Research Article Open Access
Demography and Short Term Outcome of Tuberculous Lymphadenitis; A Case Series from Central Srilanka
Madegedara D1*, Nandedeva D2 and Yasaratne BMGD21Respiratory Disease Treatment Unit II, Teaching Hospital, Kandy, Srilanka
2Consultant respiratory physician, Srilanka
- *Corresponding Author:
- Dushantha Madegedara
Respiratory Disease Treatment Unit II
Teaching Hospital, Kandy, Srilanka
Tel: 0094812384374
E-mail: dmadegedara@yahoo.com
Received Date: November 15, 2016; Accepted Date: December 19, 2016; Published Date: December 27, 2016
Citation: Madegedara D, Nandedeva D, Yasaratne BMGD (2016) Demography and Short Term Outcome of Tuberculous Lymphadenitis; A Case Series from Central Srilanka. J Tuberc Ther 1:101.
Copyright: © 2016 Madegedara D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Tuberculosis and Therapeutics
Abstract
Objective: To delineate the pattern of tuberculous lymphadenitis (TBL) and the short-term outcome following routine practice, in an endemic setting with an intermediate disease burden.
Setting: Respiratory Disease Treatment Unit (RDTU), Kandy, Sri Lanka.
Methodology: A retrospective study of TBL patients treated with ATT during the period from year 2008 January-2011 December was performed. Clinic records were reviewed and an interviewer administered questionnaire was used to assess treatment outcome.
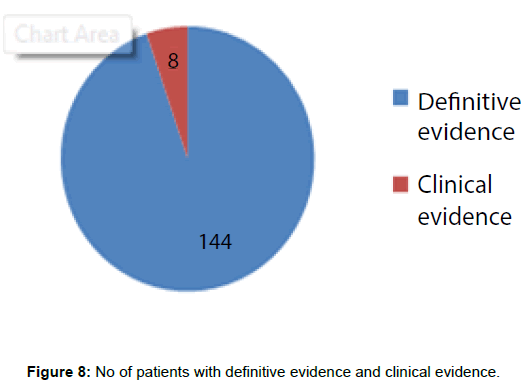
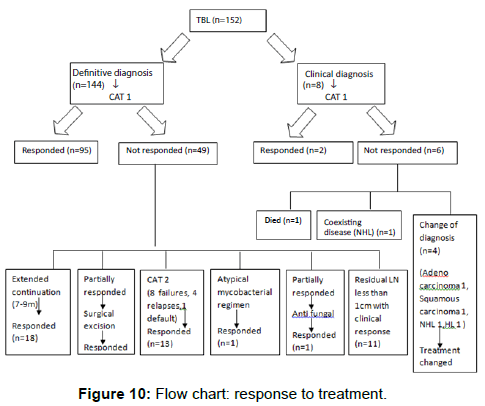
Results: A total of 152 patients with isolated peripheral lymph node TB were listed in the database. All of them had undergone lymph node sampling. Microbiological investigations were performed only in 38 occasions. Hundred and forty four patients were started treatment according to definitive evidence and all of them had good response. Eight patients were started treatment on clinical evidence; out of them the diagnosis was changed later in four patients.CAT 2 regimen was given for only 13 patients during our study. After cessation of treatment, relapses were not detected to date.
Conclusion: We noted that the microbiological studies were heavily underutilized among patients with TBL referred from other units to RDTU. However histology based diagnosis followed by standard ATT appeared safe and effective. Even though a trial of ATT may be warranted occasionally on clinical grounds alone, these patients need close follow up to exclude co-existing/alternative pathologies. Also we noted that the adverse drug reactions were very low and response to first line ATT was high. There were no instances of drug resistance.
Keywords
Extra pulmonary tuberculosis; Lymph node; Antituberculous treatment (ATT)
Introduction
Tuberculosis (TB) remains a public health concern worldwide particularly in third world countries where incidence is high. Sri Lanka is a country with intermediate disease burden with 9328 cases in 2010 (Quarterly returns of District Chest Clinics, 2010). Lymph node tuberculosis is the most frequent extra pulmonary localization. In the developing world, 43% of cases of peripheral lymphadenopathy are due to TB [1]. In rural India the prevalence of TB lymphadenitis (TBL) in children up to 14 years of age is approximately 4.4 cases per thousand [2]. In United States about 20% of patients with TB have extra pulmonary tuberculosis (EPTB) and TBL accounts for about 30-40% of EPTB [3-5]. Due to demographic transitions and the high prevalence of HIV, TB remains a major burden in both the developed and developing world to date.
Detailed information regarding TBL is scarce in the WHO database. Published information is focused mainly on demography. Data regarding the performance of diagnostic methods, therapeutic strategies and outcome are limited in scope.
The behavior and treatment response of patients with TBL is known to differ. A controlled clinical trial by the British Thoracic Society revealed the “paradoxical behavior” of lymph node TB, with some patients developing new lymphadenopathy and sinus formation despite treatment in the absence of culture confirmed relapse [6]. The study also revealed no difference in outcome between 6 and 9 months of treatment. Although these events are documented in clinical trials, [6-9] they are yet perceived by some clinicians as treatment failure or relapses.
Studies regarding these aspects have not been conducted in Sri Lanka, despite TBL being a major health problem. Therefore, we evaluated the demographic characteristics, diagnostic approaches, therapeutic strategies and outcome of treatment in patients with confirmed TBL undergoing standard Category 1 treatment in an endemic setting.
Objective
To delineate the pattern of tuberculous lymphadenitis (TBL) and the short-term outcome following routine practice, in an endemic settingwith an intermediate disease burden.
Methodology
We performed a retrospective analysis of TBL patients diagnosed during 2008-2011 at the Respiratory Disease Treatment Unit (RDTU), Teaching Hospital Kandy, Sri Lanka.
All tuberculosis (TB) patients diagnosed in Kandy District, Central Sri Lanka are required to be registered at RDTU and were incorporated in this study. We recruited all patients diagnosed with TBL during 2008-2011 from the TB registry. Case definition criteria, based on National guidelines for extra-pulmonary tuberculosis (EPTB), were (i) presence of microbiological (smear, culture, TB-PCR) and/ or (ii) histological evidence of TBL on lymph node sampling or (iii) strong clinical evidence consistent with TBL. Patients presenting with pulmonary tuberculosis and concurrent lymph node (LN) enlargement were excluded from the series.
All interventions were carried out as part of the routine clinical management. Strict confidentiality was maintained regarding patient records.
Clinic records of all recruits were reviewed with regard to symptomatology, biochemistry, microbiology, histology and radiology at the time of diagnosis. All patients were interviewed using an interviewer administered questionnaire. The treatment outcome was assessed clinically and biochemically. Descriptive statistics (percentages) were used in data analysis. Statistical analysis was carried out using Microsoft EXCEL 2007 software.
Results
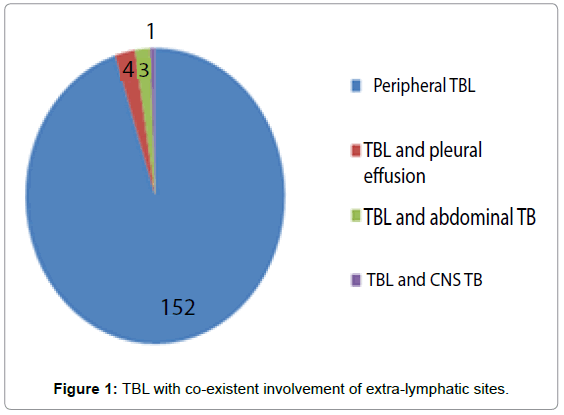
There was a total of 3410 (average 852 per annum) TB patients registered at RDTU Kandy during the study period. Out of 933 (27.4%) patients with EPTB, 152 (16.29%) with isolated TBL were recruited for this study. Additionally, eight patients, excluded from the study were noted to have TBL with co-existent involvement of extra-lymphatic sites (Figure 1).
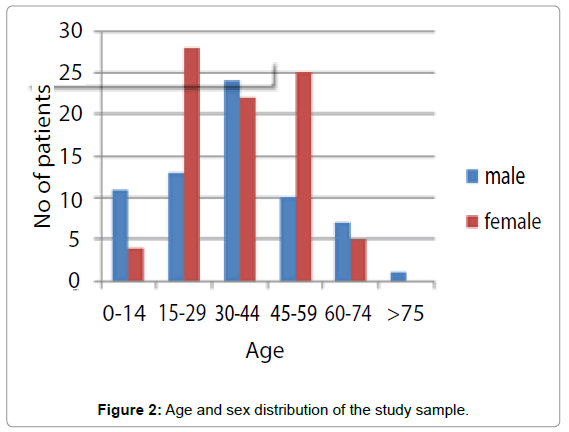
There were 86 females (56.57%) and 76 males. The mean age of the study sample was 35.97 years with a range of six months to 80 years (Figure 2).
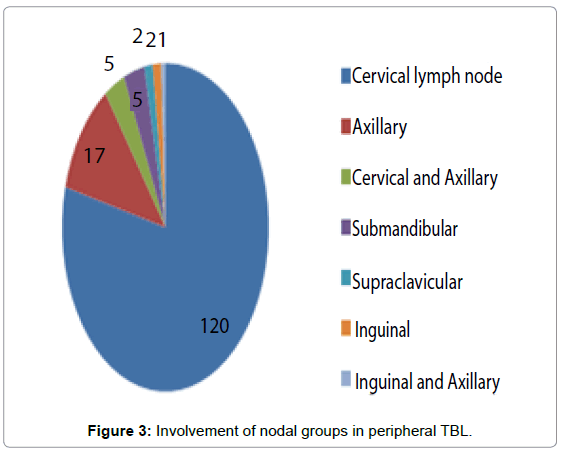
Of patients with peripheral TBL alone, majority (78.94%) had isolated cervical lymphadenopathy, while multiple lymphatic sites were involved in 3.94% (Figure 3). There were 2 patients with mesenteric lymphadenitis and 1 patient with hilar lymph adenopathy, but they had involvement of other extra lymphatic sites as well. Out of patients with single nodal site involvement, 55% had single lymph node enlargement while only 45% had multiple LN enlargement.
All 152 patients presented with swelling over the lymphatic site and constitutional symptoms were noted in 40.78%. A positive contact history of tuberculosis was identified in ten patients (smear positive pulmonary TB in 8, smear negative pulmonary TB in 1, EPTB in 1). BCG scar was positive in 90.16% of patients.
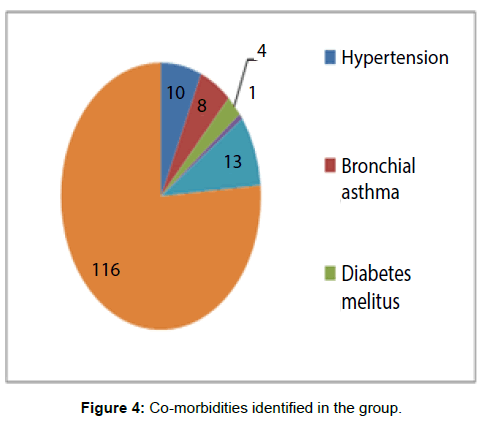
Hypertension was the commonest co-morbidity identified in the group 10 (6.57%), while bronchial asthma 8 (5.26%), diabetes mellitus 4 (2.63%) and chronic renal failure 1 (0.65%) were also noted (Figure 4).
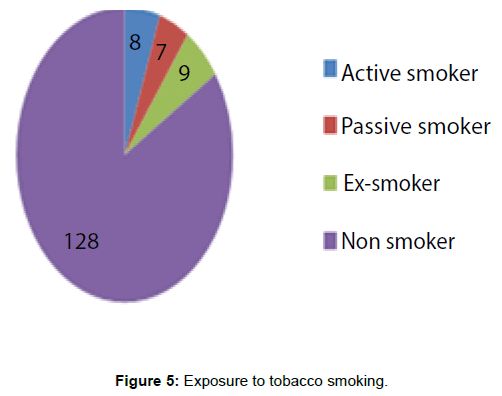
Exposure to tobacco smoking (active, passive or ex-smoker) was seen in 24 (15.78%) patients (Figure 5).
Seventy three percent of the total (111) was referred from surgical units after biopsy was performed. All 152 had undergone LN sampling; FNAC was perform ed in 16 patients while 150 patients underwent excision lymph node biopsy.
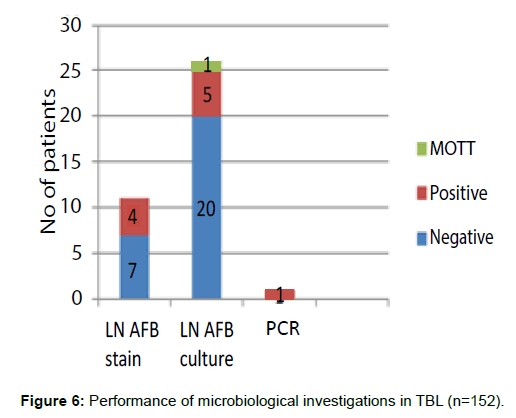
Only those patients who initially presented to the RDTU had microbiological tests performed. Four patients were positive for acid fast bacilli (AFB) staining out of 11 performed. Lymph node biopsy for culture was performed only in 26 patients. Culture confirmation for Mycobacterium tuberculosis (MTB) was achieved in five patients, while one was positive for Mycobacteria other than tuberculosis (MOTT). Five of them were sensitive to first line ATT (including MOTT) and one patient’s report showed resistance to first line drugs. LN for polymerase chain reaction (PCR) for MTB was performed only in one patient and it was positive (Figure 6).
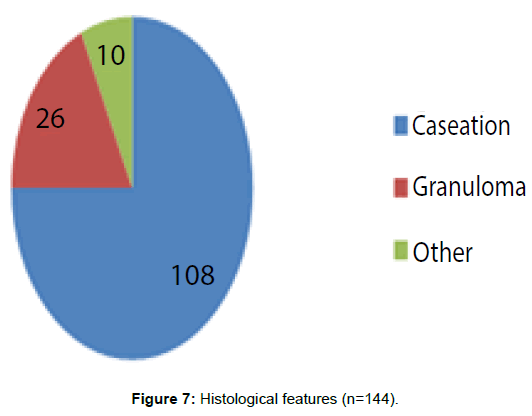
Out of the 152 patients 144 had positive histological evidence of TBL (Figure 7). Hundred and eight patients had caseation with or without other positive histological evidence. Twenty six patients had granulomas without caseation and 10 had other histological evidence suggestive of TBL such as isolated Langhan giant cells, multinucleated giant cells, histiocytes and epitheliod cells. All patients with microbiological evidence were found to have histological confirmation as well.
Eight patients did not show positive microbiological or histological evidence, but had supportive features of tuberculosis such as symptoms, raised ESR and strongly positive Mantoux. They were empirically treated with ATT according to the national TB guide lines (Figure 8).
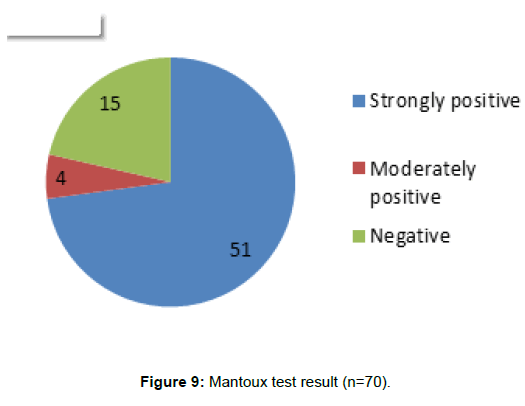
Mantoux test was performed in 70 (46%) patients and was strongly positive (more than 15 mm) in 51 (72.85%), moderately positive (10-14 mm) in 4 (2.63%) and negative (Less than 9 mm) in 15 (9.86%) (Figure 9).
The average pre-treatment ESR was 45.29 mm/h.
In the patients with inconclusive or borderline evidence, blood picture, CRP, HIV, VDRL, Toxoplasma serology and radiological tests (USS, CT, X-ray) were performed. However one of the patients were positive for HIV, VDRL or Toxoplasma.
All patients were commenced treatment initially with standard Category 1 (CAT1) treatment with 4HRZE + 2 HR fixed dose drug combinations (FDC).
CAT2=Category 2=2HRZES+1HRZE+5HRE
(4=4 months, 2=2 months, 1=1 month, 5=5 months)
(H-Isoniazid, R-Rifampicin, Z-Pyrazinamide, E-Ethambutol, S-Streptomycin).
Response of TBL was assessed according to improvement of symptoms, weight gain, reducing ESR and LN size improvement (Figure 10).
Of the patients with a definitive histological/ microbiological diagnosis of TBL (n=144), ninety five responded to standard 6 months course of CAT1 regimen. Forty nine did not show complete response and required further intervention. This included five patients responding to surgical excision after end of CAT1 regimen, thirteen patients converted to CAT2 (8 failures, 4 relapse, 1 default), eighteen patients responding to 7-9 month extended continuation regimen, one patient requiring 18 month regimen for atypical mycobacteria (clarithromycin, ethambutol, rifampicin) and one patient responded to both Anti TB Treatment (ATT) and antifungals (repeat biopsy positive for fungal species). Eleven patients had residual LN (<1 cm in diameter) at the end of 6-9 month CAT 1/extended regimen. At the time of discontinuation of treatment LN size was reduced and clinically, radiologically and biochemically those patients had improved. Further follow up revealed that they had not relapsed.
In the group without definitive diagnosis of TBL (n=8), four patients underwent change in the treatment since the diagnosis changed later (1 adenocarcinoma, 1 squamous carcinoma, 1 non-Hodgkin lymphoma (NHL), 1Hodgkin lymphoma (HL)). One patient had both TBL and coexisting NHL. One patient with cervical lymphadenopathy died at the end of second month, and the cause was unknown. Two patients who were treated based on clinical evidence improved with CAT1 treatment.
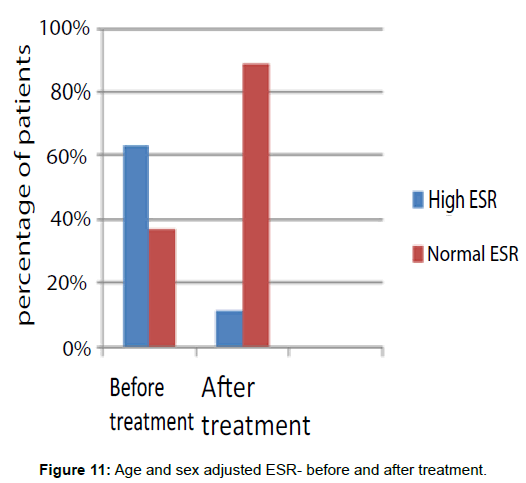
Age and sex adjusted ESR was high in 63% of the patients before treatment and after completion of treatment it remained elevated in 11% (Figure 11).
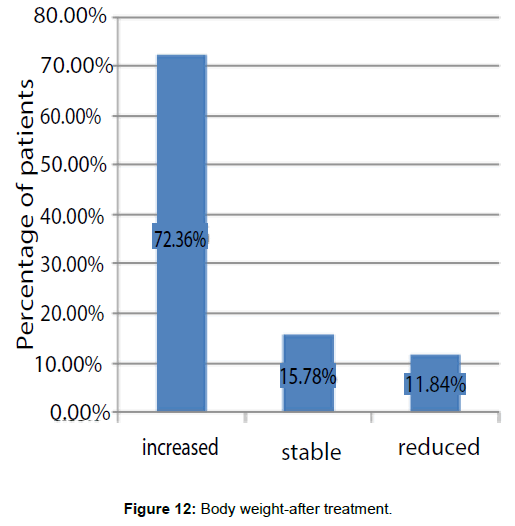
Body weight was assessed before and after treatment was completed. It was increased in 72.36% of patients after treatment was completed, reduced in 11.84% and stable in 15.78% (Figure 12).
After completion of treatment, persistent ESR elevation and loss of weight represented those patients who had not responded to treatment and or co-existing other medical problems.
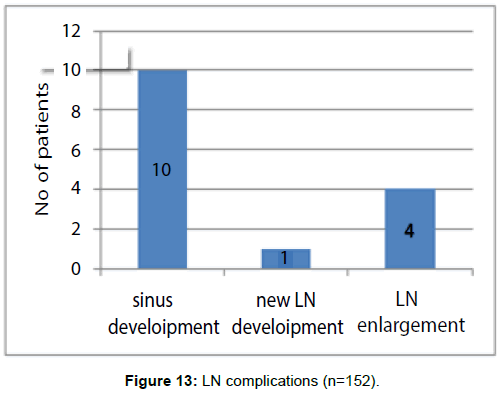
During the course of ATT sinus development seen in 10 patients, new LN development seen in 1 patient and LN enlargement seen in 4 patients (Figure 13).
Of the 144 patients who had started ATT according to definitive evidence, 22 had undergone repeat biopsy due to delayed resolution. All of them had evidence of TBL. Five had both evidence of TBL and co-existing disease (e.g. reactive follicular hyperplasia, parasitic granuloma, fungal infection, foreign body granuloma, non Hodgkins lymphoma).
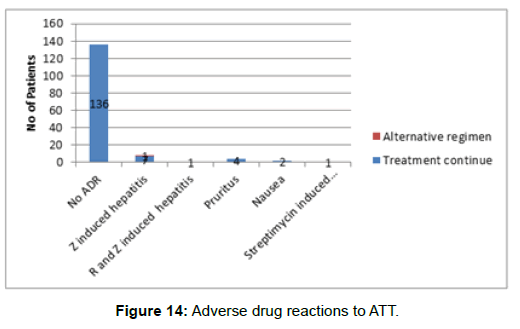
Out of 152 patients, 136 patients had no adverse drug reactions (ADR) to first line ATT drugs. Only 16 patients developed ADR. Eight patients developed pyrazinamide induced hepatitis and of them 1 patient failed desensitization and had to start an alternative regimen (replaced with levofloxacin). One patient developed hepatitis to both rifampicin and pyrazinamide and had to convert to an alternative regimen (2SHE+10HE). Streptomycin induced vestibular dysfunction developed in one patient and was replaced with levofloxacin. Four patients developed mild pruritus to ATT which responded to antihistamines and two patients developed nausea to ATT which responded to antiemetics (Figure 14).
Discussion
Tuberculosis continues to be a major public health problem throughout the world, particularly in developing countries. Nearly one-third of the global population (i.e., two billion people) is infected with Mycobacterium tuberculosis and is at risk of developing the disease. More than nine million people develop active tuberculosis every year and about two million die of the disease. It is the leading cause of death among adults due to a single infectious agent. The highest burden of the disease is in the most economically productive age group of our society (15-54 years). The rapid increase in the incidence of tuberculosis in the developing countries and its resurgence in the developed countries led the World Health Organization (WHO) to declare tuberculosis a global emergency in 199 [10].
Tuberculous lymphadenitis is among the most frequent presentations of EPTB. TB is responsible for 43% of peripheral lymphadenopathy in the developing world. In the United States, about 20% of patients with TB have extra pulmonary disease and lymphadenitis is a presenting symptom in about 30 to 40% of cases [1,3-5].
The human immunodeficiency virus (HIV) epidemic has been associated with an increase in the total incidence of TB and an increased proportion of miliary, disseminated and extra pulmonary TB cases including lymphadenitis [11].
The differential diagnosis of isolated peripheral lymphadenopathy is extensive and includes malignancy (e.g. Hodgkin lymphoma and non-Hodgkin lymphoma and other infections (e.g. Non-tuberculous mycobacteria (M. scrofulaceum, M. aviumcomplex, M. kansaii), cat scratch disease, fungal infection, sarcoidosis and bacterial adenitis). Kikuchi’s disease can cause a necrotizing lymphadenitis and mimic tuberculosis cervical lymphadenopathy [12]. The most likely alternative diagnoses depend on the clinical setting including the patient’s age, ethnic background, immune status and presenting clinical features.
Diagnosis of TB lymphadenitis is established by histopathological examination along with AFB smear and culture of lymph node material.
Molecular diagnostic techniques such as PCR have increased the sensitivity of FNA for TB diagnosis [13]. Culture permits susceptibility testing and therefore provides important therapeutic information even in the setting of positive PCR results. For circumstances in which the culture is negative or there is discrepancy between the clinical impression and excisional biopsy, PCR should be pursued if possible.
In our study we had 27.4% of EPTB cases and the incidence was compatible with international data. But TBL was found only in 16.29%. This may be due to low case detection. Also it may be useful to do further studies to find out the cause for low incidence of TBL in Central Sri Lanka.
In the United States, the rate of TB lymphadenitis is higher among females [1,4,14]. In our study too there were 56.57% of female patients with TBL.
In developed countries in contemporary series the median age has been approximately 40 years (range 1-88years) [15-17]. In our study the mean age was 35.97 years and the age range was 0.5-80 years which gave similar results to developed countries.
Cervical lymphadenopathy is the most common manifestation of TB lymphadenitis. In contemporary series it represents 63 to 77% of cases. In our study too isolated cervical lymphadenopathy were noted in 78.94% [15,17].
Other sites of TBL include the axillary, inguinal, mesenteric, mediastinal and intrammary lymphnodes. We identified involvement of axillary, submandibular, supraclavicular, inguinal, mesenteric and hilar lymphadenopathy [18-20].
The most common presentation is isolated chronic non-tender lymphadenopathy in a young adult without systemic symptoms [13,21]. All the patients with isolated lymphadenopathy in our study presented with swelling over the lymph node site, and constitutional symptoms were noted only in 40.78%.
Co-existing other medical problems and exposure to tobacco smoking were very low in prevalence and it represents that the isolated TBL occurs commonly in apparently healthy patients.
According to the data obtained the patients had a very low incidence of contact history. This leads to the conclusion that the infection would have most likely being acquired from the community. There was one patient with a positive contact history of EPTB which is unlikely to be the source for the infection for the particular patient.
Although most patients had disease at only one site, multiple nodes may involve at that site [14,21]. In our study multiple lymphatic sites were involved in 3.94% and multiple LN involvement detected in 45%.
BCG scar was positive in 90.16% which indicates that there is no relationship between occurrence of TBL and presence of BCG scar.
73% of the patients were referred from surgical team with the histology report after LN biopsy was performed, which indicates that in our setting most patients with LN enlargement were initially presented to surgical unit. In our study most patients (94.73%) had undergone LN biopsy and histology while microbiological (culture, smear, PCR) investigations were highly underutilized. In histology reports there were 75% of patients with caseation which indicates that in our setting most of the patients with caseation in the histology report should suspect tuberculosis as a first differential diagnosis.
Where there is no definitive evidence for TBL it is important to do Mantoux and monitor ESR and body weight. The Mantoux was very high in 72.85% with TBL. But with negative Mantoux test cannot exclude TBL since some patients with negative tests had TBL. ESR became normal in most of the patients (89%) who were responded to ATT. Body weight increased or remain stable in more than 88% of patients who responded to ATT.
Under clinical trial conditions, the behavior of LN tuberculosis was variable [1-3,22,23]. We felt that it would be interesting to see whether outcomes in routine practice mirrored those reported in clinical trials in Central Sri Lanka over last four years.
In our study 0.65% developed new lymph nodes during treatment, which is lower than the BTS trial findings (16%) [6]. Our sinus development rate (6.57%) was also low than the BTS trial findings (9%) [6] and sinuses healed with usual ATT chemotherapy without complications. Enlargement of lymphnodes during treatment were detected only in 2.63% of patients and there were not enough evidence to conclude that it was due to paradoxical reaction.
In our study 94.73% of patients had definitive evidence of TBL, all were confirmed with histology. All of them had responded to ATT management that had been carried out. None of them had relapses during our short course of follow up which indicates that for the diagnosis of TBL histological evidence is accepted. 65.97% of the patients responded to standard 6 months CAT1 regimen, which reflects that most with TBL were sensitive to CAT1, while few were responded to CAT2, extended continuation, surgical excision, and alternative regimen.
In our study 7.23% of the patients had some residual lymphadenopathy at the end of the treatment comparing favorably with the 23-41% rate reported in the trial setting [6].
Our study and the BTS trial differed in the follow up of patients, both in time and method. On discharge all the patients in our study were advised to return to the service if new lymph nodes developed, whereas in BTS trial all patients were routinely followed up.
11.84% of patients had to treat with extended continuation of treatment. In BTS trial setting [7] concluded that 6 months treatment showed similar efficacy to 9 month of treatment.
3.28% of patients had to undergo surgical excision which may be due to resistance to ATT chemotherapy. (scrofula-non tuberculous mycobacteria). Only one patient was treated with atypical mycobacteria regimen, which indicates the incidence was very low but should be kept in mind for non-responding TBL. Also co-existing other pathological diseases should be considered for non- responding TBL, since there were one patient with co-existing fungal infection and one with coexisting NHL.
5.26% of patients were started ATT according to clinical evidence. Out of them 37.5% responded to CAT1. During the course of treatment 4 patients had to change the diagnosis since biopsy came as a different pathological diagnosis. Therefore those patients who had started ATT with clinical grounds should monitor closely.
All the patients were treated with first line ATT except one who had to treat with atypical regimen (clarithromycin, rifampicin and ethambutol for 18 months). It indicates that the sensitivity to first line drugs were high. None of the patients had multidrug resistance (MDR). Although culture reports later came as 1 MOTT, and one patient was resistant to all first line drugs both of them responded to CAT1, indicating that those reports may be wrong. It concludes that clinical evidences are equally important as definitive evidence.
There were only 10.52% of patients who developed ADR to ATT. Out of them only 18.75% had given alternative regimen, which concludes that the ADR to ATT were very low incidence.
Conclusion
We noted that the microbiological studies were heavily underutilized among patients with TBL referred from other units to RDTU. However histology based diagnosis followed by standard ATT appeared safe and effective. Even though a trial of ATT may be warranted occasional on clinical grounds alone, these patients need close follow up to exclude co-existing/alternative pathologies. Also we noted that the adverse drug reactions were very low and response to first line ATT was high. There were no instances of drug resistance.
We suggest;
1. All suspected TBL patients should undergo excision biopsy and histology, which is available at base hospital levels.
2. All samples should also be sent for Mycobacterial microbiology and culture, as facilities are available at government sector.
3. Empirical ATT may need to be given occasionally without histological or microbiological evidence; however those patients should be closely observed at a specialist clinic.
References
- Danapat MC, Mishra BM, Dash SP, Kar PK (1990) Peripheral lymph node tuberculosis: a review of 80 cases. Br J Surg 77: 911.
- Narang P, Narang R (2005)Prevalence of tuberculous lymphadenitis in children in Wardha district, Maharashtra State, India. Int J Tuberc Lung Dis 9: 188.
- Centers for Disease Control (2006) Reported tuberculosis in the United States, 2006. Department of Health and Human Services, CDC, Atlanta, U.S.
- Rieder HL, Snider DE, Cauthen GM (1990) Extrapulmonary tuberculosis in the United States. Am Rev Respir Dis 141: 347.
- Peto HM, Pratt RH, Harrington TA (2009) Epidemiology of extra pulmonary tuberculosis in the United States. Clin Infect Dis 49: 1350-1357.
- British Thoracic Society Research Committee (1992) Six months versus nine-months chemotherapy for tuberculosis of lymph nodes: preliminary results, British Thoracic Society Research Committee. Respir Med 86: 15-19.
- Campbell IA, Ormerod LP, Friend JA, Jenkins PA, Prescott RJ (1993)Six months versus nine months chemotherapy for tuberculosis of lymph nodes: final results. Respir Med 87: 621-623.
- British Thoracic Society Resarch Committee (1985) Short course chemotherapy for tuberculosis of lymph nodes: a controlled trial. BMJ (Clin Res Ed) 290: 1106-1108.
- British Thoracic Society Research Committee (1988) Short-course chemotherapy for lymph node tuberculosis: final report at 5 years. Br J Dis Chest 82: 282-284.
- National programme for tuberculosis control and chest diseases (2005) General manual for tuberculosis control.
- Hill AR, Premkumar S, Brustein S (1991) Disseminated tuberculosis in the acquired immunodeficiency syndrome era. Am Rev Respir Dis 144: 1164.
- Kamath MP, Bhojwani K, Naik R (2006) Tuberculosis mimicking Kikuchi’s disease. Ear Nose Throat J 85: 126.
- Artenstein AW, Kim JH, Williams WJ, Chung RC (1995) Isolated peripheral tuberculous lymphadenitis in adults: current clinical and diagnostic issues. Clin Infect Dis 20: 876.
- Castro DJ, Hoover L, Csstro DJ, Zuckerbraun L (1985) Cervical mycobacterial lymphadenitis: Medical vs. surgical management. Arch Otolaryngol 111: 816.
- Geldmacher H, Taube C, Kroeger C (2002) Assessment of lymph node tuberculosis in northern Germany: a clinical review. Chest 121: 1177.
- Wark P, Goldberg H, Ferson M (1998) Mycobacterial lymphadenitis in eastern Sydney. Aust N Z J Med 28: 453.
- Mert A, Tabak F, Ozaras R (2002)Tuberculous lymphadenopathy in adults: A review of 35 cases. Acta Chir Belg 102: 118.
- Alvarez S, McCabe WR (1984) Extra pulmonary tuberculosis revisited: a review of experience at Boston City and other hospitals. Medicine (Baltimore) 63: 25.
- Shafer RW, Kim DS, Weiss JP, Quale JM (1991) Extra pulmonary tuberculosis in patients with human immunodeficiency virus infection. Medicine (Baltimore) 70: 384.
- Yilmaz F, Yagmur Y, Uzunlar AK (2000) Tuberculosis in an intramammary lymph node. Eur J Surg 166: 267.
- Shikhani AH, Hadi UM, Mufarrij AA, Zaytoun GM (1989) Mycobacterial cervical lymphadenitis. Ear Nose Throat J 68: 660-662.
- Fontanilla JM, Barnes A, Von Reyn CF (2011) Current diagnosis and management of peripheral tuberculous lymphadenitis. Clin Infect Dis 53: 555.
- Singh KK, Muralidhar M, Kumar A (1990) Comparison of in house polymerase chain reaction with conventional techniques for the detection of Mycobacterium tuberculosis DNA in granulomatous lymphadenopathy. J Laryngol Otol 104: 24.
Relevant Topics
- Antituberculous Drugs
- Bovine Tuberculosis
- Gastrointestinal Tuberculosis
- Laryngeal Tuberculosis
- Latent Tuberculosis
- Lymphadenitis
- Mantoux Tuberculin Test
- Meningeal Tuberculosis
- Miliary Tuberculosis
- Multiple Drug Therapy
- Mycobacterium Tuberculosis
- Non Pulmonary Tuberculosis
- Pulmonary Tuberculosis
- Tuberculin
- Tuberculosis
- Tuberculosis Cerebritis
- Tuberculous Meningitis
- Tuberculous Osteomyelitis
- Tuberculous Pericarditis
Recommended Journals
Article Tools
Article Usage
- Total views: 7709
- [From(publication date):
December-2016 - Aug 20, 2025] - Breakdown by view type
- HTML page views : 6663
- PDF downloads : 1046