Research Article Open Access
Emergency Department Intervention Program for Enhancing Choice at the End of Life: A Quality Improvement Project at a Comprehensive Cancer Center
Maria T Cruz-Carreras1*, Patrick Chaftari1, Carmen Gonzalez1, Rowena Enojo2 and Jayne Viets-Upchurch1
1Department of Emergency Medicine, The University of Texas MD Anderson Cancer Center, Houston, Texas
2Department of Emergency Center, The University of Texas MD Anderson Cancer Center, Houston, Texas
- *Corresponding Author:
- Maria T. Cruz-Carreras
Department of Emergency Medicine
The University of Texas MD Anderson Cancer Center, Houston, Texas
Tel: (713) 745-4516
Email: mcruz3@mdanderson.org
Received date: January 26, 2017; Accepted date: February 22, 2017; Published date: February 27, 2017
Citation: Cruz-Carreras MT, Chaftari P, Gonzalez C, Enojo R, Viets-Upchurch J (2017) Emergency Department Intervention Program for Enhancing Choice at the End of Life: A Quality Improvement Project at a Comprehensive Cancer Center. J Palliat Care Med 7:298. doi:10.4172/2165-7386.1000298
Copyright: © 2017 Maria, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Advance care planning (ACP) for end-of-life care is especially important for individuals with terminal illnesses such as advanced cancer. It ensures that patients’ wishes are honored and alleviates the decisionmaking burden on family members and medical providers. It reduces unnecessary medical costs, and prevents waste of valuable resources. We proposed a quality improvement project to improve documentation of advanced care directives in the Emergency Department (ED) of a tertiary cancer center.
Methods: We developed a pocket card to help emergency physicians screen patients in need of ACP. The goal was to assist ED staff in initiating conversations about end-of-life issues, and encourage patients and their caregivers to get involved in decisions about their medical treatment.
Intervention: The project was implemented in a Plan-Do-Study-Act design. Baseline data was collected from the medical records of all patients visiting the ED on seven consecutive days prior to the distribution of the pocket card tool. After the launch of the intervention, the charts of all patients visiting the emergency center were reviewed for documentation of advanced care planning. Metrics polled included presence of a health care power of attorney and determination of code status, specifically the do-not-resuscitate (DNR) status.
Results: 429 patients who visited the ED seven consecutive days prior to institution of the screening tool. Of these, we found that 66 (15.4%) had indicated their do-not-resuscitate (DNR) status in their charts, and 82 (19.1%) had a health care power of attorney. Post launch of the intervention, 391 patients visited the ED over seven consecutive days. Of these, 125 (32.0%) indicated their DNR status in their charts before leaving the ED, and 95 (24.3%) had a health care power of attorney. After implementation of our screening tool, there was a 107.8% increase in documentation of DNR status and a 76% increase in patients with a health care power of attorney.
Conclusions: In this quality improvement project, a straightforward, low cost intervention was successfully implemented to improve documentation of patients’ ACP goals.
Keywords
End of life; Cancer; Emergency department; DNR; Medical power of attorney; Advanced directives; Palliative
What this Paper Adds
Section 1: What is already known on this subject
ACP is an essential tool employed to document and honor patient wishes with regard to health care that is particularly valuable as the patient approaches end of life care.
Section 2: What this study adds
This pilot project employed a low cost intervention (pocket cards) and structured documentation to improve ACP rates and documentation.
Introduction
Problem description
Advance care planning (ACP) allows patients to make decisions about the kind of care they would like to receive. It is particularly helpful in the setting of patients nearing the end of life owing to terminal disease. The process involves the patient learning about available medical treatments and making decisions about which therapies they elect to receive or forego. ACP allows these wishes to be clearly communicated to family and healthcare professionals. Should a patient become unable to speak for themselves, ACP provides a platform upon which the patient’s medical proxy and health care team can base decisions made on the patient’s behalf [1,2].
Documentation of ACP may be made in the form of advance directives. In the United States, these documents most commonly include a living will, which provides directives regarding treatment, and a durable power of attorney for health care, which appoints a surrogate who can make medical decisions on an individual’s behalf. During ACP, decisions about specific treatments can also be documented, the most common being a decision to withhold cardiopulmonary resuscitation made by signing a do not resuscitate (DNR) order.
Available knowledge
Emergency department physicians and other medical providers should consider discussing end-of-life issues-including out-of-hospital DNR orders, with cancer patients nearing the end of life [3]. Patients who have made their end-of-life care wishes known through ACP spend fewer days in the hospital in the last year of life and have reduced hospital costs [4,5]. Among patients who prefer to die at home, a group which includes many patients with advanced cancer [6], those with a DNR order are less likely to die in the hospital.
Rationale
Cancer patients would ideally address ACP decisions with their primary oncologist outside the setting of the ED. Unfortunately, for many patients, this does not occur in the outpatient setting. We set out to equip ED clinician with a tool to identify patients in need of ACP and to initiate meaningful conversations with the patient and family regarding their healthcare choices.
Specific aims
In this study, we implemented the use of a screening tool to identify patients who would most benefit from ACP. We aimed for a 20% increase in the number of patients at The University of Texas MD Anderson Cancer Center who were dispositioned from the ED (whether it be to be discharged home or to be admitted to the hospital) with advance directive documentation in their medical records. We also focused on identifying the barriers preventing emergency physicians from addressing end-of-life issues with patients at the ED.
Methods
Context
Our ED is a 43 bed unit with an annual volume of 26,000 patients. The department is integral to the functioning of the cancer center. Over 40% of inpatient encounters are initiated by the emergency department. The majority of these have established care with our facility for treatment of their cancer. In addition to the treating ED clinician, the care team for established patients includes their primary oncologist, nursing, case management, social work and chaplaincy (if desired).
Intervention
Utilizing a Plan-Do-Study-Act (PDSA) methodology, our project consisted of three phases [7]. A screening tool was developed to identify patients in need of proactive advance care planning. Baseline data was collected over a one week period in the pre-pilot phase. The pilot phase included the distribution of the screening tool and physician education in its use. The post-pilot phase examined the results of the intervention with data being collected over another one week period.
Pre-pilot phase
We reviewed the medical records of all patients discharged from the ED over a period of seven consecutive days before the screening tool was instituted. Of those patients, we recorded how many had documentation of advance directives (medical power of attorney, living will, and/or DNR order).
Over a period of seven consecutive days prior to institution of the screening tool, 429 patients visited the ED at MD Anderson. Of those, we found that 66 patients (15.4%) had indicated their DNR status in their charts, and 82 patients (19.1%) had a health care power of attorney.
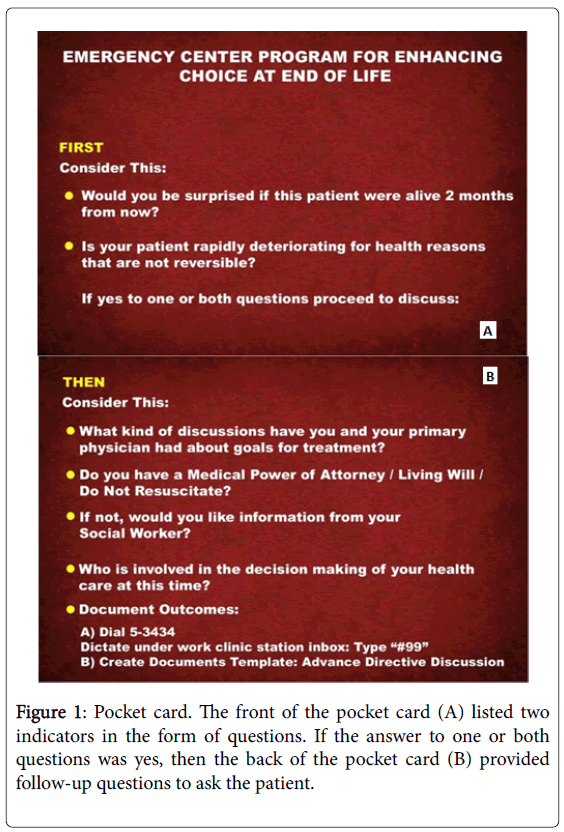
A screening tool was developed in the form of a pocket card (Figure 1). The front of the card asked the providers to consider the two questions:
1) "Is your patient rapidly deteriorating for health reasons that are not reversible?" We hypothesized that patients who have experienced an acute deterioration may not have had the opportunity or inclination to discuss ACP with their primary oncologist.
2) “Would you be surprised if this patient were alive two months from now?" This is variant of the typical “surprises question.” [8]. The two month endpoint was chosen to underscore the acute nature of the ED patient population.
An affirmative answer to one or both of these questions prompted the provider to consider initiating a discussion regarding ACP. Prior to any discussion, the patient’s chart would be checked for advance directives or evidence of end-of-life care preferences. The patient’s primary oncologist (or the oncologist on call) would be contacted to assist in establishing the overall prognosis and obtain feedback from the oncologist as to his/her opinion regarding the appropriateness of DNR status.
If an emergency medicine physician determined that a conversation regarding end-of-life issues was necessary, the conversation was held with the patient and family members while the patient was still in the ED. The back of the pocket card provided recommendations or scripted ideas on how to initiate the conversation. Among them, physicians were to ask the patient and family about prior discussions of goals of care and whether there was already a health care power of attorney, living will, or DNR documents. Before the patient was discharged home or admitted to the inpatient floor, social workers and ED registered nurses reinforced these end-of-life conversations.
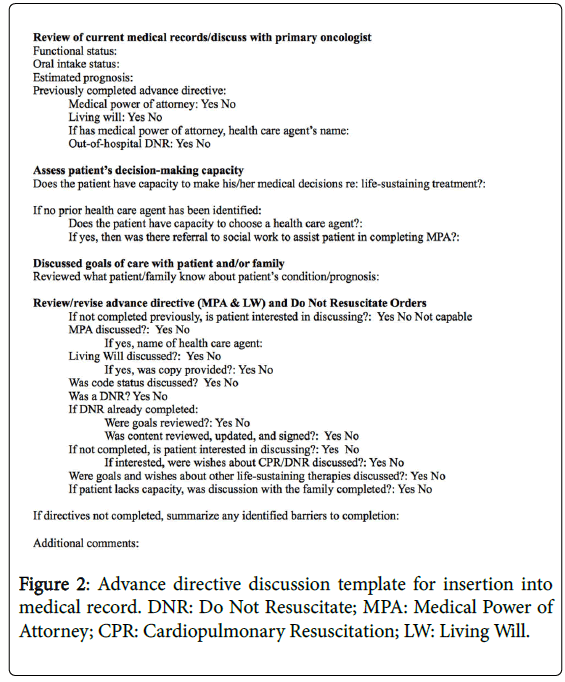
An Advance Directive Discussion Template (Figure 2) was used to record and document in the medical record the patients’ status, prognosis, and decision-making capability. If advance directives could not be completed or were difficult to obtain for any reason, the reasons for this could also be documented in the Discussion Template.
Pilot phase
The proposed intervention was reviewed and physician buy in was obtained over the course of several faculty meetings. The pocket card screening tool was distributed to the ED clinical faculty and implemented for a one month period. Physicians were educated in the use of the screening tool and all questions were answered. Likewise, social workers and case managers actively rounded on patients to explore whether they may meet screening criteria. Figure 3 is a patient flow map that for the intervention. Red lines and text are representative of changes to the previously existing patient flow model.
Post-pilot phase
During seven consecutive days, one month after the screening tool was instituted, 391 patients visited the ED. Of those, 125 patients (32.0%) indicated their DNR status in their charts before leaving the ED, and 95 patients (24.3%) had a health care power of attorney in their charts before leaving the ED.
Ethical considerations
This project was approved by our institution’s Quality Board. We report our findings here according to SQUIRE 2.0 guidelines which provides a framework for reporting new knowledge about health care improvement [9].
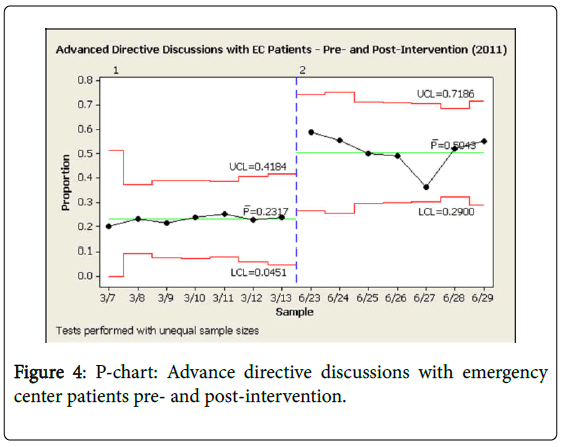
Results
Comparing the number of patients who were discharged from the ED with documentation of DNR status and health care power of attorney before and after implementation of the screening tool, there was a 107.8% increase in documentation of DNR status and a 27.2% increase in patients with health care power of attorney (Figure 4). We surpassed our goal of increasing by 20% the number of patients discharged from the ED with documentation in their medical record of their wishes regarding advance directives.
Discussion
Numerous barriers may prevent emergency physicians from having end-of-life discussions and obtaining advance directives. For physicians, these barriers included a fear that the patient would see the provider or treatment as a failure, cultural differences, and a reluctance to have in-depth conversations with patients and family members that the ED physician had never met before-especially if the patients had not previously had such discussions with physicians familiar with their case history. For patients and their families, barriers included cultural differences, a reluctance to initiate an end-of-life discussion, fear of patient abandonment, and denial of the need for a discussion about end-of-life issues, mortality, or poor health status. Barriers identified within the environment included time constraints and a belief among both providers and patients that the EC was not the most appropriate setting for a discussion about end-of-life issues. Barriers in the process included not knowing where to find advance directive forms or resources for end-of-life planning. Finally, barriers regarding documentation included concerns about the legal correctness of the advance directive documents and the process of extracting patients’ prognoses from the medical record.
The combined use of the screening tool and Advance Directive Discussion Template, addresses a number of barriers to discussing end-of-life issues. Nonetheless, it takes training and practice to become comfortable with addressing end-of-life issues with patients and families and subsequently documenting those discussions in the medical record. Structured documentation has been shown to increase follow through of the aim to have it entered in the chart. It is essential to identify roles within the ED team to avoid duplicity of work; a stronger definition of these roles of the various members of the staff is needed to strengthen implementation of the intervention in the future; and it would be helpful to have a multidisciplinary ACP document that is accessible to all providers for each patient. By addressing these barriers, we could potentially increase the percentage of patients leaving the ED with advance directives even further.
Healthcare providers need to be educated in EOL issues and care. The American College of Emergency Physicians recommended in the Choosing Wisely Initiative [10] “To not delay engaging in available palliative and hospice care services in the ED for patients likely to benefit.” To address the providers concern of time constrictions to conduct those sensitive conversation about EOL, we recommend a study other emergency centers wherein a palliative care team is incorporated into other Emergency Departments [11].
During this study, we noted many other benefits of addressing ACP through the ED. These included building trust and teamwork between patients, patients’ families, and health care teams; reducing uncertainty and conflict about the appropriate level of future care; providing peace of mind for patients and their families; and establishing a trustworthy, shared decision-making process.
In order to maintain our improvements in ACP in ED patients, we plan to coordinate an educational intervention to coach all ED clinicians on how to effectively address end-of-life issues. Physicians will also be trained to get code status clarification prior to hospital admission and to avoid unnecessary, expensive testing and aggressive therapy that is not aligned with a patient’s wishes and goals of care.
Limitations
This project was undertaken in the ED of a comprehensive cancer center. While the general barriers to ACP discussion may be universal, our patients represent a very specific subpopulation.
Our ED patients have generally established care at our facility which provides our clinicians with a wealth of information regarding the patient’s health status and social support. On call specialists for each of the oncologic services are available 24/7. A separate palliative care unit is available for patients whose goals of care have changed from curative intent to palliation at end-of-life. Patients seen in community emergency department setting will not likely have this extensive network of resources.
Rapport is a key element in these conversations. As a dedicated unit in a cancer center, our patients may be seen by the same ED provider across multiple visits. In keeping with their complexity and frequent comorbidities, our average patient stay is longer than those of a typical emergency center. These factors may allow our clinicians to establish a stronger rapport with the patient and their family than is typically seen in a community setting.
Patients with widely metastatic cancer, or who have failed multiple lines of therapy, may well have privately addressed the issue of their mortality outside of the medical setting. As they experience functional declines, they likely become more willing to address ACP with healthcare providers. Emergency departments in the community certainly see patients with chronic health issues. However they also have a large population of previously healthy patients whose acute illness, no matter how catastrophic, has left them little time to process the severity of their condition.
Conclusions
As physicians, our goal is to overcome disease. When this is not possible we must help patients understand their medical treatment options and allow them to make decisions regarding their care. While end-of-life conversations naturally involve grief and bereavement, they are essential to establish and honor the patient’s wishes. It is important to develop tools that address barriers to discussions about advanced care planning. Proactive interventions allow physicians to overcome these barriers and their own reluctance to discuss this topic and may provide a tool by which to document the patient’s wishes clearly in the record.
References
- Institute of Medicine (2015) Dying in america: improving quality and honoring individual preferences near the end of life. Mil Med 180: 365-367.
- Field MJ, Cassel CK (1997) Approaching death: improving care at the end of life. National Academic Press, Washington (DC).
- Hwang JP, Patlan J, de Achaval S, Escalante CP (2010) Survival in cancer patients after out-of-hospital cardiac arrest. Support Care Cancer 18: 51-55.
- Abel J, Pring A, Rich A, Malik T, Verne J (2013) The impact of advance care planning of place of death, a hospice retrospective cohort study. BMJ Support Palliat Care 3: 168-173.
- O'Sullivan R, Murphy A, O'Caoimh R, Cornally N, Svendrovski A, et al. (2016) Economic (gross cost) analysis of systematically implementing a programme of advance care planning in three Irish nursing homes. BMC Res Notes 9: 237.
- Higginson IJ, Sen-Gupta GJ (2000) Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med 3: 287-300.
- Duffy G, Moran J, Riley W (2009) Rapid cycle PDCA.
- Moss AH, Lunney JR, Culp S, Auber M, Kurian S, et al. (2010) Prognostic significance of the "surprise" question in cancer patients. J Palliat Med 13: 837-840.
- Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, et al. (2016) Standards for quality improvement reporting excellence 2.0: revised publication guidelines from a detailed consensus process. J Surg Res 200: 676-682.
- American College of Emergency Physicinas (2013) ACEP prepares list for choosing wisely campaign.
- Rosenberg M, Rosenberg L (2013) Integrated model of palliative care in the emergency department. West J Emerg Med 14: 633-636.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 5181
- [From(publication date):
March-2017 - Aug 15, 2025] - Breakdown by view type
- HTML page views : 4252
- PDF downloads : 929