Acceptance of Tele-Consultation and its Determinant Factors among Doctors in Outpatient Clinics in the Hospital of Conselor Tuanku Muhriz, Kuala Lumpur, Malaysia
Received: 29-Mar-2018 / Accepted Date: 16-Apr-2018 / Published Date: 18-Apr-2018 DOI: 10.4172/2161-0711.1000606
Abstract
The recent introduction of information technology has improved the quality of healthcare services. In many developing countries, including Malaysia, patients suffer from a shortage of trained medical specialists and teleconsultation (TC) would ease access to specialists. The need to know if doctors are willing to accept such technology has prompted this study. The objective of the study therefore was to measure the acceptance, knowledge, and attitude towards tele-consultation among doctors in Conselor Tuanku Muhriz, Kuala Lumpur, Malaysia (HCTM) and to identify the factors which influence its acceptance. Factors such as socio-demographics, knowledge, attitude, perceived ease of use (PEOU) and perceived usefulness (PU) towards tele-consultation were chosen according to the technology acceptance model (TAM) and some literature. This was a cross-sectional study based on a quantitative method. Data was collected from HCTM outpatient clinics in Cheras area, Kuala Lumpur, Malaysia in March 2017. A total of 90 questionnaires were collected from eight different outpatient clinics in HCTM. Statistical Package for the Social Sciences (SPSS) (version 22.0) was used to analyse the data. The results showed an acceptance rate of 63.3% among doctors in HCTM. The study also showed that perception of usefulness and positive attitude had a significant association with the acceptance of TC. In conclusion, this study has revealed the important factors that have influenced tele-consultation acceptance as perceived usefulness and positive attitude. Furthermore, the overall findings from the study suggest that TAM is an appropriate model for explaining physicians' technology acceptance decisions.
Keywords: Telemedicine; Perception; Tele-consultation; Acceptance; Doctors
Introduction
In many developing countries, including Malaysia, patients usually face lack of trained medical specialists especially in the rural areas. Many patients have to wait for a while before they get to see a specialist and general practitioners often have to refer patients with complicated medical cases from their primary health centres to tertiary centres due to lack of available specialists [1].
Technological discoveries are reforming the way in which healthcare services are delivered. Modern technology has changed the constitution and organization of the entire medical field, starting from the universal acceptance of electronic medical records to the progress in biomedical engineering and technology [2].
Malaysia is one the countries that has made many amendments in advance of health information implementation into the health system. The concept of the term “Paperless hospitals” started in 1996-2000 through the seventh Malaysian plan by introducing a fully computerized system for electronic medical records, telemedicine, and tele-conferencing [1]. Improving Health Information Management was also one of the primary intentions to attain the vision of the 9th Malaysian plan to ensure the Integration of Health information Management into all healthcare organizations of the country [3].
Tele-consultation is a form of telemedicine that does not involve a direct 'face to face' or 'in person' consultation for diagnosis or followup of any medical conditions. There are 2 methods of tele-consultation namely: The store-and-forward method (asynchronous) in which, patient medical information is compressed in a digital matter, and sent via the network such as electronic mail (e-mail) to a known specialist or physician. This method is found to be feasible for developing countries since it provides low-cost telemedicine for clinical purposes [4,5]. The second method is to use TC in an interactive way (synchronous), which involves the use of video conferencing between the sender and the receiver for the purpose of medical advice. This method is less implemented in developing countries compared to the synchronous mode due to the inappropriate tele-communication infrastructure in these countries [5].
Telehealth was implemented by the Malaysian government under the Multimedia Super Corridor (MSC) project, Telehealth Flagship in 1996. This project was one of the seven flagship applications of MSC grouped under the ‘Multimedia Development Flagship Application' and has great knowledge with reasonable depth on Telehealth. At first, the support provided was to access the sources of information by healthcare professionals via the internet to medical journals, e-books, and medical databases and to use the e-mail and related technologies to create virtual environment for the healthcare professionals to interact and communicate electronically [6,7]. The Telemedicine Act 1997 endorsed the growth of information communication technology (ICT) in the health sector. The Ministry of Health wanted to manage patient information by linking systems and providers through a solid program of information communication technology and initiated the telemedicine plan which included the Multimedia Super Corridor Flagship initiatives, Program/function-based enterprises including the Nationwide Health Management Information System, the State-wide Tele-primary Care, and Public/Client Access.
The objectives of this study, therefore, were to assess the acceptance, knowledge, and attitude towards tele-consultation among doctors at outpatient clinics in tertiary hospitals and the determinant factors of using tele-consultation. To identify the factors that influence the acceptance of teleconsultation among doctors in HCTM including socio-demographic factors (age, sex, education level, medical specialty, years of experience, and computer literacy), knowledge, attitude, perceived ease of use and perceived usefulness towards teleconsultation. Finally to explore user technology acceptance in healthcare organization planning to provide telemedicine care and services.
The technology acceptance module theory
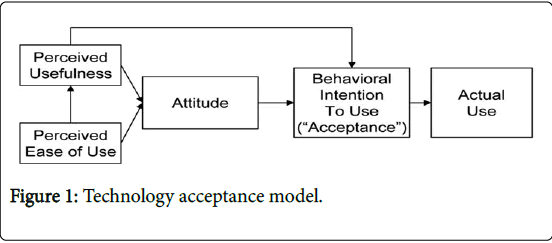
Technology Acceptance Module (TAM) is a global module proposed by Fred. D. Davis in 1989 for evaluating the acceptance of any new technology [8]. This module processes the behavior-related part of attitude in order to differentiate between belief and attitude towards the new technology by setting up a relationship of the two factors (the perceived ease of use and perceived usefulness). Such acceptance is then calculated by users’ perceived ease of use, their perceived usefulness and their attitude towards the new technology. Perceived ease of use (PEOU) is evaluated by assessing how much users believe that the new technology is free of any mental and physical effort. On the other hand, perceived usefulness (PU) is evaluated by assessing how much the user believes that using a particular technology will enhance the diagnosis and treatment of patients thus improving health care practices (Figure 1) [9,10].
Methodology
In this study, a descriptive cross-sectional survey using a definite questionnaire was established to assess associations between the variables by accumulating data from The Hospital of Conselor Tuanku Muhriz (HCTM), Cheras, Malaysia. The duration of this study was from February to June 2017. Doctors in the outpatient clinics in HCTM where chosen.Questionnaires were then administered to medical officers and specialists who practice medicine in the outpatient departments of HCTM. The HCTM center was chosen because it is not only a tertiary centre but also a teaching hospital and a research institution; where intranet solution for teleconferencing is being implemented for educational purposes and where teleconsultation could be easily carried out in the near future. The departments involved were internal medicine, surgery, orthopedic, gynecology and obstetrics, pediatrics, ENT, hematology, and family medicine and the list of physicians was gotten from the Human Resources department with a total 117 names. The choice of doctors from the HCTM was based on the proportion of doctors at the selected departments and the likelihood of their participation in the study.
A 4-paged paper questionnaire comprising six main sections (sociodemographics, knowledge of TC, PEOU, PU, attitude towards TC, acceptance of TC). All sections of the questionnaire except the knowledge section were adapted and modified from two similar studies [7,11,12]. The researcher developed the other set of questionnaires regarding the knowledge section according to the objectives of the study and from related literature reviews. Although validated by prior research, the adopted instrument was examined to ensure content validity and reliability within the targeted context by the judgment of a panel of experts including two experts in health technology, three doctors of public health, and three physicians from altered medical specialties/subspecialties to weigh content validity and to confirm the relevancy of the questions to the objectives of the study. A pre-test was done among 26 doctors inside and outside HCTM who were excluded from the study and Reliability was tested by using the Cronbach's Alpha in SPSS. All sections of the questionnaire gave a result of 0.882 which represents a commonly acceptable level for exploratory research.
Data was analysed using SPSS version 22. Descriptive analysis was carried out by calculating frequencies and percentages. Association was identified between independent and dependent variables using Chi-square tests. After running initial frequencies, bivariate analysis was carried out using chi square and multivariate analysis was carried out using regression analysis for linking association between factors and outcome. Approval for the study was gotten from the Ethical Committee of Universiti Kebangsaan Malaysia (UKM) The Dean’s office and heads of outpatient departments gave permissions as well before proceeding for data collection.
Results
Out of the 110 questionnaires distributed, 90s were completed and returned which represents 83% response rate. Majority of the participants were below 40 of years (91.1%) and a little more than half were males. (51.1% males vs. 48.9% females). The highest number of participants (25.6%) were from Gynaecology and Obstetrics department followed by the Orthopaedic and Internal Medicine departments (22.2% and 20%) respectively then other departments followed. Majority of participants 75.6% had obtained the MBBS degree as their highest level of education, while only 15.6% had obtained a Master Degree and 8.9% had obtained other certificates after their MBBS. None of the participants had a PhD degree. About 71% of the participants had between 5-10 years of experience in the health sector while 19% had more than 10 years of experience and only 10% of the participants had 1-5 years of experience.
After running the Chi square analysis (Table 1) we found association between perception of usefulness and acceptance of TC (P=0.001), Phi and Cramer’s V value of 0.34 shows moderate strength of association. There was an association found in the attitude towards tele-consultation with acceptance of TC (P=0.001), Phi and Cramer’s V value of 0.35 shows moderate strength of association. Other factors such as socio-demographics, knowledge and perceived ease of use did not show association with the acceptance of TC among doctors in HCTM.
| Variable | Acceptance of TC | No Acceptance | χ2 | P-value | ||
|---|---|---|---|---|---|---|
| n | Percentage | n | Percentage | |||
| Age | ||||||
| 30 to 39 | 32 | 39% | 50 | 61% | 3.823 | 0.281 |
| 40 to 49 | 0 | 0% | 5 | 100% | ||
| 50 to 59 | 1 | 50% | 1 | 50% | ||
| 60 and above | 0 | 0% | 1 | 100% | ||
| Sex | ||||||
| Male | 15 | 32.6% | 31 | 67.4% | 0.667 | 0.414 |
| Female | 18 | 40.9% | 26 | 59.1% | ||
| Medical speciality | ||||||
| Hematology | 0 | 0% | 1 | 100% | 5.332 | 0.62 |
| Family medicine | 1 | 33.3% | 2 | 66.7% | ||
| ENT | 0 | 0% | 5 | 100% | ||
| General surgery | 5 | 33.3% | 66.7 | 100% | ||
| Orthopedic | 8 | 40% | 12 | 60% | ||
| Obs and Gyn | 8 | 34.8% | 15 | 65.2% | ||
| Internal medicine | 8 | 44.4% | 10 | 55.6% | ||
| Paediatrics | 3 | 60% | 2 | 40% | ||
| Highest grade obtained | ||||||
| MBBS | 25 | 36.8% | 43 | 63.2% | 3.699 | 0.157 |
| Master | 3 | 21.4% | 11 | 78.6% | ||
| Others | 5 | 62.5% | 3 | 37.5% | ||
| Years of service in health sector | ||||||
| 1-5 Years | 4 | 44.4% | 5 | 55.6% | 0.528 | 0.768 |
| 5-10 Years | 22 | 34.4% | 42 | 65.6% | ||
| More than 10 years | 7 | 41.2% | 10 | 58.8% | ||
| Feel comfortable with technology | ||||||
| Yes | 30 | 34.9% | 56 | 65.1% | 2.649 | 0.104 |
| No | 3 | 755 | 1 | 25% | ||
| Knowledge | ||||||
| Poor knowledge | 16 | 48.5% | 17 | 51.5% | 1.42 | 0.233 |
| Good knowledge | 17 | 29.8% | 40 | 70.2% | ||
| PEOU | ||||||
| No PEOU | 11 | 47.8% | 12 | 52.2% | 1.657 | 0.198 |
| PEOU | 22 | 32.8% | 45 | 67.2% | ||
| PU | ||||||
| No PU | 22 | 55% | 18 | 45% | 10.421 | 0.001 |
| PU | 11 | 22% | 39 | 78% | ||
| Attitude | ||||||
| Negative attitude | 22 | 56.4% | 17 | 43.6% | 11.553 | 0.001 |
| Positive attitude | 11 | 21.6% | 40 | 78.4% | ||
Table 1: Relationship between acceptance of TC with other factors.
As shown in (Table 2) only two independent variables made a unique statistically significant contribution to the model (perceived Usefulness and positive attitude) when simple logistic regression was done while only positive attitude was statistically significant when multiple logistic regression was done. This study showed that doctors who would accept TC were over 4 times more likely to a have positive attitude towards TC than who had negative attitude towards TC. Similarly, doctors who would accept TC were over 4 times more likely to have perception of usefulness of TC compared to doctors who had no perception of usefulness of TC with p<0.05, after controlling of all other factors in the model, yet this factor was no longer a significant predictor for TC when multi logistic regression was done.
| Variables | Simple logistic regression | Multiple logistic regression | ||||
|---|---|---|---|---|---|---|
| B | Crude OR (95% CI) | P-value | B | Adjusted OR (95% CI) | P -value | |
| Sex(Male) | 0.358 | 1.431 (0.605-3.384) | 0.415 | 0.879 | 2.401 (0.605-9.596) | 0.213 |
| Age | -0.446 | 0.640 (0.39-10.60) | 0.755 | 37.425 | 1.792 ( 0.00 -0.00) | 0.999 |
| Medical specialty | -0.264 | 0.768 (0.566- 1.041) | 0.089 | 20.197 | 590754 ( 0.00 -0.00) | 1 |
| Years of service | -0.11 | 0.989(0.440-2.220) | 0.978 | 0.057 | 1.059 (0.175 – 6.395) | 0.95 |
| Comfort with tech | 1.723 | 5.6 (0.558- 56.203) | 0.143 | 0.616 | 1.852 ( 0.143 – 24.06) | 0.638 |
| Knowledge (good) | 0.795 | 2.215 (0.911-5.380) | 0.079 | 0.475 | 1.608 (0.497- 5.200) | 0.428 |
| PEOU | 0.629 | 1.875 (0.715-4.917) | 0.201 | 0.233 | 1.263 (0.347- 4.595) | 0.723 |
| PU | 1.466 | 4.333 (1.737-10.811) | 0.002 | 1.123 | 3.073 (0.839- 11.253) | 0.09 |
| Attitude(Positive) | 1.549 | 4.706 (1.876-11.805) | 0.001 | 1.479 | 4.389(1.162- 16.578) | 0.029 |
Table 2: Final model for factors associated with TC using logistic regression.
Adjusted r2: 0.55
Direct logistic regression method applied.
Multicollinearity and interaction term were checked and not found (Tolerance>0.1)
Hosmer-Lemeshow test (p=0.143) and Omnibus test (p=0.009), thus the fit of this model is achieved.
Percentage accuracy in classification: PAC is 76.7%
The highlighted are the significant variables respectively
Discussion
A total of 57 doctors had good behavioral intention to use TC when it becomes available in HCTM. This percentage is slightly lower than a similar study done in Iran [13] with a 75% acceptance rate and in Italy with an acceptance rate of 85% [14]. Majority of the factors studied in this paper did not have a significant influence on acceptance. Even though this percentage is slightly lower than what is expected, it is considered a proper outcome because of the factors that affected the overall acceptance of doctors. According to Vieru [15] doctors’ higher education and experiences make them more likely to accept new technologies when compared with fresh medical graduates. In this study most doctors had MBBS as their highest degree (75.6%) although they lack experience about TC since TC is not yet implemented in HCTM. Another factor affecting their acceptance is the objection to the concept of seeing patients online even only for simple illnesses (39% disagreement rate regarding seeing patients online, for the purpose of diagnosing or prescribing medication of diseases that do not require much investigation). This phenomenon can be explained by the use of tele-consultation in Malaysia only between doctors for referral or for second opinions.
Unlike the studies by Vankatesh and Au [16,17] men were not more influenced by their perception of usefulness while females were more influenced by ease of usefulness.. In terms of age the majority of participants 91.1% were between 30-39 years of age, yet 39% of this age group did not accept TC (compared to 100% acceptance among the 40-49 age group), nor did it influence their perception of usefulness unlike Au’s study [17] which showed a direct relationship between perceived usefulness and behavioural intention Study results also showed that years of experience has no significant association with the acceptance of TC unlike the literature review supported by Marrop and Win that related experience with the training and education that usually affect the appreciation of TM benefits and capabilities [5].
According to Au and Ayatollahi [13,17] knowledge is considered an essential influence of perception and attitude toward telemedicine. The overall knowledge level (63.3%) is considered appropriate (answering at least 8 questions out of 10) when compared with a similar study in Iran with 91% poor knowledge level among doctors [13]. This would be because they had previous knowledge of the concept of telemedicine and tele-consultation (57.8%) although this was not so in HCTM.
The results of this study were similar to the outcome of Chau and Hu’s study [18] where they stated that physicians have a relatively high general competence and mental/cognitive capacity and may comprehend the use of telemedicine-technology quickly as such become familiar with its operations without going through the intense training that might be necessary among other user populations. Alkmim [19] also indicated that the effect of PEOU varies with different authors, yet 93% of the participants in his study exhibited PEOU compared to only 67% in our findings. Furthermore, physicians in many cases have relatively high staff support for operating medical equipment and related technologies. Together, these factors might have contributed to physicians' placing less weight on perceived ease of use.
The overall PU among physicians was only 55.6% which is considered lower than a parallel study that showed a perception of usefulness of 71% up to 95% [14] and an 86% perception of usefulness in Italy [20]. In our study majority of the respondents who had perception of usefulness of TC actually accepted TC and although many doctors did not perceive the usefulness of TC in following up of chronic diseases like Diabetes Mellitus that did not affect the overall perception of usefulness among doctors. Furthermore, there was a significant influence of PU on acceptance. These results correspond with Chau and Hu statements in their study that perceived usefulness is the most significant factor affecting physicians’ acceptance of telemedicine technology [18]. The effect of perceived usefulness on both attitude and behavioural intention were consistently the highest among all other models examined in their study. Judging by the direct and indirect effect (via attitude) on behaviour intention, perceived usefulness is likely to assert significant influences on a physician’s intention to use telemedicine technology [18]. However, this factor was excluded as a determinant due to the insignificant results gotten for both direct and indirect multiple logistic regression analysis.
Both bivariate and multivariate analysis showed significant influence of positive attitude on acceptance. These results agree with Chau and Hu’s statement about the critical role of attitude in technology acceptance and decision making by individual professionals and therefore singles out the importance of attitude cultivation and management to successful technology implementation [18]. Only 56.7% of doctors showed positive attitude towards TC and this outcome was due to the majority having concerns 78.9% about the loss of effective communications between doctors and patients. In addition, 87.8% of the respondents expressed concerns about patient privacy/confidentiality and 81.1% expressed their concerns about the high cost of the equipment used in TC implementation although these concerns did not affect the overall influence of attitude on the acceptance of TC among doctors. We expect that more physicians would have a positive attitude towards TC after they actually use it thereby eliminating of concerns with practice and increasing their perception of ease of use which would affect their attitude. This expectation was also established in another similar study where physicians’ attitude had changed after execution of TC [20].
Conclusion and Recommendations
This study has highlighted the acceptance of tele-consultation among doctors in HCTM. It used a cross-sectional study method to gather data from doctors in the outpatient departments of HCTM. Acceptance rate among doctors in HCTM was moderate which was lower than similar studies. Majority of the factors studied in this paper did not have a significant influence on acceptance except perception of usefulness and positive attitude. The lower acceptance rate might be due to the lack of “actual” experience of TC or due to having MBBS as the highest degree obtained among participants. Male gender, years of experience, technology literacy and medical speciality did not influence the acceptance of TC unlike similar studies [5]. In addition, good knowledge and perception of ease of use did not have influence on the acceptance of TC unlike similar studies [13,18].
The study had significant impact on technology adoption studies in health care in Malaysia. It has revealed the important factors that have: Influenced tele-consultation acceptance, have established a significant role in the acceptance of the technology in the health care environment. These aspects were found to be Perceived usefulness of TC and positive attitude towards TC. In addition, the overall, findings from the study suggest TAM be an appropriate model for explaining individual physicians' technology acceptance decisions.
It is recommended that doctors get proper training before implementing tele-consultation in HCTM so they gain more perception about the usefulness of TC and more perception of ease of use such technology. Proper training also would widen their horizon about the application of diagnostic and management methods when it comes to distant telecommunication with patients and not only with doctors. It is also recommended that the government along with stakeholders arrange the legal framework for any rules and regulations related to telemedicine and deal with the telemedicine issues, such as confidentiality, reliability, liability and cross-border authority. Providing the equipment required for implementation of telemedicine is a key factor in finding good suppliers and providers of the hardware, and the software of telemedicine required for the implementation. The availability of TC would help users get familiar with technology which would affect their perception and acceptance.
References
- Merican I, bin Yon R (2002) Health care reform and changes: The Malaysian experience. Asia Pac J Public Health 14: 17-22.
- Beach MC, Gary TL, Price EG, Robinson K, Gozu A, et al. (2006) Improving health care quality for racial/ethnic minorities: A systematic review of the best evidence regarding provider and organization interventions. BMC Public Health 6: 104.
- Selvaraju DDS (2006) Health information management: Malaysian experience. Health Informatics Center, Ministry of Health, Malaysia.
- Yusof K, Neoh KH, Bin Hashim MA, Ibrahim I (2002) Role of teleconsultation in moving the healthcare system forward. Asia Pac J Public Health 14: 29-34.
- Maarop N (2013) Understanding the acceptance of teleconsultation technology in Malaysian government hospitals.
- Maarop N, Win KT (2012) Understanding the need of health care providers for teleconsultation and technological attributes in relation to the acceptance of teleconsultation in Malaysia: A mixed methods study. Journal of medical systems 36: 2881-2892.
- Mascha MF, Adya M (2010) Using the technology acceptance model in predicitng acceptance of imposed technology: A field study. Marquette University.
- Abu-Dalbouh HM (2013) A questionnaire approach based on the technology acceptance model for mobile tracking on patient progress applications. J Comp Scien 9: 763-770.
- Kifle M, Mbarika VW, Datta P (2006) Telemedicine in subâ€Saharan Africa: The case of teleophthalmology and eye care in Ethiopia. J Ame Society Inform Scien Technol 57: 1383-1393.
- Gagnon MP, Orruño E, Asua J, Abdeljelil AB, Emparanza J (2012) Using a modified technology acceptance model to evaluate healthcare professionals' adoption of a new telemonitoring system. Telemed J E Health 18: 54-59.
- Ayatollahi H, Sarabi FZP, Langarizadeh M (2015) Clinicians’ knowledge and perception of telemedicine technology. Perspect Health Inf Manag.
- Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, et al. (2009) Teleconsultation service to improve healthcare in rural areas: acceptance, organizational impact and appropriateness. BMC Health Serv Res 9: 238.
- Vieru D (2000) A model for telemedicine adoption: A survey of physicians in the provinces of Quebec and Nova Scotia. Concordia University.
- Venkatesh V, Morris MG (2000) Why don't men ever stop to ask for directions? Gender, social influence, and their role in technology acceptance and usage behavior. MIS quarterly 24: 115-139.
- Au L (2009) Assessing the potential needs for telehealth in Papua new guinea (PNG).
- Chau P Y, Hu PJH (2002) Investigating healthcare professionals’ decisions to accept telemedicine technology: An empirical test of competing theories. Information and management 39: 297-311.
- Alkmim MB, Marcolino MS, Figueira RM, Sousa L, Nunes MS, et al. (2015) Factors associated with the use of a teleconsultation system in Brazilian primary care. Telemedicine and e-Health 21: 473-483.
- Larcher B, Arisi E, Berloffa F, Demichelis F, Eccher C, et al. (2003) Analysis of user-satisfaction with the use of a teleconsultation system in oncology. Medical Informatics and the Internet in Medicine 28: 73-84.
Citation: Abushaar LA, Ismail A (2018) Acceptance of Tele-Consultation and its Determinant Factors among Doctors in Outpatient Clinics in the Hospital of Conselor Tuanku Muhriz, Kuala Lumpur, Malaysia. J Community Med Health Educ 8: 606. DOI: 10.4172/2161-0711.1000606
Copyright: © 2018 Abushaar LA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6031
- [From(publication date): 0-2018 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 5078
- PDF downloads: 953