Hereditary Multiple Exostoses Misdiagnosed as Rheumatoid Arthritis
Received: 20-Dec-2017 / Accepted Date: 16-Jan-2018 / Published Date: 23-Jan-2018 DOI: 10.4172/2167-7964.1000287
Abstract
Making a diagnosis of rheumatoid arthritis is often tricky. With no single test that confirms or eliminates the disease, the diagnosis of RA is based on a physical exam, patient history, laboratory tests and often imaging. However, symptoms of RA, such as pain, swelling and fatigue, are not exclusive to the disease. And correct diagnosis is important in choosing an appropriate treatment plan.
A number of diseases, such as lupus, fibromyalgia or Sjögren’s syndrome, may easily be confused with RA, or coexist in a patient. Arthritis symptoms might develop following certain infections, such as Lyme disease, tuberculosis, gastrointestinal infection or sexually-transmitted diseases. Patients with certain cancers, such as large granular lymphocyte (LGL) leukemia, have an increased incidence of RA, an acute leukemia in children may even be misdiagnosed as idiopathic juvenile arthritis.
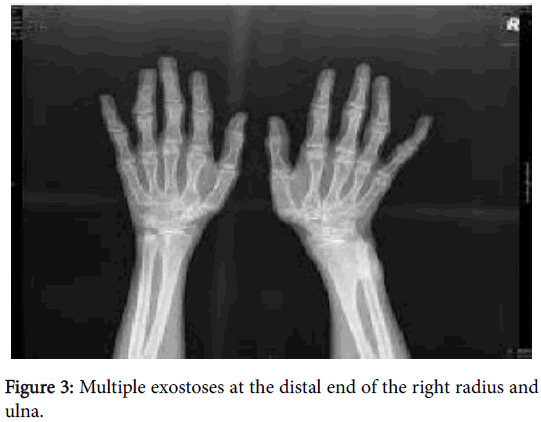
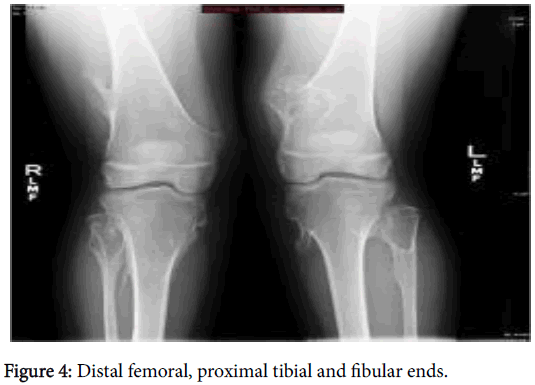
In this case report a 25 years male patient presented with arthralgia, fatigue, swelling of swelling of all MCPs, PIPs both wrists and knees, tender shoulders, Limited range of motion of right elbow, limitation of ROM of knees, severe cervical muscle spasm, was misdiagnosed as rheumatoid arthritis with 2ry Sjogren's syndrome with no response to treatment; imaging revealed multiple exostoses at distal end of Rt radius, ulna and distal femoral and tibial end.
Keywords: Rheumatoid arthritis; Adult; Arthralgia; Hereditary multiple exostoses
Introduction
Making a diagnosis of rheumatoid arthritis is often tricky. With no single test that confirms or eliminates the disease, the diagnosis of RA is based on a physical exam, patient history, laboratory tests and often imaging. However, symptoms of RA, such as pain, swelling and fatigue, are not exclusive to the disease. And correct diagnosis is important in choosing an appropriate treatment plan. A number of diseases, such as lupus, fibromyalgia or Sjögren’s syndrome, may easily be confused with RA, or coexist in a patient. In this case report a 25 years male patient was misdiagnosed as rheumatoid arthritis then revision of diagnosis was done secondary to imaging and was finally diagnosed as Hereditary multiple exostoses (HME) [1], also known as Multiple Osteochondromas (MO), which is a rare orphan autosomal dominant pediatric disorder that has an incidence of about 1:50,000 [2].
HME is characterized by nonmalignant cartilage-capped bony tumors-called osteochondromas or exostoses-that form within the perichondrium flanking the growth plates of long bones, ribs, hip, and vertebrae in very young and adolescent patients [3]. Patients often display a significant number of osteochondromas throughout their skeleton by the time the growth plates close at the end of puberty. Because of their location, sizes, and considerable number, osteochondromas can, and do, cause a number of health problems [4,5]. Surgery is currently the common treatment for HME patients and is used to resect the most symptomatic and problematic osteochondromas and ameliorate associated skeletal defects, such as skeletal element bowing, growth disparities, or nerve impingement [6,7]. In about 2% of the patients, osteochondromas can undergo malignant transformation, turning into chondrosarcomas or osteosarcomas that can be life threatening because of their typical resistance to chemo- or irradiation therapy [8,9].
Case Report
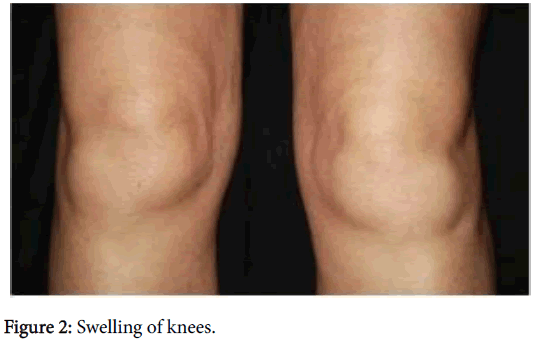
Male patient of age 25 years presented to OPD with history of generalized bony aches for two years, polyarthralgia mainly of small joints of hands, wrists, and knees with intermitted swelling, morning stiffness 15 min and dry mouth. He was diagnosed as rheumatoid arthritis with 2ry Sjogren's syndrome was on Methotrexate 25 mg/week S.C. injection, hydroxychloroquine 400 mg/d. prednisone 5 mg oral/day & NSAIDs with mild improvement. On examination there was swelling of all MCPs, PIPs (Figure 1) both wrists and knees (Figure 2), tender shoulders, Limited range of motion of right elbow, limitation of ROM of knees, severe cervical muscle spasm, all other findings were within normal limit. Family history was irrelevant, Vital signs were all normal.
Routine blood investigations were normal, all autoimmune profiles were negative, and MRI cervical and lumber was completely free. X rays hands (Figure 3) showed multiple exostoses at the distal end of the Rt. Radius & ulna. X rays knees (Figure 4) showed multiple bony exostosis projected from distal femoral and proximal tibial & fibular ends.
Discussion
The diagnosis was Hereditary multiple exostoses (HME), also known as Multiple Osteochondromas (MO). Clinical, radiological, immunological and epidemiological parameters play important role in diagnosis of Diaphyseal aclasis [10-13].
Osteochondromatosis is the most frequent benign bone tumor of the skeletal system [10,14-19]. Osteochondroma may occur in some short bones and may develope endochondral ossification despite its preference for long bones [19]. Affected individuals exhibit bilateral deformities and multiple osteochondromas in the hands, wrists, legs and feet. The forearms and wrists are the most common influenced sites. These deformities include relative shortening of the ulna, bowing of the radius, ulnar deviation of the distal aspect of the radius, wrist and hand [14-18]. In this case, all these deformities and multiple osteochondromas were present in defined locations.
The Management of HME is surgical, whereas the medical one is still at an experimental level.
Must be underlined that treatment of exostoses may be conservative if there are no clinical problems to avoid eventual surgical complications; also, spontaneous regression of the lesions has been documented in single cases during childhood and adolescence [20]. Surgery may be considered when symptoms appear: individuals affected by HME often undergo multiple interventions (sometimes greater than 20) to remove symptomatic osteochondromas or address deformities [21].
References
- Wicklund CL, Pauli RM, Johnson D, Hecht JT (1995) Natural history of hereditary multiple exostoses. Am J Med Genet 55: 43-46.
- Schmale GA, Conrad EU, Raskind WH (1994) The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 76: 986-992.
- Solomon L (1963) Hereditary multiple exostosis. J Bone Joint Surg 45: 292-304.
- Stieber JR, Dormans JP (2005) Manifestations of hereditary multiple exostoses. J Am Acad Orthop Surg 13: 110-120.
- Uchida K, Kurihara Y, Sekiguchi S, Doi Y, Matsuda K, et al. (1997) Spontaneous haemothorax caused by costal exostosis. Eur Respir J 10: 735-736.
- Dormans JP (2005) Pediatric orthopaedics: core knowledge in orthopaedics. Philadelphia: Elsevier, London.
- Jones KB (2011) Glycobiology and the growth plate: current concepts in multiple hereditary exostoses. J Pediatr Ortho 31: 577-586.
- Porter DE, Lonie L, Fraser M, Dobson-Stone C, Porter JR, et al. Severity of disease and risk in malignant change in hereditary multiple exostoses. J Bone Joint Surg Br 86: 1041-1046.
- Porter DE, Simpson AHRW (1999) The neoplastic pathogenesis of solitary and multiple osteochondromas. J Pathol 188: 119-125.
- Noonan KJ, Levenda A, Snead J, Feinberg JR, Mih A (2002) Evaluation of the forearm in untreated adult subjects with multiple hereditary osteochondromatosis. J Bone Joint Surg 84: 397-403.
- Peterson HA (1989) Multiple hereditary osteochondromata. Clin Ortho 239: 222-230.
- Porter DE, Emerton ME, Villanueva-Lopez F, Simpson AHRW (2000) Clinical and radiographic analysis of osteochondromas and growth disturbance in hereditary multiple exostoses. J Pediatr Ortho 20: 246-250.
- Vanhoenacker FM, Van Hul W, Wuyts W, Willems PJ, De Schepper AM (2001) Hereditary multiple exostoses: from genetics to clinical syndrome and complications. Eur J Radiol 40: 208-217.
- Faiyaz-Ul-Haque M, Ahmad W, Zaidi SHE, Hussain S, Haque S, et al. Novel mutations in the EXT1 gene in two consanguineous families affected with multiple hereditary exostoses (familial osteochondromatosis) Clin Genet 66: 144-151.
- Fogel GR, McElfresh EC, Peterson HA, Wicklund PT (1984) Management of deformities of the forearm in multiple hereditary osteochondromas. J Bone Joint Surg Am 66: 670-680.
- Wood VE, Sauser D, Mudge D (1985) The treatment of hereditary multiple exostosis of the upper extremity. J Hand Surg Am 10: 505-513.
- Peterson HA (1994) Deformities and problems of the forearm in children with multiple hereditary osteochondromata. J Pediatr Ortho 14: 92-100.
- Pritchett JW (1986) Lengthening the ulna in patients with hereditary multiple exostoses. J Bone Joint Surg Br 68: 561-565.
- Becelli R, Saltarel A, Santamaria S, Mastellone P, Gwanmesia I, et al. (2004) A case report of osteochondroma of the frontotemporosphenoidal suture. J Exp Clin Cancer Res 23: 147-151.
- Passanise AM, Mehlman CT, Wall EJ, Dieterle JP (2011) Radiographic evidence of regression of a solitary osteochondroma: a report of 4 cases and a literature review. J Pediatr Ortho 31: 312-316.
- Jager M, Westhoff B, Portier S, Leube B, Hardt K, et al. (2007) Clinical outcome and genotype in patients with hereditary multiple exostoses. J Orthop Res 25: 1541-1551.
Citation: El-Hadary HF, Saad S (2018) Hereditary Multiple Exostoses Misdiagnosed as Rheumatoid Arthritis. OMICS J Radiol 7: 287. DOI: 10.4172/2167-7964.1000287
Copyright: ©2018 El-Hadary HF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 7637
- [From(publication date): 0-2018 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 6640
- PDF downloads: 997