Biorisk Management Practices in Public and Private Laboratories in Uganda: A Nationwide Baseline Survey
Received: 27-Jun-2018 / Accepted Date: 09-Aug-2018 / Published Date: 15-Aug-2018 DOI: 10.4172/2157-2526.1000164
Abstract
Introduction: Uganda is one of the Phase one prioritized countries by Global Health Security Agenda tasked to develop an interagency roadmap for establishment of robust biosafety and biosecurity systems and networks. Several initiatives have been undertaken by the Central Public Health Laboratories-Ministry of Health in partnership with partners to strengthen bio risk management utilizing a multispectral approach. The program performance was monitored through uncoordinated, facility specific supervisory visits focused on a relatively narrow and specific component of biosafety and biosecurity. This study utilized a national standardized quantifiable tool that enabled assessment of comprehensive status of the national biosafety biosecurity performance, comparison of BRM performance across service delivery levels and guide the development of a nationwide implementation roadmap.
Methodology: The national, standardized, and quantifiable score based tool was used to assess individual laboratories on bio risk management elements. The questionnaire was administered to biosafety officers, hub coordinators, lab managers, and facility in-charges of 210 public and private laboratories in 100 districts of Uganda.
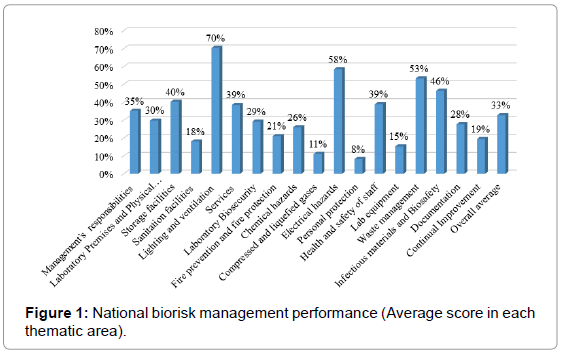
Results: Overall, national bio risk management performance in both public and private laboratories scored 33%. Performance as per level of service delivery was 52% in RRH, 43% in General Hospital and <30% in HC IV and HC III and specialised labs like Uganda Blood Transfusion Services and Masaka district veterinary laboratory. Regionally, Moroto health region registered the best overall performance at 50%, followed by Kampala (42%) while Fort portal, Jinja, Lira, Mbale and Mbarara scored below 30% each.
Conclusion and recommendations: This performance renders laboratories in the country as an eminent source or recipient of bio-threats. The Ministry of Health and other stakeholders need to refocus on key strategic areas like enactment of biosafety and biosecurity law, improve on infrastructure, tripartite training and increase awareness by establishing a national Centre of excellence for biosafety and biosecurity capacity building.
Keywords: Biosafety; Biosecurity; Bio risk; Bio risk management; Bio threat; Bioterrorism
Introduction
Biological Laboratories are critical facilities for conducting diagnosis, epidemiological surveillance and scientific research on infectious diseases that have plagued humans and animals throughout history. However, Laboratories can be dangerous if manipulations are done with bad intentions, which often result into endangering public health security [1]. The handling, processing and multiplication of biological/infectious agents and toxins habitually expose personnel, community and environment to risk of infections, injuries and other harms-attested to by the nine cases of SARS in Beijing community resulting from laboratory acquired infection [2]. Similarly, infection of co-workers by a lab technician with Shigella dysenteriae type 2 from a hospital’s collection and the use of Bacillus anthracis that was believed to have originated from a U.S. biodefense laboratory in the 2001 letter attack are some of the documented biosafety and biosecurity incidents of international concern [3]. Prevention and control of risks associated with biological agents-or Biorisk Management (BRM)-takes account of both biosafety and biosecurity aspects, and requires a variety of health (human and animal) system capacities [4-6]. Subsequently, with increasing laboratory capacity in the low and middle income countries, biosafety and biosecurity has become a significant theme in Global Health Security Agenda (GHSA) [7,8]. Conventionally, biosafety refers to “principles, technologies, practices, and measures implemented to prevent the accidental release of, or unintentional exposure to pathogenic agents” while biosecurity refers to the “protection, control, and accountability measures implemented to prevent the loss, theft, misuse, diversion, or intentional release of pathogenic agents and related resources as well as unauthorized access to, retention or transfer of such material” [6,9]. The risks associated with biological materials can be eliminated or reduced by establishing tiered mitigation control measures such as risk transfer or substitution, engineering and administrative controls, ensuring proper work practices and use of personal protective equipment [10,11]. In developed regions, regulations for safe operations in animal and human health laboratories exist [2,12-14]. However, regardless of these containment standards, laboratory accidents with unintentional exposure and or intentional release do occur [15]. Despite extensive documentation of occurrence of these infections in developed countries, paucity of information still exists in low income countries [16]. In Uganda, the magnitude of these infections, injuries and contamination arising from public and private laboratories either from human or veterinary sector remains largely unknown. Similarly, the increased volume of biological specimens moving from one point to another through the current hub system presents an imminent biosafety and biosecurity avenues [17]. These biosafety and biosecurity threats are further heightened by non-existent biobanking management, weak laboratory regulations, emergence and re-emergence of infectious pathogenic agents such as Ebola, Yellow fever and Marburg [18-20]. Additionally, there is increasing potential application of traditional agents such as Helminths (21), multidrug resistant bacteria and rift valley fever virus in contemporary bio-weaponisation. These quandaries renders the country as an eminent source or recipient of biothreats/bioterrorism [21-24]. Cognizant of the above, Uganda was one of the Phase one prioritized countries by GHSA tasked to develop an interagency roadmap for establishment of robust biosafety and biosecurity systems and networks [25]. Over the last 5 years, Central Public Health Laboratories-Ministry of Health (CPHL-MOH) in partnership with Implementing and Development partners have undertaken several initiatives to strengthen BRM at all health and veterinary laboratories embracing One Health Agenda. For instance, development of a national BRM Policy, establishment of national multi-sectorial Biosecurity Engagement committee, developing a National Harmonized BRM curriculum and trainings among others. In addition, several regulatory approaches to limit unauthorized access to biological agents and toxins in laboratories are now being considered for implementation, including centralized inventory systems of select agents/pathogens and legal framework strengthening like Biosafety Biosecurity bill in Parliament. These measures are all aimed at reducing the likelihood and consequences of both accidental and intentional exposure of personnel, community and environment to biological agents while minimizing the risk that materials in the laboratory could be used maliciously. However, the performance of all these previous implemented measures and checks were qualitatively assessed using a non-customized checklist and thus the program was unable to measure the improvements despite intensive implementation activities by different stakeholders. Secondly, these assessments were conducted through uncoordinated, facility specific supervisory visits focused on a relatively narrow and specific component of biosafety. Consequently, these reports could not give a comprehensive national biosafety biosecurity status and/or performance, enable performance comparison between different service provision levels and be used to guide in developing a nationwide implementation work-plan. Subsequently, the National Biorisk management Coordination Office (NBCO) at CPHL-MOH developed a national, standardized, and quantifiable score based tool in a bid to measure individual laboratory performances on different BRM elements. This report describes current national and region specific biosafety biosecurity status, identified gaps and suggested recommendations to guide future implementation efforts and set a baseline against which these efforts will be measured.
Materials and Methods
Study design and participants
The assessment was conducted in April 2017 and it employed a cross-sectional survey design. A total of 210 laboratories from both public and private owned health laboratories were audited. The laboratories were drawn from different ministries including Health, Agriculture Animal Industry and Fisheries, Internal Affairs, Defense and Veteran Affairs. The laboratory level of service provision ranged from National reference labs (NRL), Regional reference labs (RRL), General hospital (GH), Health sub district health center IV (HC IV) and Parish levels health center III (HC III). Out of the 210 laboratories from 100 districts audited, 180 (86%) were government owned while 30 (14%) were private institutions. The government owned laboratories (Human, Military and Veterinary) comprised of Regional Referral Hospitals (n=12), General Hospitals (n=38), Health Center IV (n=67) and Health Center III (n=61). Privately owned laboratories consisted of those attached to Hospitals (n=16), Health Center IV (n=2) and Health Center III (n=12). In addition, specialized national reference laboratory, Uganda Blood Transfusion Services (n=1) and District veterinary laboratory (n=1) were assessed.
Audit checklist design and implementation
The standardized audit checklist used comprised of two parts: demographic questions and general biosafety and biosecurity questions. The checklist was developed based on the standards stipulated in the Laboratory bio risk management standard CWA 15793 document (CWA 2011; ISO: 15190, 2003; ISO: 15189, 2012; and the national harmonized Bio risk management curriculum as well as the Laboratory Biosafety Manual (3rd Edition) developed by the World Health Organization (2014). The checklist consisted of a standardized quantifiable score that allowed measurement of individual laboratory performances per BRM elements. Each independent activity/question was scored 2 marks. Activities/questions that have been batched up together were scored out of 5, 3, or 2 marks depending on their weight (complexity and importance). However, any partial or No to any one of the batched up questions earned a score of 1. Some questions were added the option of “NA” implying this question is not applicable to a particular level of laboratory and the lab cannot be assessed on it, these marks were then subtracted from the overall total when calculating the percentage. The questionnaires were purposively administered to biosafety officers, hub coordinators, lab managers, and facility incharges. Open ended questions to assess the respondents’ general knowledge of laboratory biosafety and biosecurity were administered. The interviewees were also asked about the availability and use of biosafety devices and PPE as well as availability of occupational safety and health programs. These were supplemented by review of relevant documents and records as well as observation of practice and working ethics in the facilities. The questionnaire was pretested at CPHL-MOH before deployment. The higher level participating laboratories were purposively selected while simple random sampling was employed for inclusion of the lower health facilities (HC IV & IIIs).
Data analysis
All completed checklists were transmitted back to the coordinating office at CPHL. The raw data was entered, cleaned and analyzed using excel spreadsheet. Quality of the data was achieved through validation and tested to ensure that checklist conformed to the conceptual frame work of the Audit following Amin (2003) recommended validity index of at least 0.7. The scores were transformed into percentages and displayed using graphs, tables and charts. A numeric scoring system was developed to assess all the sections and cut-off points for low / moderate / high risk scores were defined as in Table 1.
| Very high risk | High risk | Moderate Risk | Low Risk | Very low Risk |
|---|---|---|---|---|
| (Poor) | (Fair) | (Average) | (Good) | (Very good) |
| ≤ 30 % | 31%-49% | 50%-59% | 60%-79% | ≥ 80% |
Table 1: Scoring and ranking of biosafety and biosecurity risk levels in ugandan laboratories.
Results
Facility disaggregation by ownership and service delivery levels
Out of 210 laboratories audited/ assessed, 86% (180) were government owned while 14% (30) belonged to private institutions. The government owned laboratories (Health, Military and Veterinary) included RRH (n=12), GH (n=38), HC IV (n=67) and HC III (n=61). Privately owned laboratories consisted of those attached to Hospitals (n=16), HCIV (n=2) and HCIII (n=12). In addition, Uganda Blood Transfusion Services laboratory, a specialized National Reference Laboratory (n=1); and District veterinary laboratory (n=1) as shown in (Table 2). Amongst these laboratories, 34% (72) were hubs, these are facilities with improved infrastructure, diagnostic equipment and personnel, while 66% (138) were Non- hub laboratories.
| Facility levels | Ownership | ||||
|---|---|---|---|---|---|
| Public | Private | MoDV | MAAIF | MoIA | |
| RRH | 12 | 0 | |||
| GH | 37 | 16 | 1 | ||
| HC IV | 65 | 2 | 2 | ||
| HC III | 59 | 12 | 1 | 1 | |
| NSRL | 1 | 1 | |||
Foot note: NSRL=National specialized reference laboratory; RRH=Regional referral hospital; GH=General hospital; HCIV=Health center four; HCIII=Health center three; MoDV=ministry of defense and Veteran affairs; ministry of agriculture animal industry and fisheries; MoIA=ministry of internal affairs
Table 2: Number of audited facilities by ownership and service levels.
Biorisk management performance by thematic areas and regions
Overall, national BRM performance scored 33% (Figure 1), with government owned health laboratories scoring 34% while privately owned health laboratories at 33% (data not shown). Administratively, the various health facilities are designated into health regions (n=12) that are overseen by a regional referral hospital and each health region is supported by at-least one implementing partner. Moroto health region registered the best overall performance of 50%, followed by Kampala (42%) while Arua, Gulu, Hoima, Kabale, Mubende and Soroti health regions scored above 33% (Figure 2). The remaining health regions of Fort portal, Jinja, Lira, Mbale and Mbarara scored below 30% each (Figure 2). The specific performance of regional referral hospital laboratories was 52%, General Hospital laboratories scored 43%, HC IV 33% and HC III 24%, while the others (UBTS – Nakasero) and Masaka district veterinary laboratory) scored 30% each (data not shown). The overall performance of 210 laboratories assessed on the selected core sections are as below:
Management responsibilities: Facility Management and support for BRM performance was found at 33%. The role of management is to delegate mandate or authority to enforce safety practice putting in place effective BRM programs or policies. For this survey, management responsibilities were; appointment of biosafety officers with clear written roles and responsibilities; provision of training of both technical and non-technical personnel; establishing an infection prevention and control/biosafety committee, and having budget / work-plans that supports safety activities. Moroto health region emerged the best with 64% of its facilities having fulfilled management responsibilities mandate and Kampala as second (54%) while Mbarara, Masaka and Fort portal each scored below 25% (Table 3). The rest of the health regions performance ranged from 25-40%.Laboratory physical premises and biosecurity Laboratory premises and physical security were assessed for adherence to the laboratory level specific national infrastructure guidelines, availability of protection from external disasters/threats such as lighting conductors, burglary proofs, security guards, secure perimeter fence as well as appropriateness of physical working environment. The study observed that only 30% of the assessed laboratories conformed to the national infrastructure guidelines for construction. Relatedly, this survey found that 29% of the facilities were practicing biosecurity measures such as pathogen inventory, risk assessment and documented access control measures to sample/isolate storage areas. Remarkably 13% of the facilities had defined risks and incidence response plans. Moroto, Kampala and Hoima health regions observed the best performance (above 45%) in both physical premise and laboratory biosecurity measures. The worst performing health regions were Lira (13%), Jinja, Mbale, Gulu and Fort portal each with an average 20% (Table 3). Additionally, 75% of facilities had sockets located above the worktop and away from sinks and other wet places. Appropriateness of the storage facility, controlled and documented access of the store were among other items considered.
| Health regions | Occupational health and safety %(n/N) | Premise & physical security %(n/N) | Management of infectious agents %(n/N) | Lab safety equipment %(n/N) | Chemical hazard management %(n/N) | Waste management %(n/N) | Management responsibility %(n/N) |
|---|---|---|---|---|---|---|---|
| Arua | 39.2 (5.1/13) | 41.5(5.4/13) | 58.4(11.1/19) | 11.4 (0.8/7) | 28.0 (1.4/5) | 66.0 (6.6/10) | 38.4 (7.3/19) |
| Fort Portal | 35.4 (4.6/13) | 29.2 (3.8/13) | 32.1 (6.1/19) | 12.9 (0.9/7) | 10.0 (0.5/5) | 52.0 (5.2/10) | 25.3 (4.8/19) |
| Gulu | 31.5 (4.1/13) | 36.7 (4.9/13) | 72.3 (9.4/19) | 14.3 (1.0/7) | 22.0 (1.1/5) | 53.0 (5.3/10) | 40.0 (7.6/19) |
| Hoima | 37.7 (4.9/13) | 47.7 (6.2/13) | 41.1 (7.8/19) | 17.1 (1.2/7) | 30.0 (1.5/5) | 50.0 (5/10) | 48.4 (9.2/19) |
| Jinja | 30.7 (4.0/13) | 33.1 (4.3/13) | 37.9 (7.2/19) | 15.7 (1.1/7) | 24.0 (1.2/5) | 44.0 (4.4/10) | 33.7 (6.4/19) |
| Kabale | 53.1 (6.9/13) | 33.1 (4.3/13) | 60.5 (11.5/19) | 15.7 (1.1/7) | 36.0 (1.8/5) | 64.0 (6.4/10) | 31.1 (5.9/19) |
| Kampala | 56.2 (7.3/13) | 46.2 (6.0/13) | 55.8 (10.6/19) | 25.7 (1.8/7) | 36.0 (1.8/5) | 76.0 (7.6/10) | 54.7 (10.4/19) |
| Lira | 31.5 (4.1/13) | 18.5 (2.4/13) | 28.4 (5.4/19) | 14.3 (1.0/7) | 12.0 (0.6/5) | 40.0 (4.0/10) | 25.8 (4.9/19) |
| Masaka | 35.4 (4.6/13) | 40.7 (5.3/13) | 45.8 (8.7/19) | 17.1 (1.2/7) | 42.0 (2.1/5) | 46.0 (4.6/10) | 22.1 (4.2/19) |
| Mbale | 35.4 (4.6/13) | 33.8 (4.4/13) | 39.5 (7.5/19) | 14.3 (1.0/7) | 24.0 (1.2/5) | 49.0 (4.9/10) | 33.2 (6.3/19) |
| Mbarara | 26.2 (3.4/13) | 24.5 (3.2/13) | 40.0 (7.6/19) | 11.4 (0.8/7) | 14.0 (0.7/5) | 42.0 (4.2/10) | 24.7 (4.7/19) |
| Moroto | 66.2 (8.6/13) | 47.7 (6.213) | 67.4 (12.8/19) | 20.0 (1.4/7) | 52.0 (2.6/5) | 72.0 (7.2/10) | 64.2 (12.2/19) |
| Mubende | 36.2 (4.7/13) | 46.9 (6.1/13) | 52.1 (9.9/19) | 22.9 (1.6/7) | 40.0 (2.0/5) | 60.0 (6.0/10) | 33.7 (6.4/19) |
| Soroti | 41.5 (5.4/13) | 40.7 (5.3/13) | 47.9 (9.1/19) | 12.9 (0.9/7) | 24.0 (1.2/5) | 58.0 (5.8/10) | 39.5 (7.5/19) |
Table 3: Performance of health sub regions in key thematic area.
Chemical hazard management: The level of awareness of the hazards associated with chemicals as well as their management revealed a 26% compliance level by all facilities combined (Figure 1). For this survey, chemical management components included availability of an updated chemical inventory; chemical hazard/hygiene plan, material safety data sheet, a chemical spill kit and training in use, transportation and knowledge of handling chemical spillages. Relatedly, Health region performance in chemical hazard management varied; Moroto (52%), Masaka (42%), Mubende (40%), while Kampala and Kabale had 36% each. This survey showed that Mbarara, Fort portal and Lira health regions had the worst performance in chemical hazard management with each scoring below 15% (Table 3).
Occupational health and safety programs: Occupation health and safety programs such as functional / active medical checks and vaccination programs, protocols for reporting lab infections/accidents and presence of first aid kits as well as training in first aid management were evaluated. An overall national score of 39% (Figure 1) was registered. Specifically, only 9.5% (20) of all laboratories assessed had an established and functional medical surveillance program in place. Nonetheless, 61% had fully vaccinated personnel against Hepatitis B virus, while 74.8% (157) and 46.7% (98) had PEP program and First Aid kits available at strategic locations respectively. However, only 27% of the sites had had their staff trained in first aid provision and 70% (147) had hazard communication signs appropriately displayed. The results show that Moroto health region had the most facilities (66%) with an established and functional occupational health and safety programs whereas Kampala and Kabale scored 56 and 53% respectively (Table 3). Health regions of Lira, Gulu and Jinja had the least performance of below 22%.
Laboratory safety Equipment (Primary and secondary bio-containment): The study revealed that the ability of these laboratories to physically restrain pathogenic agents by isolation in an environmentally and biological secure cabinets was poor. Laboratory equipment like biosafety cabinets, fume hoods, autoclaves, centrifuges as well as functional maintenance plans for all these equipment scored a paltry 15% (Figure 1). Kampala, Mubende and Moroto health regions demonstrated a 25%, 23% and 20% compliance respectively while Arua and Mbarara each scored about 11%. The remaining health regions had between 12-17% (Table 3).
Waste management: The proportion of facilities with waste management systems in place was 53%. The audit scope ranged from availability of waste management protocols or manuals, proper PPE for waste handlers as well as provision of waste bins and disposal methods. Most facilities did not have written protocols for waste management as well as proper PPE for waste handlers. Ministry of Health through central public health laboratories develops and disseminates reference materials including guidance on proper waste management practices among others. Compared to the other key aspects assessed, waste management compliance was best in Kampala health region facilities (76%), followed by Moroto (72%) while Mubende, Kabale and Arua scored above 60% each. Mbarara, Lira, Jinja and Masaka health regions had the most facilities with the least compliance of about 40% (Table 3).
Infectious / biological material handling and accountability: This survey found that management of infectious agents as measured by proportion of facilities with personnel trained in infectious materials shipment, in addition to protocols for storage, retrieving and transportation of biological materials was 46%. Regional Referral Hospitals scored 65%, GH at 53.7%, HC IVs at 47% and HC IIIs scoring 36%. Out of all facilities audited, 25% (53) had specimen reception procedures (SOPs) in place and adhered to by the lab personnel. Majority of facilities 68% (143) had inadequate or undocumented procedures. Only 25% (53) facilities had proper infectious substance systems in place that included effective tracking and handling of infectious substance, protocols for reporting missing biological specimen and staff fully aware of procedures for dealing with breakage and spillage. Gulu health region performed better in this basic standard (72%), followed by Moroto (67%), Kabale, Arua and Kampala at 60%, 58% and 55% correspondingly (Table 3). Lira was the poorest performer in infectious material management systems.
Personal protective equipment: A poor protection level of laboratory workers against laboratory borne infections and injuries was recorded. Supply and use of personnel protection equipment (PPE), which forms the basis of protection to laboratory personnel during work scored 35%. Key PPEs evaluated included gloves, goggle/ face shields, closed shoes, respirators, lab coats, eye wash stations and emergency showers among others.
Documentation and continual quality improvement
The remaining section scored as follows; Compressed and liquefied gases (11%), electrical hazards (58%), documentation (28%), and BRM related continual improvement (19%) indicating a poor commitment to improve laboratory processes towards standard BRM.
Biosafety officers’ appointment per service delivery level
Out of 210 facilities audited, only 39% of facilities had biosafety or infection prevention and control committees in place. About half of facilities with biosafety committees’ had documented biosafety officers to oversee BRM activities in the work place. Appointment letters and terms of reference assigned to the BSO served as evidence for management responsibilities. Out of the 49.5% delegated Biosafety officer, the majority were in public health facilities (88.5%); with 18% of these facilities being at HCIII, RRH (12%), General District Hospitals (36%) and HCIVs with 34% (Figure 2).
Discussion
We report for the first time the national status of biorisk management practices across both public and private health laboratories in Uganda. The performance of national biorisk management status in both public and private healthcare laboratories stands at 33% after more than 5 years of biorisk management implementation. This percentage is far below the proportion reported in other developing countries and in sharp contrast to the proportion reported among different professionals in Uganda [1,26,27]. The inclusion of human and animal research facilities, crop protection and wildlife laboratories in a study conducted by Kirunda et al, 2014, paralleled to this study could lend a probable account for the observed differences. The current study focused on human health laboratories and therefore included only one veterinary facility which could be a potential misrepresentation of veterinary laboratories. The subsequent surveys should however, provide a representative sample of both veterinary and human health facilities considering the zoonotic nature of most infectious agents and also strengthen the ‘One Health concept” [28,29]. Additionally, this study utilized a national standardized score based audit checklist that was comprehensive and very restrictive. This scoring, done for the first time could have attributed to the observed differences. Inferring biosafety and biosecurity practices in facilities by level of health service provision revealed that Regional Referral Laboratories-albeit a limited number-scored the highest as compared to laboratories at the General Hospital and HC IV or HC III levels. This is not surprising considering their ongoing participation in Strengthening Laboratory Management Towards Accreditation program (SLMTA) [30], level of Hospital management commitment and funding from various implementing partners as well as the recent renovations/refurbishments of all Regional Referral laboratories that helped improve organizational and safety measures. These results allude that implementation of biosafety and biosecurity measures require management support to establish policies, biosafety committees, designate and support performance of biosafety officers as well as secure resources for implementation of safety practices [10,31]. Conversely, this study revealed an overall low levels of facility management awareness regarding national and international laws and/or policies pertaining to laboratory biosafety and biosecurity, as attested by only 35% of the facilities assessed, having documented commitment to enforce safety practice and policies. This inadequate knowledge and commitment by management indicate a glaring shortfall in laboratory biosafety and biosecurity systems and lends an urgent call to address this gap especially in the face of emerging and re-emerging infectious disease agents in Uganda. Although this report conflicts with assessment conducted by FAO 2015, in central veterinary laboratories in four African countries-including Uganda it does conquer with similar findings in veterinary research facilities in Nigeria [32,33]. Additionally, poor knowledge and management commitment was further evidenced by few facilities having established and functional occupation health and safety programs such as medical surveillance and vaccination programs. The authors are aware that the Uganda National Expanded Program on Immunization (UNEPI) covers immunizations against most childhood disease and data from routine immunization coverage is part of the Uganda monthly Health Management Information Systems; especially the proportion of the “fully immunized child” [34]. However, we recommend extension of monitoring and vaccination of all healthcare personnel in both public and private facilities who are at the forefront of outbreak casualties. Specifically, only 9.5% of all laboratories assessed had established and functional medical surveillance program in place and about 61% of those laboratories had fully vaccinated personnel against Hepatitis B virus. Low medical surveillance and vaccination programs coupled with inadequate basic personal protective equipment and waste management practices, indicate institutional incapacity to protect the personnel, community and environment against highly pathogenic agents such as Anthrax, Hepatitis B, Ebola and Marburg [35]. Specimens of these agents are supposed to be handled under biosafety level IV containment facilities and procedures but are often first handled at much lower level facilities in-case of outbreaks in the country. Most of the respondents in public facilities cited inadequate safety supplies and meagre budgets allocated for facility biorisk management as well as lack of delegated Biosafety officers. It is therefore, eminent that all stakeholders should contribute to ensure that adequate biosafety principles, technologies and practices are instituted to help prevent unintentional exposure to pathogens and toxins, or their accidental release. Furthermore, laboratory biosecurity measures should be instituted to ensure protection, control and accountability for valuable biological materials and information within laboratories, in order to prevent their unauthorized access, loss, theft, misuse, diversion or intentional release. This will require an integrated approach that encompasses both policy and regulatory frameworks. One of the habitually employed and recommended measure for effective biosecurity is engineering controls. However, observation that majority of the surveyed institutions lacked adequate measures aimed at preventing the misuse of dangerous pathogens negate the BTWC and UN resolution 1540 [9], and reflects an increased risk of access to dangerous pathogens. The low compliance by the facilities could be attributed to lack of awareness and unavailability of national laboratory infrastructure guidelines at facility level as well as resources to implement the standards [27]. Since most of these establishments are repurposed to assist during the recurrent outbreaks of highly dangerous pathogens in Uganda, coupled with increased volume of biological samples moving from one point to another through the current hub system, dual-use opportunities are more eminent if preventive interventions are not implemented. Although the nature and volume of biological materials handled in public and private laboratories were not assessed in this study, conforming to global standards that restrict access to dangerous pathogens would help reduce the threat of bioterrorism, as well as fulfil the legal requirement contained in the 1972 Biological Weapons Convention [9]. In light of the above, there is need for a countrywide documentation of the nature and volumes of biological materials/agents handled in the different laboratories. We also observed an unsatisfactory performance in documentation and continual improvement measure towards BRM in the assessed facilities. This was accentuated by lack of reporting mechanism/ procedures of biosafety and biosecurity incidents from the facility to the national level. Incidents such as seroconversion due to needle stick injuries, occupationally acquired TB and Hepatitis infections cannot be accurately assessed without proper documentations of incidents / occurrences. It is therefore necessary that CPHL-MOH develops a national reporting procedures to enable tracking for all occupational incidents / occurrences to provide evidenced based policy guide. Taken together, the results of this study calls for an urgent need for promoting biosafety and biosecurity within the health laboratories to avoid the emergence of dual-use and protect against accidental release of pathogens into the environment. Although biosafety and biosecurity surveys have been conducted in various sectors in the country this is the first study to comprehensively document BRM status in public and private health laboratories in Uganda [27].
Conclusion and Recommendations
Results from 210 laboratories assessed indicate an overall 33% BRM performance, with negligible variation between public (34%) and those in private sector 33%. The Ministry of Health and its Development/ Implementing Partners and other sectors need to refocus on key strategic areas that will stimulate involvement of all stakeholders. These critical areas includes: (i) Enactment of biosafety and biosecurity law to provide an environment for enforcement of biosafety biosecurity policies; (ii) All Laboratories should be mandated to have designated biosafety officers to promote facility based biosafety biosecurity policy awareness and implementation; (iii) Promote tripartite trainings including facility administrators. Refocused engagement of facility Managers will stimulate performance improvement, promote ownership and foster prioritization of biosafety related operations. This can be further augmented by comprehensive onsite technical support supervision and mentorships; (iv) Targeted procurement of assorted biosafety and waste management equipment and supplies; (v) Overhauling all the health laboratory facilities based on national infrastructure guideline, implementing physical engineering controls and waste management practices. Lastly, establishing a national Centre of excellence for biosafety and biosecurity capacity building in the country will promote one health training and increase awareness among different sectors.
Acknowledgement
The authors are grateful to all laboratory Development and Implementing partners for funding this survey. We wish to acknowledge the efforts of all the national Biosafety Biosecurity trainers who participated in data collection. We are very grateful to the management and respondents of the institutions for their participation.
Author Contributions
1. Atek Kagirita and Tonny Jimmy Owalla conceived, conducted and drafted the first manuscript.
2. Andrew Baguma, Paul Okwalinga, Joel Opio, conducted the study and reviewed the first draft.
3. Rodney Mugasha, Francis Kakooza, Rita Eragu and Sulaiman Ikoba performed the data analysis.
4. Amato Ojwiya, Steven Aisu, Ambrose K. Musinguzi supported documenting the study, technical guidance and drawing conclusion
5. Susan Nabadda and Diana Atwine spearheaded the study.
All authors read and reviewed the final copy of the manuscript.
References
- Jennifer G, Tamara Z ( 2007) Survey of  Bioscience Research Practices in Asia: Implications for Biosafety and Biosecurity. Applied Biosafety 12: 260-267.
- World Organization for Animal Health (OIE) (2014) Standard for managing biorisk in the veterinary laboratory and animal facilities. Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (2014).
- Salerno RM, Gaudioso J, Frerichs RL, Estes D (2004) A BW Risk Assessment: Historical and Technical Perspectives. The Non-proliferation Review 11: 25-55.
- Tran PD, Vu LN, Nguyen HT, Phan LT, Lowe W, et al. (2014) Strengthening global health security capacity–Vietnam demonstration project, 2013. MMWR Morb Mortal Wkly Rep 63: 77-80.
- Borchert JN, Tappero JW, Downing R, Shoemaker T, Behumbiize P, et al. (2014) Rapidly building global health security capacity–Uganda demonstration project, 2013. MMWR Morb Mortal Wkly Rep 63: 73-76.
- Bakanidze L, Imnadze P, Perkins D (2010)Â Biosafety and biosecurity as essential pillars of international health security and cross-cutting elements of biological non-proliferation. BMC Public Health 10: S12.
- Caceres SB (2011) Global health security in an era of global health threats. Emerg Infect Dis 17: 1962-1963.
- BTWC (2006) Sixth review conference of the state’s parties to the convention on the prohibition of the development, production and stockpiling of bacteriological (biological) and toxin weapons and on their destruction. Biological and Toxin Weapons Convention (BTWC) 6th Review Conference, Geneva.
- Adel NZ (2010) Biosafety and biosecurity measures: management of biosafety level 3 facilities. Int J Antimicrob Agents 36: S70-S74.
- Public Health Agency Canada (PHAC) (2013) Canadian Biosafety Standards and Guidelines for Facilities Handling Human and Terrestrial Animal Pathogens, Prions, and Biological Toxins (2013).
- Occupational Safety and Health Administration (OSHA) Laboratory Safety Guidance (2011).
- Centers for Disease Control (CDC) (2009) 5thed Principles in biosafety. Biosafety in Microbiological and Biomedical Laboratories (BMBL).
- Gunther S, Feldmann H, Geisbert TW, Hensley LE, Rollin PE, et al. (2011) Management of accidental exposure to Ebola virus in the biosafety level 4 laboratory, Hamburg, Germany. J Infect Dis 3: S785-S790.
- Centers for Disease Control (CDC) (2015) Report on the Potential Exposure to Ebola Virus. CDC website: CDC. (2015).
- Katongole ME (2009) Assessing the Meaning and Scope of Biosafety and Biosecurity in the Context of Uganda - Paper presented at the Open Session of the UNAS consensus study (“Advancing the National Dialogue through a Universal Understanding of Biosafety and Biosecurity in Ugandaâ€), 10 June 2009, Hotel Africana, Kampala.
- Kiyaga , Charles K, Sendagire H, Joseph E, Connell IMc, et al. (2013) Uganda’s New National Laboratory Sample Transport System: A Successful Model for Improving Access to Diagnostic Services for Early Infant HIV Diagnosis and Other Programs. PLoS ONE 8: e78609.
- Mbonye A, Wamala J, Winyi-Kaboyo, Tugumizemo V, Aceng J, et al. (2012) Repeated outbreaks of viral hemorrhagic fevers in Uganda. Afr Health Sci 12: 579-583.
- Mbonye AK, Wamala JF, Nanyunja M, Opio A, Makumbi I (2014) Ebola viral hemorrhagic disease outbreak in West Africa- lessons from Uganda. Afr Health Sci 14: 495-501.
- Knust B, Schafer IJ, Wamala J, Nyakarahuka L, Okot C , et al. (2015) Multidistrict Outbreak of Marburg Virus Disease-Uganda, 2012. J Infect Dis 212: S119-128.
- Kwak ML (2016)Â Helminths as Weapons of Bioterrorism: an Unrecognised Threat. J Bioterror Biodef 7: 148
- Ceccarelli G, Ceccarelli C, Pacifici LE (2013) Circulation of Multidrug Resistant Pathogens between Developed and Developing Countries: A New Frontier of Biodefense. Implication for Policy Makers. J Bioterr Biodef 4: e109.
- Cogliati S, Costa JG, Ayala FR, Donato V, Grau R (2016) Bacterial Spores and its Relatives as Agents of Mass Destruction. J Bioterror Biodef 7: 141.
- Mandell RB, Flick R (2011) Rift Valley Fever Virus: A Real Bioterror Threat. J Bioterr Biodef 2: 108.
- Sikandar KS, Rasheed F, Amin T, Jeelani R, Kazmi SU (2010) An evaluation of current biosafety practices in pathogical laboratories of Korachi, Pakistan Administrator.
- Kirunda H, Maxwell OO (2014) Low Level of Awareness in Biosafety and Biosecurity among Professionals in Uganda: A Potential Risk in the Dual-Use Dilemma. J Bioterror Biodef 5: 128.
- Nessan D, Robert K (2000) Prevalence and control of zoonotic diseases: collaboration between public health workers and veterinarians in Burkina Faso. Acta Tropica 76: 53-57.
- Destoumieux-Garzón D, Mavingui P, Boetsch G, Boissier J, Darriet F, et al. (2018) The One Health Concept: 10 Years Old and a Long Road Ahead. Frontiers in Veterinary Science.
- Yao K, Luman ET (2014) SLMTA Collaborating Authors. Evidence from 617 laboratories in 47 countries for SLMTA-driven improvement in quality management systems. Afr J Lab Med 11.
- Heckert RA, Reed JC, Gmuender FK, Ellis M, Tonui W (2011) International biosafety and biosecurity challenges: suggestions for developing sustainable capacity in low-resource countries. Appl Biosaf 16: 223e30.
- Food and Agricultural Organisation of the United Nations (2015) Biosafety/biosecurity: national veterinary laboratories assessed in fur African countries.
- Ismail AO, Afusat TJ, Bernard AO, Yiltawe SW,  Adisa RI, et al. (2017) Status of Laboratory Biosafety and Biosecurity in Veterinary Research Facilities in Nigeria. Saf Health Work 8: 49-58.
- UNAS (Uganda National Academy of Sciences) (2010) The Scope of Biosafety and Biosecurity in Uganda Policy Recommendations for the Control of Associated Risks, a Consensus Study Report.
- Gangadharan D, Smith J, Weyant R (2013) Biosafety Recommendations for Work with Influenza Viruses Containing a Hemagglutinin from the A/goose/Guangdong/1/96 Lineage. MMWR Recomm Rep 62: 1-7.
Citation: Atek AK, Owalla TJ, Baguma A, Okwalinga P, Opio J, et al. (2018) Biorisk Management Practices in Public and Private Laboratories in Uganda: A Nationwide Baseline Survey. J Bioterror Biodef 9:164. DOI: 10.4172/2157-2526.1000164
Copyright: © 2018 Atek AK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4656
- [From(publication date): 0-2018 - Dec 12, 2025]
- Breakdown by view type
- HTML page views: 3731
- PDF downloads: 925