Research Article Open Access
Effects of Brief Communication Skills Training Workshop on Improving Workers' Communication Behavior: A Randomized Controlled Trial
Somemura H1*, Sasaki N1, Horikoshi M2, Shinmei I2, Nakamura S1, Yamamoto M1, Kimura R1, Isojima M1, Takano T1and Tanaka K11Department of Occupational Mental Health, Graduate school of medical science, occupational mental health, Kitasato University, Japan
2Cognitive behavioral center, National Center of Neurology and Psychiatry, Japan
- *Corresponding Author:
- Hironori Somemura
MD, Department of Occupational Mental Health
Graduate School of Medical Sciences
Kitasato University, 1-15-1 Kitasato
Minami-ku, Sagamihara-shi
Kanagawa 252-0329, Japan
Tel: +81-3-3260-1146
E-mail: some811@leaf.ocn.ne.jp
Received date: October 21, 2015 Accepted date: November 16, 2015 Published date: November 21, 2015
Citation:Somemura H, Sasaki N, Horikoshi M, Shinmei I, Nakamura S, et al. (2015) Effects of Brief Communication Skills Training Workshop on Improving Workers' Communication Behavior: A Randomized Controlled Trial. J Community Med Health Educ 5:381. doi: 10.4172/2161-0711.1000381
Copyright: ©2015 Somemura H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objectives: To investigate the efficacy of communication skills training (CST) on improving communication behaviors of employees, we conducted a randomized controlled trial. Methods: We randomly divided 128 white-collar workers to either a CST intervention group (n=64) or a nonintervention control group (n=64). The three-hour CST session was conducted by an occupational physician. A Likert scale was used to assess four aspects of communication behavior: conversing so as not to put pressure on the subject, displaying empathy and support, helping the subject sort out problems, and thinking together to solve problems. Communication behavior scores were compared between the intervention and control groups three months after training. Results: Intention-to-treat analyses using mixed effect models showed a significant interaction between group and time (p=0.045) for all participants for "thinking together to solve problems," with an effect size (Cohen's d) of 0.37. For the other three items, although an improving trend was noted in the intervention group, no statistically significant interactions between group and time were observed. The sub-group analysis results for the four items' lower half baseline value for the items "helping the subject sort out problems" and "thinking together to solve problems" showed a significant interaction between group and time (p < 0.01) with effect sizes of 0.67 and 1.04, respectively. Conclusion: Brief CST for workers may be useful in improving communication behavior between individual employees. Given that CST improves and contributes to developing positive mental health, we hope that further intervention studies will be conducted in the future.
Keywords
Communication skills; Communication behaviors; Randomized controlled trial; Work place; Problem-solving
Introduction
Stimulating workplace communication between employees enhances mental health [1-3], discretion [4], and the well-being [5] of employees and has been associated with a reduction in depression and anxiety [6,7]. Further, poor workplace communication has been found to increase conflict in relationships between workers [8,9], whereas effective communication between workers can foster team spirit [10].
Several types of communication skills training (CST) for health occupations are being conducted at medical institutions to improve medical services and patient safety. Reviews and meta-analyses on the effect of these interventions have suggested that CST improves medical workers’ communication and attitudes, subsequently reducing patient psychological anxiety and anguish while increasing treatment adherence [11-17]. The success of CST intervention in medical establishments suggests that such training may also be effective in improving communication between workers in lay business organizations as well. However, thus far, few intervention studies have assessed the statistical significance of occupational CST in such environments. Here, we evaluated the effect of short-term CST intervention on communication behavior in workers at a private company.
Methods
Participants and study design
The participants were employees in the research and development sector at a private enterprise company in Japan. The purpose of the research was explained via a company e-mail to all workers. Workers were assured that participation was wholly voluntary and that declining to participate would not invoke any sort of punishment. No exclusion criteria were provided, since the company’s health and safety committee wanted all staff to be eligible. The eligible workers were registered as study participants with the Kitasato Clinical Research Center and randomly assigned to one of two groups: an intervention group, which received the CST; and a control group, which received no training.
For ethical reasons, after the experiment was complete, the control group received the same training as the intervention group. The study was conducted with approval from the health and safety committee of the participants’ company and the Kitasato University ethics committee.
Intervention
The intervention group received CST from an occupational physician who had undergone 10 hours of training on delivering CST by the expert of communication skills training prior to the experiment. The training consisted of one 3-hour session conducted during working hours, and intervention group participants were asked to attend one of the two equivalent training sessions (August and September 2014). The CST session materials were based on the Communication Skills Training Guide developed by National Center for Cognitive Behavior Therapy and Research, National Center of Neurology and Psychiatry [18]. In addition to goals of building good relationships with the subjects, the communication training also aimed to provide support for problem solving using analytical questioning (Socratic method). The training content structure is shown in Table 1.
| Total (n=128) | Intervention (n=64) | Control (n=64) | P-value* | |
|---|---|---|---|---|
| Sex (male, n [%]) | 123 (96.1) | 61 (95.3) | 62 (96.9) | 0.64 |
| Age (years, mean [SD]) | 41.1 (8.91) | 42.4 (8.51) | 40.7 (9.28) | 0.29 |
| Occupation, n (%) | ||||
| Research and development | 107 (83.6) | 53 (82.8) | 54 (84.4) | 0.97 |
| Management | 18 (14.1) | 8 (12.5) | 10 (15.6) | |
| Others | 2 (1.6) | 2 (3.2) | 0 (0.0) | |
| Missing | 1 (0.8) | 1 (1.6) | _ | |
| Years employed in current department, n (%) | ||||
| <1 | 5 (3.9) | 3 (4.7) | 2 (3.1) | 0.96 |
| 1 ≤ x < 3 | 14 (10.9) | 6 (9.4) | 8 (12.5) | |
| 3 ≤ x < 5 | 28 (21.9) | 14 (21.9) | 14 (21.9) | |
| ≥5 | 80 (62.5) | 40 (62.5) | 40 (62.5) | |
| Missing | 1 (0.8) | 1 (1.6) | ||
| Weekly [check] hours of overtime, n (%) | ||||
| < 20 | 46 (35.9) | 20 (31.3) | 26 (40.6) | 0.35 |
| 20 ≤ x < 45 | 61 (47.7) | 33 (51.6) | 28 (43.8) | |
| 45 ≤ x < 80 | 18 (14.1) | 8 (12.5) | 10 (15.6) | |
| ≥80 | 2 (1.6) | 2 (3.1) | 0 (0.0) | |
| Missing | 1 (0.8) | 1 (1.6) | ||
| Nightly hours of sleep, n (%) | ||||
| <4 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.06 |
| 4 ≤ x < 5 | 12 (9.4) | 6 (9.4) | 6 (9.4) | |
| 5 ≤ x < 6 | 46 (35.9) | 18 (28.1) | 28 (43.8) | |
| 6 ≤ x < 7 | 50 (39.1) | 29 (40.6) | 24 (37.5) | |
| 7 ≤ x < 8 | 14 (10.9) | 9 (14.1) | 5 (7.8) | |
| ≥8 | 5 (3.9) | 4 (6.3) | 1 (1.6) | |
| Missing | 1 (0.8) | 1 (1.6) | ||
| K6 score, mean (SD) | 4.5 (4.5) | 4.4 (4.1) | 4.5 (4.8) | 0.94 |
| Conversing so as not to put presure on the subject, mean (SD) | 6.8 (1.9) | 6.9 (1.9) | 6.6 (1.9) | 0.31 |
| Displaying empathy and support, mean (SD) | 6.7 (1.8) | 6.8 (1.7) | 6.6 (1.9) | 0.58 |
| Helping the subject sort out problems, mean (SD) | 6.2 (1.9) | 6.2 (2.0) | 6.1 (1.8) | 0.74 |
| Thinking together to solve problems, mean (SD) | 6.7 (1.9) | 6.7 (1.9) | 6.8 (1.9) | 0.92 |
| *at test for continuous variables and Fisher’s exact test for categorical variables were used. | ||||
Table 1: Structure of communication skills training.
Outcomes
An original self-report questionnaire was used to examine communication skills proficiency, featuring four items: "I converse in a manner so as not to put pressure on the person with whom I am speaking (conversing so as not to upset the subject)," "I display empathy and support when having a conversation (displaying empathy and support)," "I help the person I am speaking with sort out their problems (helping the subject sort out problems)," "I think together with the person I am speaking with to solve problems (thinking together to solve problems)."These 4 items were measured using an 11- point Likert scale of responses ranging from 0 to 10, with a higher number representing greater affirmation of the item.
Basic attributes of participants
Information on basic participant attributes, namely age, gender, occupation, years of employment at the company, hours of overtime per month, nightly sleep duration, and mental health status, was obtained. Mental health status was evaluated using the Japanese version of K6 [19,20]. Each of the 6 items had a possible score of 0 to 4 (possible total score, 0-24), with a higher score indicating more severe mental state.
Randomization
The Kitasato Clinical Research Center randomly assigned participants to either the intervention group or the control group. Although the data analyses were blind, the participants were aware of their group assignment to due to the nature of intervention.
Statistical analysis
The data analysis outcome loss percentage was 4.7%. To satisfy the intention-to-treat (ITT) principle, which states that all participant analyses should be conducted as they are allocated, multiple imputations (MI) [21] were performed, with data assumed to be missing at random. In a previous meta-analysis [12] of CST among medical workers, the effect size for communication behavior (Cohen’s d) was 0.54. In the present study, the CST effect was assumed to be moderate (Cohen’s d=0.5), α-error was set at 0.05, β-error was set at 0.20, and the sample size was 64 people per group.
Linear mixed models with group, time, and interactions between group and time were used as the fixed effects, and participants were randomized for the random effect in order to examine the effect of CST on the workers’ communication skills. To evaluate the significance of the interaction between group and time, the type III Wald test was applied. The outcome data for both intervention and control groups from the follow-up test three months after the experiment was used to calculate the intervention effect size. Further, as an adjustment factor, the baseline outcome value was added to the model. For the sub-group analysis, the baseline outcome value for the lower half of the workers was performed in the same manner as described above. In the baseline comparison for the intervention and control groups, a t test for continuous variables and Fisher’s exact test for categorical variables were used. Statistical significance was set at α=0.05, and a two-sided test was conducted. IBM SPSS Statistics 22 and IBM SPSS Missing Values 22 (IBM Corp, Armonk, NY, USA) were used for statistical analyses.
Results
Participant flow
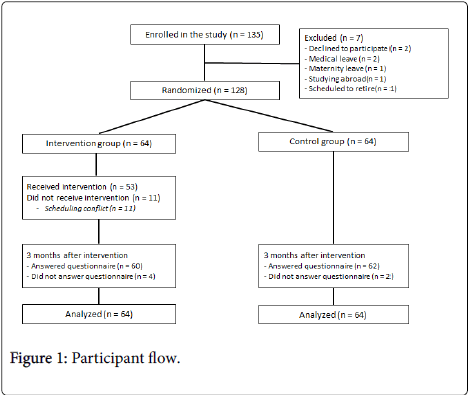
The participant flow is shown in Figure 1. Participation consent was received from 128 of the 135 workers contacted; of the 7 who did not participate, 2 refused to participate, 2 were on medical leave, 1 was on maternity leave, 1 was studying abroad, and 1 was scheduled to retire. The final 128 participants were the randomly assigned to either an intervention group or a control group (n=64 each). Of the 64 people in the intervention group, 11 were unable to participate due to scheduling conflicts, and 53 (84%) ultimately received the CST intervention. In total, 60 of the 64 participants in the intervention group (94%) and 62 of the 64 participants in the control group (97%) responded to the questionnaire distributed three months after the intervention.
Participant characteristics
Participant baseline attributes are shown in Table 2. Subjects were 123 men (61 in the intervention group, 62 in the control group) and 5 women (3 in the intervention group, 2 in the control group) with a mean overall age of 41.6 years. (intervention group, 42.4 years; control group, 40.7 years). No significant differences were noted between the two groups in any of the characteristics assessed nor in baseline outcome values.
| Mean Scores (SE)* | Group × Time interaction** | Effect size | ||
|---|---|---|---|---|
| Intervention Group (n=64) | Control Group (n=64) | (95% CI)* | ||
| Conversing so as not to put pressure on the subject | 6.7 (0.2) | 6.6 (0.2) | 0.9 | 0.07 (−0.29-0.42) |
| Displaying empathy and support | 6.8 (0.2) | 6.7 (0.2) | 0.73 | 0.11 (−0.25-0.46) |
| Helping the subject sort out problems | 6.3 (0.2) | 6.1 (0.2) | 0.57 | 0.14 (−0.21-0.50) |
| Thinking together to solve problems | 7.0 (0.2) | 6.5 (0.2) | 0.045 | 0.37 (0.01-0.72) |
Table 2: Baseline characteristics in intervention and control groups.
ITT analysis
ITT findings for all subjects are shown in Table 3. For the item "thinking together to solve problems," a significant interaction was observed between group and time (F1, 244.0=4.06, P=0.045). Three months after the intervention, the score of "thinking together to solve problems" was 7.00 for the intervention group and 6.51 for the control group, and a significant difference was observed for both groups with effect size (Cohen’s d) of 0.37. For the remaining three items, although improving trends were evident, no statistically significant interactions for group and time were observed.
| Mean Scores (SE)* | Group × Time interaction** | Effect size | ||
|---|---|---|---|---|
| Intervention Group (n=64) | Control Group (n=64) | (95% CI)* | ||
| Conversing so as not to put pressure on the subject | 6.7 (0.2) | 6.6 (0.2) | 0.9 | 0.07 (−0.29-0.42) |
| Displaying empathy and support | 6.8 (0.2) | 6.7 (0.2) | 0.73 | 0.11 (−0.25-0.46) |
| Helping the subject sort out problems | 6.3 (0.2) | 6.1 (0.2) | 0.57 | 0.14 (−0.21-0.50) |
| Thinking together to solve problems | 7.0 (0.2) | 6.5 (0.2) | 0.045 | 0.37 (0.01-0.72) |
Table 3: Comparison of intervention and control groups at three-month follow-up (entire analysis).
Table 4 shows the lower half group sub-analysis results for the baseline values for the four items. For the item, "helping the subject sort out their problems," the group and time interaction was significant (F167.3=7.64, P=0.007), with an effect size of 0.67. In addition, for the item, "thinking together to solve problem," a significant interaction was found between the group and time interaction was significant (F1, 43.4=12.93, P=0.001), with an effect size of 1.04. For the remaining two items, the sub-analysis results showed a large effect size compared to the entire analysis; however, no statistically significant differences were observed for group and time.
| Mean Scores (SE)* | Group × Time interaction** | Effect size | ||
|---|---|---|---|---|
| Intervention Group | Control Group | (95% CI)* | ||
| Conversing so as not to put pressure on the subject (≤6 points) | 6.1 (0.3) (n=24) | 5.3 (0.3) (n=27) | 0.15 | 0.49 (−0.07-1.05) |
| Displaying empathy and support (≤6 points) | 5.8 (0.3) (n=23) | 5.3 (0.3) (n=23) | 0.43 | 0.38 (−0.20-0.96) |
| Helping the subject sort out problems (≤6 points) | 6.0 (0.2) (n=32) | 5.2 (0.2) (n=36) | 0.007 | 0.67 (0.18-1.16) |
| Thinking together to solve problems (≤6 points) | 6.4 (0.3) (n=21) | 5.1 (0.3) (n=24) | 0.001 | 1.04 (0.41-1.66) |
Table 4: Comparison of intervention and control groups at three-month follow-up (two-quantile analysis).
Discussion
In the present study, communication behavior in workers such as “thinking together to solve problems” was significantly improved with the CST. This CST program emphasized that, when seeking to solve problems, the listener should not force his opinion on the partner but provide guidance so that the partner can find their own solutions to their problems and issues. This is reflected in the study results. Further, substantial improvement was seen following CST among individuals who had low initial baseline self-evaluation scores in the intervention group for the item "helping the subject sort out problems" in addition to "thinking together to solve problems."
Because the subjects in this study were company workers, the intervention program needed to require very little time to complete, so as not to disrupt work schedules. In prior studies at medical institutions, most CST programs lasted several days, with even the shortest program lasting six hours [13-17,22-30]. The relatively short 3-hour duration of the CST program approved by the occupational physician markedly reduced the time cost to workers and the economic burden to the business. This short duration and the significant positive effect of CST noted in the present study suggest that such a program may be appropriate and effective in many workplaces.
The CST effects observed in our study were not as significant as those reported in previous intervention studies for medical institutions. A meta-analysis [12] of research based on ITT analyses indicated a moderate effect (d=0.54) for communication behavior among medical personnel following CST intervention. In daily clinical situations, medical personnel commonly discuss diagnoses, treatment selection, and other such serious matters with patients and their family members. Improving communication skills in medical workers has been shown not only to reduce the anxiety and psychological anguish suffered by patients [13-15] but also to increase rates of adherence to treatment [16,17].
Therefore, they are well aware that high-level communication skills are essential for effective on-site work in medical institutions. This can be the reason CST is more effective in medical workers than in workers in other occupational fields.
Given that the follow-up test was conducted just three months after the intervention, we were unable to verify the presence of a long-term effect. In previous CST intervention research in the medical field, follow-up evaluations were conducted anywhere from three months [15,26,27] to one year [24,29] after intervention. However, in studies with follow-up tests conducted more than one year after the intervention, the effect of CST intervention had a tendency to be small. While we did not evaluate how long the CST effect in the present study lasted, the possibility of attenuation over time cannot be discounted, and some manner of post-training support (such as sending encouraging emails or providing supplementary information) may be valuable in achieving a booster effect.
Observational workplace studies have shown that good superior subordinate communication enhances mental health [1-3], discretion [4], and the well-being [5] of employees and is also associated with a reduction in depression and anxiety [6,7]. In the present study, because of the small number of superiors, participants were not divided into groups by work designations, such as supervisors and subordinates; however, if such division had been possible, a different effect may have been observed.
Communication skills improvement due to CST intervention for medical workers has been shown to increase self-efficacy and reduce stress, depression, and anxiety [31-33]. A cross-sectional study of general workers in a workplace [34] showed that the promotion of communication was negatively correlated with psychological distress in workers. Future CST studies should examine whether or not improvements in positive mental health can promote improvements in areas such as work performance and work motivation.
Several limitations to the present study warrant mention. First, it was difficult to decide on an effective sample size, as no previous studies have examined the effectiveness of CST interventions in a nonmedical workplace. Our study may therefore lack sufficient statistical weight for the conclusions to be sound. Second, sampling bias exists, as most subjects were men working in research and development. Future studies should try to diversify the examined population. Third, our intervention was held during a relatively busy period for the company; consequently, 11 of the 64 participants (17.2%) in the intervention group were unable to participate in the training due to scheduling conflicts. Fourth, given that all participants worked at the same company, subjects in the intervention group may have disclosed details about the training program to those in the control group, resulting in contamination. Finally, because the questionnaire used here was originally developed for our study, the reliability and validity were not verified. Further, the questionnaire was self-administered, and no objective evaluation of communication behaviors was conducted.
Conclusion
Although the CST program used in this study was only three hours long, a significant improvement in communication behaviors was observed. In addition to improving the communication skills of workers, CST could also contribute to positive mental health. We hope that further CST-related invention studies will be conducted in the future, with more diverse and larger populations.
References
- Mineyama S, Tsutsumi A, Takao S, Nishiuti K, Kawakami N (2007) Supervisors' attitudes and skills for active listening with regard to working conditions and psychological stress reactions among subordinate workers. J Occup Health 49: 81-87.
- Ikegami K, Tagawa Y, Mafune K, Hiro H, Nagata S (2008) The effectiveness of the mental health training including active listening for managers. Sangyo EiseigakuZasshi 50: 120-127.
- Ikegami K, Tahara H, Yamada T, Mafune K, Hiro H, et al. (2010) The effects of a mental health training program for manufacturing company managers. J UOEH 32: 141-153.
- Theorell T, Emdad R, Arnetz B, Weingarten A (2001) Employee Effects of an Educational Program for Managers at an Insurance Company. Psychosomatic Medicine 63: 724-733.
- Jacobs C, Pfaff H, Lehner B, Driller E, Nitzsche A, et al. (2013) The Influence of Transformational Leadership on Employee Well-Being: Results From a Survey of Companies in the Information and Communication Technology Sector in Germany. J Occup Environ Med 55: 772-778.
- Shimizu T, Takahashi H, Mizoue T, Kubota S, Mishima N, et al. (2003) Relationships among self-efficacy, communication, self-management skills and mental health of employees at a japanese workplace. J UOEH 25: 261-270.
- Theorell T, Nyberg A, Leineweber C, Magnusson Hanson LL, Oxenstierna G, et al. (2012) Non-listening and self centered leadership--relationships to socioeconomic conditions and employee mental health. PLoS One 7: e44119.
- Pondy LR (1967) Organizational Conflict: Concepts and Models. Administrative Science Quarterly 12: 296-320.
- Pavlakis A, Kaitelidou D, Theodorou M, Galanis P, Sourtzi P, et al. (2011) Conflict management in public hospitals: the Cyprus case. International Nursing Review 58: 242-248.
- Aberese-Ako M, Agyepong I, Gerrits T, Dijk H (2015) I used to fight with them but now I have stopped!': conflict and doctor-nurse-anaesthetists' motivation in maternal and neonatal care provision in a specialist referral hospital. PLoS One 10: e0135129.
- McGilton KS, Boscart V, Fox M, Sidani S, Rochon E, et al. (2009) A systematic review of the effectiveness of communication interventions for health care providers caring for patients in residential care settings. Worldviews Evid Based Nurs6(3):149-59.
- Barth J, Lannen P (2011) Efficacy of communication skills training courses in oncology: a systematic review and meta-analysis. Annals of Oncology 22: 1030-1040.
- Razavi D, Delvaux N, Marchal S, Durieux JF, Farvacques C, et al. (2002) Does training increase the use of more emotionally laden words by nurses when talking with cancer patients? A randomised study. Br J Cancer 87: 1-7.
- Razavi D, Merckaert I, Marchal S, Libert Y, Conradt S, et al. (2003) How to optimize physicians' communication skills in cancer care: results of a randomized study assessing the usefulness of posttraining consolidation workshops. J ClinOncol 21: 3141-3149.
- Wilkinson S, Perry R, Blanchard K, Linsell L (2008) Effectiveness of a three-day communication skills course in changing nurses’ communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med 22: 365-375.
- Stewart M, Brown JB, Hammerton J, Donner A, Gavin A, et al. (2007) Improving communication between doctors and breast cancer patients. Ann Fam Med 5: 387-394.
- Nehls W, Gabrijel S, Kiss A, Delis S, Black NB, et al. (2014) Communication skills training significantly improves lung cancer patient’s understanding. J Palliative Care Med 4: 182.
- Horikoshi M, Tajima M (2014) The ABCs of communication skills. National Center of Neurology and Psychiatry, Tokyo.
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, et al. (2002) Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 32: 959-976.
- Furukawa TA, Kawakami N, Saitoh M, Ono Y, Nakane Y, et al. (2008) The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int J Methods Psychiatric Res 17: 152-158.
- Donders AR, van der Heijden GJ, Stijnen T, Moons KG (2006) Review: a gentle introduction to imputation of missing values. J ClinEpidemiol 59: 1087-1091.
- Hainsworth DS (1996) The effect of death education on attitudes of hospital nurses toward care of the dying. OncolNurs Forum 23: 963-967.
- Alexander SC, Keitz SA, Sloane R, Tulsky JA (2006) A controlled trial of a short course to Improve residents’ communication with pacientes at the end of life. Acad Med 81: 1008-1012.
- Butow P, Cockburn J, Girgis A, Bowman D, Schofield P, et al. (2008) Increasing oncologists’ skills in eliciting and responding to emotional cues: evaluation of a communication skills training program. Psychooncology 17: 209-218.
- Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, et al. (2002) Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet 359: 650-656.
- Heaven C, Clegg J, Maguire P (2006) Transfer of communication skills training from workshop to workplace: the impact of clinical supervision. Patient EducCouns 60: 313-325.
- Jenkins V, Fallowfield L (2002) Can communication skills training alter physicians' beliefs and behavior in clinics? J ClinOncol 20: 765-769.
- Kruse J, Schmitz N, Woller W, Clar B, Meyer E, et al. (2003) Effects of a psychosocial education programme to improve doctor-patient interaction with cancer patients. Z Psychosom Med Psychother 49: 232-245.
- Razavi D, Delvaux N, Farvacques C, Robaye E (1988) Immediate effectiveness of brief psychological training for health professionals dealing with terminally ill cancer patients: a controlled study. SocSci Med 27: 369-375.
- Razavi D, Delvaux N, Marchal S, Bredart A, Farvacques C, et al. (1993) The effects of a 24-h psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. Eur J Cancer 29A: 1858-1863.
- Yutani M, Takahashi M, Miyaoka H (2011) Changes in communication skills of clinical residents through psychiatric training, Psychiatry ClinNeurosci65(6):561-6.
- Yamagishi M, Toshio K, Takemasa K, Nagami M, Shimazu A, et al. (2007) Effect of web-based assertion training for stress management of Japanese nurses. J NursManag15(6):603-7.
- Delvaux N, Razavi D, Marchal S, Bredart A, Farvaques C, et al. (2004) Effects of a 105 hours psychological training program on attitudes, communication skills and occupational stress in oncology: a randomized study. Br J Cancer90(1):106-14.
- Eguchi H, Tsuda Y, Tsukahara T, Washizuka S, Kawakami N, et al. (2012) The Effects of Workplace Occupational Mental Health and Related Activities on Psychological Distress Among Workers: A Multilevel Cross-Sectional Analysis. J Occup Environ Med 54: 939-947.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12329
- [From(publication date):
December-2015 - Aug 31, 2025] - Breakdown by view type
- HTML page views : 11312
- PDF downloads : 1017