A Knowledge Translation Perspective on the Two Quantitative Sensory Tests and their Usability with Clinicians
Received: 15-Jan-2015 / Accepted Date: 16-Mar-2015 / Published Date: 30-Mar-2015 DOI: 10.4172/2165-7025.1000257
Abstract
Background: Knowledge Translation (KT) in health service can be conceptualized as evidence based knowledge transfer to clinical practice. KT puts evidence-informed innovations into practice and evaluates the effectiveness innovations. The use of Quantitative Sensory Testing (QST) is rare in clinics despite its scientific evidence and potential benefit for patient care. Appropriate KT plan can reduce the gap between scientific evidence and clinical practice. This KT project aimed to develop and conduct beta testing of two KT tools (created knowledge) with the target population (clinicians) who treat musculoskeletal pain disorders.
Methods: This paper explores how evidence-informed innovations (knowledge creation) may work in action process model of KT. The whole process may be defined as “knowledge-to-action” process, and it is a dynamic interaction between researchers, clinicians and stakeholders. We used Ovid database (e.g. MEDLINE, EMBASE, AMED, PsycINFO) for literature review and KT tool production ((knowledge creation). This KT project evaluated two KT tools (manual and video) by administering the survey with 12 clinicians.
Results: Overall rating of the KT tools (manual and video) = 5.75 out of 6. All responses from 12 clinicians were affirmative answer and minimum 75% inquires strongly agreed on all components/topics. Clinicians supported implementation of the two QST techniques for the clinical setting and their feedback assisted in the strategy for implementation.
Conclusions: Evaluation of KT through the wide lens of the “knowledge-to-action” process creates awareness of the value of clinicians and research based evidence. It justifies opportunities and pathways of KT for QST in clinic. The study with a KT model reflected clinical perspective of knowledge has a potential role in successful KT intervention. The future directed models may allow clinicians and stakeholders to analyse complex situation in health service, and it may help to identify target KT strategies to solve the practical problem for implementing two reliable, feasible and economic QST in clinical practice.
Keywords: Pain evaluation; Sensory assessment; Evidence transfer;Clinical application
360603Introduction
There is knowledge to practice gap in pain management and measurement. To corroborate, the model of mechanism-based pain suggests that pain develops through a chronological process that includes 4 stages: (a) disease/injury, (b) mechanism, (c) symptom, and (d) syndrome [1,2]. Rationally, pain management should focus on the pain “mechanism” rather the “symptom” suppression to modify disease [2,3]. Current clinical pain measuring tools are mainly focused on the “symptom” level [1,3-5]. Nonetheless, a better measure is hidden at the “mechanism” level of the chronological factors of pain. Quantitative Sensory Testing (QST) can differentiate responses of pain “mechanism” by sensitivity measure [6,7]. QST is a feasible clinical method to detect neural sensitivity by comparing basal pain sensitivity to hyper-norm-hypo sensitivity [6]. Detail description about QST is in the page 3 and 4 of this free accessed manual. The big challenge is to modify current clinical practice with a better approach on mechanism based concept and QST tools.
Clinical pain management should be based on a relational classification system of pain [1,3-5]. Pain can be classified based on disease, duration, anatomy, and mechanism or other factors [8]. At a broad level, there are two types of pain: Adaptive or Physiological pain (e.g. nociceptive, acute inflammatory) and Maladaptive or Pathological pain (e.g. neuropathic, dysfunctional) [2,4,5]. It is clinically important to differentiate patients based on these fundamental categories of pain with a feasible assessment tool. QST is such a tool, which is capable of differentiate Adaptive and Maladaptive pain (two fundamental types of pain). QST is a kind of psychophysical testing (application of a sensory stimulus, and evaluating the person’s interpretation of that stimulus) approach that can evaluate the functionality from sensory receptors to the brain and thereby detect alteration and reorganization in the nociceptive (neural pain processing) pathways. The semi-subjective QST (combination of subjective and objective assessment) measures the intensity of stimulus for specific sensory perception rather than examiner’s bias from physical examinations. It is possible to evaluate the sensory processing of both large and small fibers by the different sensory inputs of QST [6,7,9-11]. Since QST can detect subtypes of pain, it may assist clinicians to direct patients to the optimal treatments.
Maladaptive pain is a global health problem with significant economic impact [12]. Involvement of the central nervous system in “Maladaptive” pain mechanism is an emerging area of potential development in rehabilitation practice. Moreover, pain is now considered as the 5th vital sign [13-16]; hence central integrating pain measurement is an essential part of the clinical assessment. Central mechanisms have been implicated in the transition from adaptive to maladaptive pain suggesting that early detection of this involvement might allow clinicians to make more accurate prognosis and management strategies for their patients. As QST methods are developed, it is important to establish which measures are useful in clinical practice and feasible in a clinical setting. Despite potentiality, the use of QST is rare in clinics. However, appropriate Knowledge Translation (KT) plan can reduce the gap between scientific evidence and clinical practice. The success of KT plan also depends on the problem identification.
The Canadian Institutes of Health Research defined knowledge translation (KT) “as a dynamic and iterative process that includes synthesis, dissemination, exchange and ethically-sound application of knowledge to improve health, provide more effective health services and products and strengthen the health care system” [17]. In short, translating or mobilizing evidence based knowledge to clinical practice can be conceptualized as KT. Appropriate knowledge mobilization puts evidence-informed innovations into practice and evaluates the effectiveness innovations [18,19]. It is essential to identify the gap/ problem between knowledge and practice before a KT process.
Pain outcome measures in clinic and problem
QST is a new technique within the context of clinical practice, in spite of its evidence over the last two decades [6,7]. QST is used widely as a pain assessment technique in laboratories [6], whereas seldom in clinical practice. Clinicians are not so familiar with the technique, and most of the QST tests are generally thought as expensive (as seen in laboratory). An evidence based open access manualintroduce two QST procedures that might be helpful for clinical pain assessment, as well as better identification of prognostic factors for optimizing treatment plans. The combined instruction (manual and video) for the two QSTs (Ten test [20-23] and the Cold Stress test [22,24-26]) was made to illustrate that these two tests are feasible for any clinic with limited equipment resources. A comparative overview and rationale for the choice of the Cold Stress Test and the Ten Test are in the page 4 of this free accessed manual. The combination of these two simple tests provides a more comprehensive assessment of pain fibers (large diameter slow adapting A-β fiber and small diameter fast adapting A-δ and C fibers). This guide should assist with implementation. The reliability and validity of the two tests have been reported and recommended [20,21-24,26-32]. Many clinicians are busy and have a little time to read scientific papers. It is not always easy to adapt evidence based techniques [33]. Changing clinical practice can be complex and requires addressing multiple barriers. Multi-modal KT interventions may enhance the use of QST among clinicians [34,35].
Aim and objective of this knowledge translation (KT)
Sensory testing has a level of skill involvement and requires specific rules around application and interpretation. It was determined that KT tools that included information through the use of an instruction manual or booklet and video might assist with implementation. This KT project aimed to develop and conduct beta testing of these KT tools with the target population (clinicians) who treat musculoskeletal pain disorders.
The objective of this KT project is to support implementation of two simple QST techniques. The target audience is clinicians who might be able to implement QST and need applied information on the technique and its interpretation.
Knowledge translation framework of this study
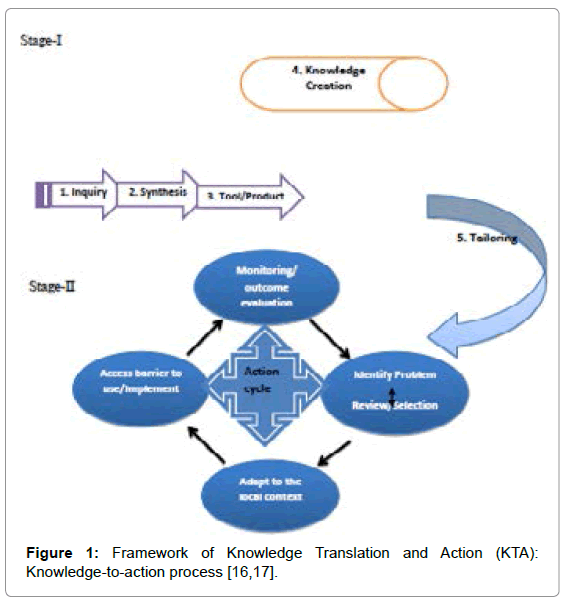
KT occurs within a complex social structure and requires collaborative interactions amongst stakeholders (e.g. patients, policymakers, health care professionals). It occurs over time, but is facilitated by an appropriate action plan for implementation [36]. Hence, it is better to conceptualize KT in a broader framework of Knowledge Translation and Action (KTA). The concept of KTA process divided into two stages: knowledge creation (stage-1) and action (stage-2) [36,37] (Figure 1). We followed the steps of knowledge creation (Figure 1), to create knowledge about the evidence-based information of the two QST techniques. After creating knowledge, we tailored it for the target stakeholders (clinicians) by making an instruction manual and a video. For our action plan, we introduced our tailored knowledge to clinicians for problem identification, and it was reviewed by a survey. We sought feedback and are now considering the KT project sustainability and its future direction within action cycle (stage-2 in Figure 1).
Methods
Literature review, tool production and KT consideration
We used Ovid (e.g. MEDLINE, EMBASE, AMED, PsycINFO) through McMaster University web library databases. Ovid is the largest and a comprehensive biomedical database. All published literature focused on The Cold Stress Test and The Ten Test were reviewed to make an informative manual. The consolidated information from literature helped us to make a 3-minutes you tube video about the tests’ procedure. Web links are provided (in the 2nd section of this paper) for the developed video and manual. Moreover, selected literature on KT (model and intervention process), QST (psychophysical measurement properties, theoretical and empirical rigour of this type of test and its clinical relevance) and pain mechanism (theory based model, classification and sensory evaluation) were reviewed to understand about KT intervention with clinicians who deal with musculoskeletal pain disorders.
Administering the survey with clinicians
We developed a web-based survey using “survey monkey” as an administration tool. The participants were asked eight questions (4 demographics and 4 about the manual and video). A suggestion box for quality improvement was included at the end of the survey. The specific feedback addressed: the need of QST, intention to use, feedback about the test description, and evaluation of whether the tools achieved the right balance between brevity and comprehensiveness.
The manual was attached with email and the volunteers were provided the tests’ procedure video link and the survey. Initially, 14 clinicians were approached, and 12 clinicians responded within a month. Details about the participants are in Table 1.
Results
The respondents were clinicians who worked in musculoskeletal pain settings and educated in either United States or Canada or Australia (Table 1). Participant’s responses to the module and video are described in Table 2. Overall rating of the KT tools (manual and video) = 5.75 out of 6. All responses from 12 clinicians were affirmative answer and minimum 75% inquires strongly agreed on all components/topics. Clinicians supported implementation of the two quantitative sensory testing techniques for the clinical setting.
| Variables | Characteristics (n = 12) |
|---|---|
| Profession | Physiotherapist = 91.7%(11), Occupational Therapist = 8.3%(1) |
| Licensing/practising country (within last 2 years) | USA = 41.7%(5), Canada = 25%(3), Australia =16.7%(2), India = 16.7%(2) |
| Clinical Experience ( in years) | years>10 = 58.3%(7), 5-10 years = 25%(3), 2-5 years =16.7% (2) |
| Practice setting | Hospital based clinic = 75% (9), Private clinic = 16.7%(2), Home based = 8.33%(1) |
| Additional degree | Masters=75% (9),Postgraduate diploma =25%(3), Doctoral (DPT) =8.33%(1) |
| Education in Canada, Australia or USA | At least a degree/diploma from Australia or USA = 58.3%(7), PhD student in Canada = 41.7%(5) |
The number after % and inside parentheses indicates the number of participants
Table 1: Background and general information about the 12 participants in the survey study.
| Q. No. | Issue/Topic | Response | Strongly | Moderately | Mildly | Rating Average (out of 6.00)* |
|---|---|---|---|---|---|---|
| 5 | The need of QST is reflected in the booklet | Yes | 75%(9) | 16.7%(2) | 8.3%(1) | 5.67 |
| 6 | Enough information to convince me for the use QST | Agree | 91.7%(11) | 8.3%(1) | 5.92 | |
| 7 | Enough information about how to perform the test | Agree | 75%(9) | 25%(3) | 5.75 | |
| 8 | Right balance between brevity and comprehensiveness | Agree | 75%(9) | 16.7%(2) | 8.3%(1) | 5.67 |
| Overall rating of the manual and video | 5.75 (median = 5.71) |
*In affirmative response (Yes/Agree), Strongly = 6, Moderately = 5, Mildly = 4; In negative response (No/Disagree), Strongly = 1, Moderately = 2, Mildly = 3; All responses were affirmative answer and minimum 75% strongly agreed on all components/topics.
Table 2: Specific information from participants about the two QST instruction booklet/manual and video.
Clinicians also suggested for quality improvement of the manual. The suggestions summery are as follow: 1. To improve readability and need some format changes (e.g. to add table of contents, list, and bullet points), 2. The need for simple language (e.g. avoids scientific terms, translate into the local language). Clinicians’ feedback assisted in the strategy for implementation and future plan.
What was learned from this KT intervention
This KT module provided us the opportunity to experience firsthand the challenges in developing a tool for clinicians that might be useful for helping them to incorporate quantitative sensory testing into their practice. Since the tools are both a manual and an accompanying video, it was required to write text with a target audience of a clinician in mind, take pictures, and produce a video for upload, which are all practical skills that are useful in creating knowledge translation tools. The process of interviewing clinicians who use the tools and understanding where we missed judge usability and hearing concerns about implementation provided an opportunity to more fully understand knowledge translation on the frontline of conducting it. The survey result reflected the strength and weakness of the KT tools. The initial version of the user manual was revised after getting suggestions from clinicians. The changes included format changes, the addition of a table of contents, and term simplifications. The critical evaluation by clinicians resulted in two tools (manual and video) that were developed through integration of evidence, theory and feedback that can assist in the implementation of the two QST techniques for the clinical setting.
Future direction of knowledge translation and action (KTA)
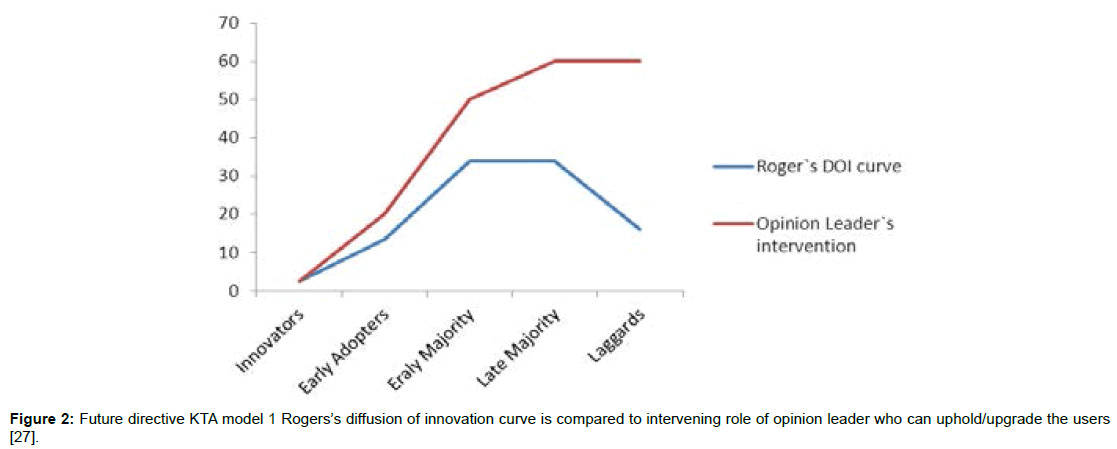
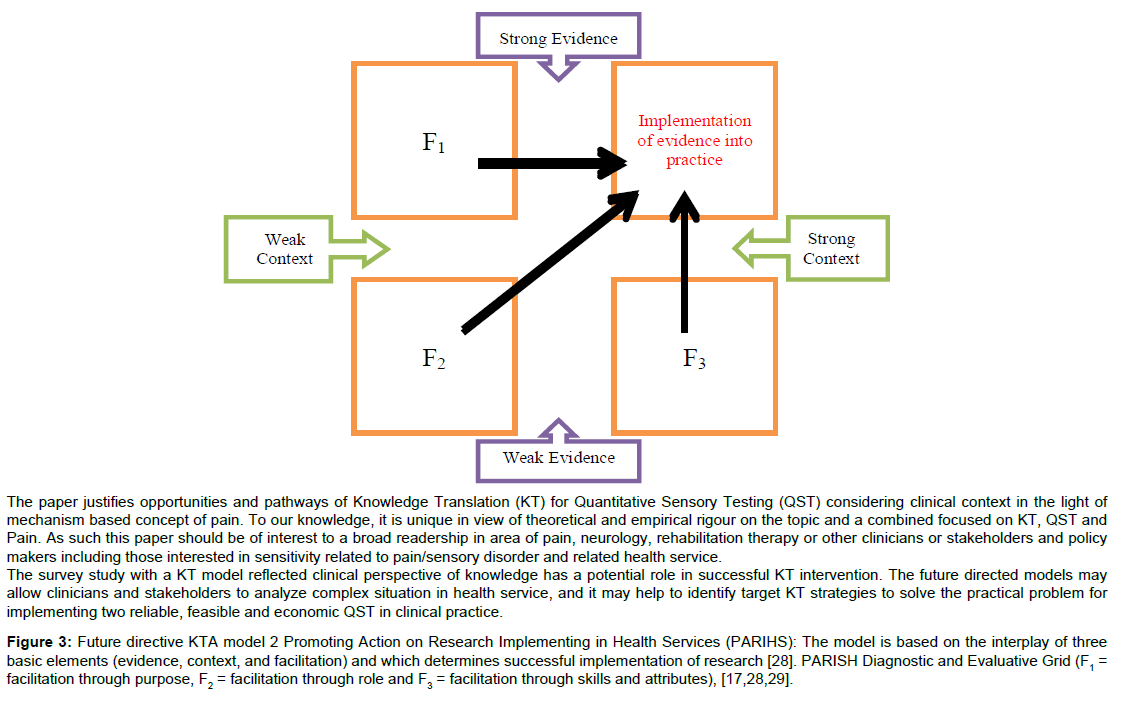
We would like to consider two models of KTA process for better success of our future plan in the local context. The proposed two models are: Diffusion of Innovations (DOI) model and Promoting Action on Research Implementing in Health Services (PARIHS) model. Schematic diagrams of these models are in Figures 2 and 3. The DOI theory explains why, how and at what absorption rates a new technology spread throughout the culture [38]. As a new technique in clinical practice, the proposed technique will be gradually accepted among clinicians according to the DOI theory. The technology transfer for target users through this model would suggest the need for an opinion leader who can motivate the users (Figure 2, demonstrated the uplift of users by an opinion leader). Conversely, the PARIHS model focuses on the context or environment in which change must happens and could be helpful to implement sensory testing in environments such as a hospital. This framework emphasizes the importance of empowering facilitation considering both the context and evidence. Facilitators are considered in the PARIHS diagnostic and evaluative grid (Figure 3). Some key elements of success suggested by this framework are: monitoring of changes and evaluation strategies, support for implementation, training for a team over change, and progress mapping. Ultimately, combination of both models (DOI and PARIHS) in the KTA process might enhance the effectiveness of KT that is designed to move quantitative sensory testing into clinical practice.
Figure 3: Future directive KTA model 2 Promoting Action on Research Implementing in Health Services (PARIHS): The model is based on the interplay of three basic elements (evidence, context, and facilitation) and which determines successful implementation of research [28]. PARISH Diagnostic and Evaluative Grid (F1 = facilitation through purpose, F2 = facilitation through role and F2 = facilitation through skills and attributes), [17,28,29].
Conclusion
Our primary KT intervention result reflected that clinicians supported implementation of the two quantitative sensory testing techniques for the clinical setting. This two simple QST tests can provide a detailed sensory profile that will compliment other clinical assessment tools. Since these two tests are feasible in the clinic and an economical choice for the clinician in comparison to the instrument based QST and both tests have good diagnostic and prognostic value in different disease conditions for evaluation of sensory function. Therefore, appropriate future directed KT intervention with clinicians and stakeholders may assist this two QST technique into clinical practice.
References
- Woolf CJ, Max MB (2001) Mechanism-based pain diagnosis: Issues for analgesic drug development. Anesthesiology 95: 241-249.
- Woolf CJ, Bennett G, Doherty M,Dubner R, Kidd B, et al. (1999) Towards a mechanism-based classification of pain? Pain77:227-229.
- Woolf CJ, Decosterd I (1999) Implications of recent advances in the understanding of pain pathophysiology for the assessment of pain in patients. Pain 82: S141-S147.
- Woolf CJ (2010) What is this thing called pain? J Clin Invest 120: 3742-3744.
- Woolf CJ; American College of Physicians; American Physiological Society (2004) Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann Intern Med 140: 441-451.
- Arendt-Nielsen L, Yarnitsky D (2009) Experimental and clinical applications of quantitative sensory testing applied to skin, muscles and viscera. J Pain 10: 556-572.
- Chong PS, Cros DP (2004) Technology literature review: Quantitative sensory testing. Muscle Nerve 29:734-747.
- Merskey H, Bogduk N (1994) Classification of chronic pain. Seattle: IASP press.
- Uddin Z, MacDermid JC, Galea V (2013) Reliability Indices, Limits of Agreement and Construct Validity of Current Perception Threshold Test in Mechanical Neck Disorder. Crit Rev PhysRehabil Med 25: In Press.
- Uddin Z, MacDermid JC, Galea V (2013) The Current Perception Threshold Test Differentiates Categories of Mechanical Neck Disorder. J Orthop Sports PhysTher: In Press.
- Uddin Z, MacDermid JC, Ham H (2013) Test-Retest Reliability and Validity of Normative Cut-offs of the Two Devices Measuring Touch Threshold: Weinstein Enhanced Sensory Test and Pressure Specified Sensory Device. Hand Therapy: In Press.
- National Center for Health Statistics (US) (2007) Health, United States, 2006 with chartbook on trends in the health of Americans. National Center for Health Statistics.
- Lanser P, Gesell S (2001) Pain management: the fifth vital sign. Healthc Benchmarks 8: 68-70, 62.
- Yuen TS, Irwin MG (2005) The 'fifth vital sign'. Hong Kong Med J 11: 145-146.
- Pain Management- United States of America (2003) Department of Veterans Affairs, Veterans Health Administration. VHA Directive 2003-2021.
- Declaration of Montreal (2010) International Pain Summit by the International Association for the Study of Pain.
- Henry JL (2008)The need for knowledge translation in chronic pain. Pain Res Manage 13:465-476.
- Grimshaw J, Ward J, Eccles M (2001) Getting research into practice. In Oxford handbook of public health practice. Oxford: Oxford University Press.
- Strauch B, Lang A (2003)The ten test revisited. PlastReconstrSurg 112: 593-594.
- Sun HH, Oswald TM, Sachanandani NS, Borschel GH (2010) The 'ten test': Application and limitations in assessing sensory function in the paediatric hand. J PlastReconstrAesthetSurg63: 1849-1852.
- Uddin Z, MacDermid JC, Packham T (2014) Clinical implementation of two Quantitative Sensory Tests: Cold Stress Test and The Ten Test. Physiotherapy Practice and Research 35:In Press.
- Uddin Z, MacDermid JC, PackhamT(2013)The Ten Test for Sensation. J Physiother59:132-132.
- Harada N (2002) Cold-stress tests involving finger skin temperature measurement for evaluation of vascular disorders in hand-arm vibration syndrome: Review of the literature. Int Arch Occup Environ Health75:14-19.
- Traynor R, MacDermid JC (2008) Immersion in cold-water evaluation (ICE) and self-reported cold intolerance are reliable but unrelated measures. Hand 3:212-219.
- Uddin Z, MacDermid JC, Packham T (2013) Ice-water (cold stress) immersion testing. J Physiother59:277.
- Coughlin P, Chetter I, Kent P, Kester R (2001) The analysis of sensitivity, specificity, positive predictive value and negative predictive value of cold provocation thermography in the objective diagnosis of the hand–arm vibration syndrome. Occup Med51:75-80.
- MacDermid JC (2005) Measurement of health outcomes following tendon and nerve repair. JHand Ther 18:297-312.
- Mahbub M, Harada N (2011) Review of different quantification methods for the diagnosis of digital vascular abnormalities in hand-arm vibration syndrome. J OccupHealth53: 241-249.
- Patel MR, Bassini L (1999)A comparison of five tests for determining hand sensibility. J ReconstrMicrosurg15:523-526.
- Strauch B, Lang A, Ferder M, Keyes-Ford M, Freeman K, et al. (1997) The ten test. PlastReconstrSurg 99:1074-1078.
- Traynor R, MacDermid JC (2008) Immersion in cold-water evaluation (ICE) and self-reported cold intolerance are reliable but unrelated measures. Hand3:212-219.
- Jette DU, Bacon K, Batty C, Carlson M, Ferland A, et al. (2003) Evidence-based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. PhysTher83:786-805.
- Menon A, Korner-Bitensky N, Kastner M, McKibbon KA, Straus S, et al. (2009) Strategies for rehabilitation professionals to move evidence-based knowledge into practice: a systematic review. JRehabil Med41:1024-1032.
- Swinkels RA, van Peppen RP, Wittink H, Custers JW, Beurskens AJ, et al. (2011) Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC MusculoskeletDisord12:106.
- Graham ID, Logan J, Harrison MB, Straus SE, Tetroe J, et al. (2006) Lost in knowledge translation: Time for a map? J ContinEduc Health Prof 26:13-24.
- MacDermid JC, Graham ID (2009) Knowledge Translation: Putting the "Practice" in Evidence-Based Practice. Hand Clin25:125-143
- Rogers EM (2003) Diffusion of innovations (5thedn). New York, NY: Free Press.
Citation: Uddin Z, MacDermid JC (2015) A Knowledge Translation Perspective on the Two Quantitative Sensory Tests and their Usability with Clinicians. J Nov Physiother 5:257. DOI: 10.4172/2165-7025.1000257
Copyright: © 2015 Uddin Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14927
- [From(publication date): 4-2015 - Aug 24, 2025]
- Breakdown by view type
- HTML page views: 10200
- PDF downloads: 4727