had better reporting on the MDG indicators which might imply that they are not representative of all SSA countries.
The MDG handbook recommends the use of information on pregnant women attending antenatal clinics between the ages 15-24 as indicator for HIV prevalence. The reason for this age limit is that the prevalence in younger ages is a better reflection of recent trends in incidence and risk behaviour, due to the long duration of an HIV infection. Although there was no age specification for the data we used for this indicator, probably resulting in the inclusion of women above the age of 24, these women will in general be younger than the average population. Recently the importance of stratification by age has been shown by Rehle et al. [19] who measured HIV incidence in South Africa and compared it to the prevalence. In all age groups the prevalence largely exceeded the incidence, in the youngest age group (<20 years) this difference was the smallest. However, we question whether HIV prevalence, measured in pregnant women, should remain a core indicator. Firstly, the incidence among women is generally higher than among men [20]. Secondly, as the prevalence is a result of the incidence and of the mortality in a population, it is only a proxy for the actual incidence in the population. The large increase of ART coverage has resulted in a decrease in mortality [16], this leads to an increase of the prevalence (also in younger ages, although in a lesser extend) when the incidence remains constant. As the prevalence in many countries has stabilized and in some countries signs of decrease started to show, even with the existing decrease in mortality, we infer that the incidence also has decreased. In order to have a better view on these trends, we suggest assessing indicators on incidence and mortality for both men and women separately. Furthermore, we recommend in future research to focus on the background and political situation in individual countries, in combination with the specific efforts made, to further investigate the reasons why some countries are better on track towards reaching MDG6 than others.
Despite efforts to increase knowledge on HIV and HIV prevention, and to promote safe sex, the improvements due to MDG6 actions were small in the countries under investigation. The indicator that achieved the largest progress was ART coverage. All countries showed large improvements, especially the countries that put major effort in increasing ART access. In recent literature the need for a combination approach of biomedical and behavioural interventions targeted on specific populations has been emphasized [21,22]. Also extending voluntary ART testing followed by immediate ART to prevent HIV transmission has been advocated [23]. The effect of ART is twofold: it is an effective treatment, resulting in fewer AIDS related deaths, and it reduces the risk of transmission of the virus as well. A further increase of the availability of ART in the total population in the total population in SSA countries with high prevalence seems therefore a promising strategy for the near future. Nevertheless, efforts in increasing knowledge on HIV and promoting the use of condoms by education can reduce the incidence of HIV by changing the behaviour of a population, which remains the best strategy in the long-term.
References
- United Nations (2000) United Nations Millennium Declaration: resolution adopted by the General Assembly. United Nations, New York.
- Kabeer N (2010) Can the MDGs provide a pathway to social justice? The challenge of intersecting inequalities. United Nations, New York.
- United Nations (2011) Millennium Development Goals.
- UNAIDS (2010) United Nations General Assembly Special Session on HIV/AIDS: Monitoring the Declaration of Commitment on HIV/AIDS, guidelines on construction of core indicators. UNAIDS, Geneva.
- UNAIDS (2011). Website accessed March.
- UNAIDS (2010) UNAIDS report on the global AIDS epidemic 2010. UNAIDS, Geneva.
- World Health Organization. Towards Universal Access: Scaling up priority HIV/AIDS interventions in the health sector: Progress Report 2010. WHO press, Geneva.
- World Health Organization (2011) Global Health Observatory Data Repository.
- United Nations (2003) Indicators for monitoring the Millennium Development Goals, Definitions, Rationale, Concepts and Sources. United Nations, New York.
- UNAIDS/WHO (2008) Epidemiological fact sheet on HIV AIDS, core data on epidemiology and response. UNAIDS/WHO, Geneva. http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_BW.pdf
- UNAIDS (2002) United Nations General Assembly Special Session on HIV/AIDS: Monitoring the Declaration of Commitment on HIV/AIDS, guidelines on construction of core indicators. UNAIDS, Geneva.
- UNAIDS (2005) United Nations General Assembly Special Session on HIV/AIDS: Monitoring the Declaration of Commitment on HIV/AIDS, guidelines on construction of core indicators. UNAIDS, Geneva.
- (2011) Measure DHS Online Tool: HIV/AIDS Survey Indicators Database.
- UNAIDS (2008) United Nations General Assembly Special Session on HIV/AIDS: Monitoring the Declaration of Commitment on HIV/AIDS, guidelines on construction of core indicators. UNAIDS, Geneva.
- UNAIDS (2008) UNAIDS report on the global AIDS epidemic 2008. UNAIDS, Geneva.
- World Health Organization (2011) The 3 by 5 initiative.
- Lang DL, Salazar LF, Wingood GM, DiClemente RJ, Mikhail I (2007) Associations between recent gender-based violence and pregnancy, sexually transmitted infections, condom use practices, and negotiation of sexual practices among HIV-positive women. J Acquir Immune Defic Syndr 46: 216-221.
- Jewkes RK, Dunkle K, Nduna M, Shai N (2010) Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet 376: 41-48.
- Rehle T, Shisana O, Pillay V, Zuma K, Puren A, et al. (2007) National HIV incidence measures--new insights into the South African epidemic. S Afr Med J 97: 194-199.
- United Nations (2011) The Millennium Development Goals Report 2011. United Nations, New York.
- Rotheram-Borus MJ, Swendeman D, Chovnick G (2009) The past, present, and future of HIV prevention: integrating behavioral, biomedical, and structural intervention strategies for the next generation of HIV prevention. Annu Rev Clin Psychol 5:143-167.
- Padian NS, Buvé A, Balkus J, Serwadda D, Cates W Jr (2008) Biomedical interventions to prevent HIV infection: evidence, challenges, and way forward. Lancet 372: 585-599.
- Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG (2009) Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet 373: 48-57.
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_BF.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_CM.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_CI.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_GH.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_MZ.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_NG.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_SZ.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_UG.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_ZM.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_ZW.pdf
http://apps.who.int/globalatlas/predefinedReports/EFS2008/full/EFS2008_ZA.pdf
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14793
- [From(publication date):
February-2012 - Dec 23, 2025] - Breakdown by view type
- HTML page views : 10141
- PDF downloads : 4652