Research Article Open Access
Impact of Oral Health Education and Oral Prophylaxis on Quality of life of Controlled Diabetic Patients in Lasuth
Oyapero A1*, Adeniyi AA2, Sofola O3, Ogbera AO41Department of Preventive Dentistry, Lagos State University Teaching Hospital,Ikeja, Lagos, Nigeria
2Department of Preventive Dentistry, Lagos State University College of Medicine, Ikeja, Lagos, Nigeria
3Department of Preventive Dentistry, University of Lagos, Surulere, Lagos, Nigeria
4Department of Medicine, Lagos State University College of Medicine, Ikeja, Lagos, Nigeria
- *Corresponding Author:
- Dr. Oyapero A
Department of Preventive Dentistry
Lagos State University Teaching Hospital
Ikeja, Lagos, Nigeria
Tel: +234-1-8777845
E-mail: fola_ba@yahoo.com
Received Date: July 06, 2015; Accepted Date: July 20, 2015; Published Date: July 28, 2015
Citation: Oyapero A, Adeniyi AA, Sofola O, Ogbera AO (2015) Impact of Oral Health Education and Oral Prophylaxis on Quality of life of Controlled Diabetic Patients in Lasuth. J Oral Hyg Health 3:181. doi: 10.4172/2332-0702.1000181
Copyright: © 2015 Oyapero A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycaemia. In the oral cavity, diabetes mellitus may lead to salivary dysfunction, increased susceptibility of oral tissues to trauma and periodontal disease. There is a possibility that oral health education and oral prophylaxis may have a positive impact on the OHRQOL of diabetic patients. The purpose of this study therefore, was to evaluate the impact of Oral Health Education and oral prophylaxis on the OHRQOL of diabetic patients at the Lagos State University Teaching Hospital, Ikeja (LASUTH) using the Oral Health Impact Profile-14 (OHIP-14).
The study subjects had an interviewer-administered questionnaire employed to obtain information on their biodata, baseline OHIP-14 scores and periodontal/glycaemic parameters. They then received oral prophylaxis and oral health education and were reviewed at one, three and six months respectively. After 6 months, the periodontal and glycaemic parameters of the subjects were recorded again and the OHIP-14 form was used to evaluate the impact of the interventions on their OHRQOL. At baseline, subjects reported moderate and high impacts on their quality of life in the sub-domains of discomfort, pain, self-consciousness and embarrassment. The prevalence of moderate and severe periodontitis in this study population was 37.5%.
At the 6 months review, there was a significant reduction in the Fasting Blood Sugar and 2 hours Post Prandial glucose of the subject was compared to baseline scores. There was also a significant mean reduction in the periodontal parameters and an improvement in the OHRQOL of the subjects. The greatest improvement in OHRQOL was in the subdomain of discomfort, pain, self-consciousness and embarrassment. This study demonstrated that oral prophylaxis and oral health education may result in an improvement in the OHRQOL of the diabetic subjects. Further studies using a randomized controlled trial design are however recommended to validate these findings.
Keywords
Oral health related quality of life; Diabetes; LASUTH; Periodontal status; Glycaemic control
Introduction
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycaemia resulting from defects in insulin secretion, insulin action, or both [1]. Presently, diabetes is classified into four major classes: Type 1 diabetes; Type 2 diabetes; Gestational diabetes and other types of diabetes caused by specific conditions such as surgery, medications, infections, pancreatic disease and other illnesses [1]. It has been projected that at least 366 million people around the world will have diabetes mellitus by the year 2030 [2]. The prevalence of diabetes varies in each country. In the United States of America, it is 7.8% [3] while the prevalence in Nigeria ranges from 2.2% to 7.9% [4,5]. There are suggestions that the prevalence of diabetes is likely to rise along with the increase in non-communicable disease in Nigeria [6].
The chronic hyperglycemia of diabetes is associated with long-term damage of various organs, including the eyes, kidneys, nerves, heart, blood vessels and the oral cavity. In the oral cavity, diabetes mellitus may lead to salivary dysfunction, increased susceptibility of oral tissues to trauma, opportunistic infections (e.g., candidiasis) and periodontal disease [7,8]. Periodontal disease has been identified as the sixth complication of diabetes bringing to the fore the value of oral health in diabetic patients [9]. Patients with uncontrolled or poorly controlled diabetes are particularly susceptible to periodontal disease because of their poor immune response due to impaired polymorphonuclear leukocyte function. They also have an enhanced expression of inflammatory mediators such as cytokines and an increased production of oxygen free radicals. In addition, periodontal disease in diabetics may affect glycaemic control because of the production of pro-inflammatory mediators which mediate insulin resistance and reduce insulin action [10].
There has been a recent focus on the quality of life in health related research. Dietary restrictions, medication use, the actual symptoms of diabetes and concomitant diseases may lead to deterioration in the HRQOL in diabetic patients [11]. In most studies, poorer HRQOL was associated with hyperglycemia [11], insulin treatment, duration of diabetes, patient’s age and diabetic complications [12]. Research has also shown that the oral health status of diabetic patients has an impact on their Oral Health Related Quality of Life (OHRQOL) [13]. Periodontal disease in particular, often contributes to morbidity because of the decreased oral function and increased risk of tooth loss and thus has an impact on the OHRQOL [14].
Most of the oral conditions in diabetics are managed by simple preventive interventions such as oral health education, adequate home care, oral prophylaxis and appropriate dental recall visits. Research shows that periodontal treatment directed at the elimination of pathogenic species and the control of inflammation may have a positive impact on glycaemic control [15]. Treatment aimed at improving insulin sensitivity in poorly controlled diabetic patients also resulted in a reduction of periodontal inflammation [16]. Thus, prevention and control of established periodontal diseases should be considered an integral part of diabetes control [17]
Oral health education, an important tool in prevention has also been shown to result in significantly reduced gingival inflammation, Community Periodontal Index and Plaque Index scores in diabetic individuals with moderate to severe periodontal disease [18]. An assessment of the oral health attitudes, behaviour, and knowledge of patients with diabetes found that most of the participants were unaware of the oral health complications of diabetes mellitus and the need for preventive care [19]. Ayanbadejo et al. [20] obtained a similar result among Nigerian diabetic patients. Hence, there is a possibility that oral health education and oral prophylaxis will have an impact on the OHRQOL of diabetic patients. The purpose of this study therefore, was to assess the oral health related quality of life of controlled diabetic patients receiving care at the Lagos State University Teaching Hospital (LASUTH) and to evaluate the impact of oral health education and oral prophylaxis on their oral health related quality of life using the Oral Health Impact Profile (OHIP-14).
Materials and Methods
Study design
A prospective longitudinal intervention study on the impact of oral health education and oral prophylaxis on the oral health related quality of life of diabetic patients at the Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria.
Study setting and location
This study was conducted at the Diabetic Clinic (Department of Medicine) and at the Preventive Dentistry clinic of the Lagos State University Teaching Hospital, (LASUTH), Ikeja, Lagos, Nigeria. Lagos State University Teaching Hospital is a tertiary health facility situated in the capital of Lagos State. It is a multi-specialist hospital with a bed complement of 741.
Sample selection
All consecutive patients that presented at the LASUTH diabetic clinic on each clinic day during the study period were screened for possible inclusion in the study. Diabetic patients that had good glycaemic control evidenced by three previous results in their clinical records and who were willing to give their informed consent were included in the study after checking them with set inclusion and exclusion criteria.
Sample size determination
From reference study [21], the estimated sample size, 40 was computed using an equation for longitudinal intervention studies. With a provision for an attrition rate of 20%, the total sample size=48.
Eligibility criteria
Subjects included in the study were those that were 18 years or older and diagnosed as having had type 1 or 2 diabetes for at least one year before the study commenced. Eligible subjects had their case histories reviewed in the diabetic clinic to assess past compliance with their medication and control of their blood sugar. Patients that were excluded from the study included poorly controlled diabetics, those who had a known diabetic complication that could lead to hospitalization, and those that had a known risk of bacterial endocarditis. Hypertensive patients on calcium channel blockers such as Nifedipine, Diltiazem or Amlodipine that could precipitate gingival hyperplasia and further worsen gingival inflammation were also excluded. Those who would require several tooth extractions or had undergone periodontal treatment within 6 months prior to the study were also excluded.
Ethical aspects
The protocol and procedures for the study was presented to Health Research and Ethics Committee of the Lagos State University Teaching Hospital and written approval was obtained. The protocol was implemented in accordance with provisions of the Declaration of Helsinki.
All participants also completed a written informed consent.
Study protocol
Pretesting of the study instrument: A pretesting of the study instrument was done among 15 diabetic patients recruited from the LASUTH dental clinic. The instrument for data collection (questionnaire) was administered and checked for clarity and ease of administration. The oral health education leaflets were read and understood by the respondents.
Data collection
Questionnaires
Information obtained included gender, age, marital status, level of education, religion and dental history. The subjects’ phone numbers and email addresses were also obtained to facilitate recall visits and reinforcement of oral health education.
OHRQOL measurement with OHIP-14
The OHIP-14 [22], a 14-question instrument that focuses on seven dimensions of impact (functional limitation, pain, psychological discomfort, physical disability, psychological disability, social disability and handicap) was used. For each of the OHIP-14 questions subjects rated how frequently they had experienced an impact in the preceding months, on a 5-point Likert scale indicating if the problem had been experienced “very often” (code 4), “fairly often” (code 3), “sometimes” (code 2), “hardly ever” (code 1), or “never” (code 0). To calculate the OHIP-14 impact scores for individual domains, the mean of the subjects’ scores was obtained to give a maximum score of 4. For individual sub-domain scores 0, 1 and 2 were classified as low impact while scores 3 and 4 were classified as high impact. In order to calculate the overall OHIP-14 total impact score for all domains, item response codes were summed to give the final scores (Maximum obtainable impact score=56). The OHIP-14 final impact scores were classified as low (0-18.9), moderate (19-37.9) and high (38-56) to describe the impact level in the study population.
Glycaemic measurements
All the subjects had venous blood samples obtained to determine the Fasting blood glucose (FBG), postprandial blood glucose (PPG) and the Glycated hemoglobin (HbA1c). The blood chemical analysis for glycated haemoglobin (HbA1c) level (using the High Performance Liquid Chromatography) was done. The subjects had this investigation done in the morning on each visit at the BT Health and Diagnostics Unit, LASUTH and made the results available in the dental clinic on the appointment day.
Periodontal examination
A full-mouth periodontal examination was performed by the investigator for all respondents. A detailed periodontal examination was done and the Gingival Index (GI), Oral Hygiene Index-Simplified (OHI-S), Community Periodontal Index of Treatment Needs (CPITN) and the Clinical Attachment Level (CAL) and Probing Pocket Depth (PPD) scores of the patient were recorded.
Probing pocket depth (PPD) and Clinical attachment level (CAL)
Probing pocket depth (PPD): measurement from the gingival margin to the total probing depth, and clinical attachment level (CAL): measurement from the cemento-enamel junction to the total probing depth) was evaluated at six tooth surfaces (mesial, mesio-buccal, disto-buccal; mesio-lingual, disto-lingual, distal.) using a Williams periodontal probe. All the teeth were examined and only the third molars were excluded in the clinical assessment.
Intervention
Scaling and Root Planing (SRP)
Disclosing tablets was used to visualize dental plaque and to demonstrate plaque formation to the patient. Scaling and root planning was done for all the study participants to remove supra- and subgingival plaque by a Chief Dental Hygienist. Both ultrasonic and hand instruments were used for the procedure and on the average, about 45 minutes was spent on each patient. The teeth surfaces were then polished.
Oral Hygiene Instructions (OHI)
After the treatment session, the patients received a 10-minute oral health education session that included instructions on tooth brushing with pictorial information related to the method, frequency and duration as well as the use of oral health aids. A pack containing oral health educational leaflets with information on how to use a toothbrush and dental floss, how to clean bridges and dentures, and how to use a plaque disclosing tablet was given to the patients.
Recall visits
1 month recall visit
At the first recall visit, reinforcement of oral hygiene instructions was given to the patients. Oral health education leaflets were replaced if they had been lost. Another review appointment was scheduled in 2 months and the patient was advised to present in the clinic immediately if any complication arises.
3 months recall visit
At the second recall visit, diabetes related information (FBS, PPBS and HbA1C) was recorded. Reinforcement of oral hygiene instructions was done for the patients. Oral health education leaflets were replaced if they have been lost. Another review appointment was scheduled for 3 months but the patient was once again advised to present in the clinic immediately if any complication arises.
6 months recall visit
The OHIP-14 form was used to evaluate the impact of periodontal therapy and oral health education on the respondents’ quality of life. Diabetes related information (FBS, PPBS and HbA1C) was recorded. Each patient then had a repeat periodontal examination performed by the investigator.
Data analysis: Data was entered into the Microsoft Excel and analysed using SPSS (Statistical package for social sciences) for Windows (version 18, Chicago, IL) statistical software package. Frequency distribution tables were generated for all variables and measures of central tendency and dispersion were computed for numerical variables. Since the data were normally distributed, descriptive statistics including means, standard deviations, and percentages were used to summarize the demographic variables and health-related behaviour of the study sample. The Chi square test was used to determine the level of association between variables. The Student’s paired t tests and Anova tests were used to compare means while the Pearson’s correlation coefficient was used to determine the level of association between the variables. A 95% confidence interval and a 5% level of significance were adopted.
Results
1. Socio-demographic and diabetic characteristics of the study population.
The age distribution of the subjects ranged between 27 and 76 years. Most of the subjects (66.7%) were in the 46-65 years category and there were more females (60.4%) enrolled in the study. Majority of participants (79.2%) were married while (52.1%) had tertiary education. Most of the subjects (89.6%) had type 2 diabetes mellitus (Table 1).
| Frequency (%) | Percentage | ||
|---|---|---|---|
| Age range (years) | 26-45 | 6 | 12.50 |
| 46-65 | 32 | 66.70 | |
| 66-above | 10 | 20.80 | |
| Gender | Male | 19 | 39.60 |
| Female | 29 | 60.40 | |
| Marital Status | Married | 38 | 79.10 |
| Single | 2 | 4.20 | |
| Widowed | 7 | 14.60 | |
| Separated | 1 | 2.10 | |
| Education | None | 2 | 4.20 |
| Primary | 8 | 16.60 | |
| Seconday | 13 | 27.10 | |
| Tertiary | 25 | 52.10 | |
| Type of Diabetes | Type 1 | 5 | 10.40 |
| Type 2 | 43 | 89.60 | |
| Total | 48 | 100 | |
Table 1: Socio-demographic and diabetic characteristics of the study subjects
2. Reasons for dental attendance in the preceding year
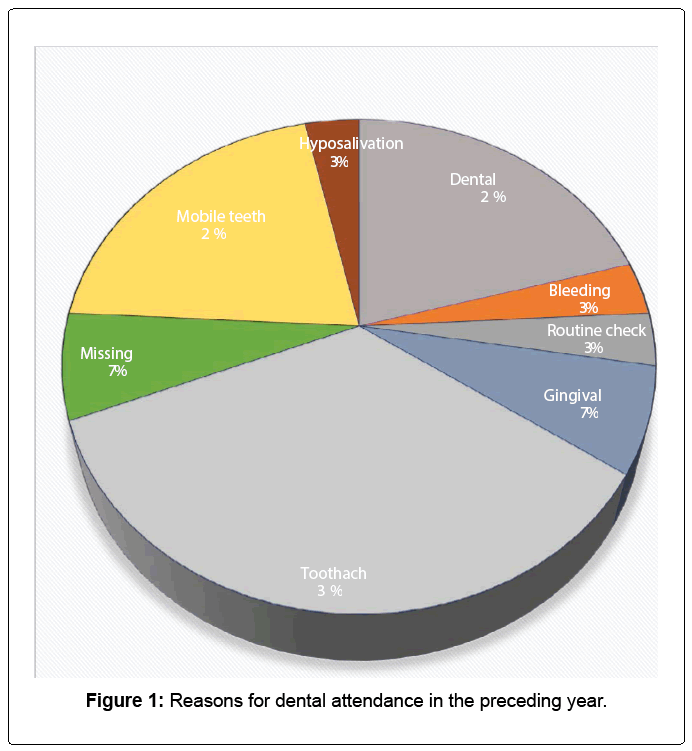
Of the 48 subjects, 29 (60.4%) had visited a dentist in the year preceding the study. Ten (35%) of the subjects who attended the dental clinic visited for toothache, 6 (21%) presented with mobile teeth and 6 (21%) had dental infections of which one was diagnosed as Ludwig’s angina. The rest had other conditions described in Figure 1.
3. OHRQOL of the study participants at baseline
The subjects’ OHIP-14 baseline scores are displayed in Table 2. At baseline, the highest OHRQOL scores were observed in the subdomains of pain, discomfort on chewing, self-consciousness and embarrassment. More than 20% of the subjects reported high impacts on the quality of life in these sub-domains. The highest mean impact score (1.92) was observed in the subdomain of discomfort on chewing. None of the subjects reported a high impact in the subdomain of occupation (jobs).
| OHIP Domains | OHIP-14 Sub-domains | Low Impact Band- 0, 1 and 2. | High Impact Band 3 and 4 | Mean OHIP-14 | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | Impact Score | |||
| Functional limitation Physical pain Psychological discomfort Physical disability Psychological disability Social disability Handicap |
Words Taste Pain Discomfort Consciousness Tense Diet Interrupt Not relaxed Embarrassed Irritable Job Life Function |
43 45 34 37 34 41 40 40 45 38 44 48 47 46 |
89.60 93.80 70.80 77.10 70.80 85.40 83.30 83.30 93.80 79.10 91.60 100 97.90 95.80 | 5 3 14 11 14 7 8 8 3 10 4 0 1 2 |
10.30 6.30 29.20 22.90 29.20 14.60 16.70 16.70 6.30 20.90 8.40 0 2.10 4.20 |
1.04 0.90 1.85 1.92 1.73 1.06 1.19 1.33 0.98 1.48 0.94 0.48 0.65 0.65 |
|
Table 2: OHRQOL of the study subjects at baseline.
4. Periodontal and glycaemic parameters of the subjects at baseline
The study subjects had a mean OHI-S score of 2.37 ± 1.10 while the mean gingival index score was 1.36 ± 0.75. The mean clinical attachment level was 3.30 ± 1.17 while the mean probing pocket depth measurement was 3.00 ± 1.26. Out of the 288 sextants examined in the 48 subjects, 111(38.5%) had CPITN scores of 3 and 4, while 37.5% of the subjects had moderate or severe periodontitis. The mean fasting blood sugar of the study subjects was 104.2 (±14.09) mg/dl while the mean 2hrs post prandial sugar reading was 126.1(±16.35) mg/dl. The mean glycated haemoglobin level was 5.32 (±0.22) (Table 3).
| Parameter | Range | Mean | SD | ||
| Fasting Blood Sugar (mg/dl) | 74-126 | 104.20 | ±14.09 | ||
| 2 hrs. Post Prandial (mg/dl) | 97-179 | 126.10 | ±16.35 | ||
| Glycated Haemoglobin (%) | 5-5.7 | 5.33 | ±0.22 | ||
| Parameter | Range | Mean | SD | ||
| Oral Hygiene Index Simplified | 0.5-5.5 | 2.37 | ±1.10 | ||
| Gingival Index | 0-3 | 1.36 | ±0.75 | ||
| Clinical Attachment Level (mm) | 0.5-6.67 | 3.30 | ± 1.17 | ||
| Probing Pocket Depth (mm) | 0.8-6.67 | 3.00 | ± 1.26 | ||
| Severity of periodontitis | N | Percentage (%) | |||
| None Moderate Severe Total |
30 17 1 48 |
62.5 35.4 2.1 100 |
|||
| Extent of Periodontitis | N | Percentage (%) | |||
| None Localised Generalised Total |
30 12 6 48 |
62.5 25 12.5 100 |
|||
| CPITN scores | N | Percentage (%) | |||
| 0 | 1 | 0.01 | |||
| 1 | 61 | 21.2 | |||
| 2 | 115 | 39.9 | |||
| 3 | 83 | 28.8 | |||
| 4 | 28 | 9.7 | |||
| TOTAL | 288 | 100 | |||
Table 3:Periodontal and glycaemic parameters of the subjects at baseline.
5. Association between the OHRQOL of the subjects and their baseline periodontal status
Subjects with poor oral hygiene had the highest overall mean OHIP-14 impact scores (18.15) even though the association was not statistically significant. (p= 0.196). There was however a significant association between the gingival index of subjects and OHIP-14 (p=0.001); probing pocket depth (p=0.002) and their clinical attachment level (p=0.005). The highest overall mean OHIP scores were observed in subjects with severe gingival inflammation; deep pockets and severe attachment loss. Subjects with generalised periodontitis had higher overall mean OHIP14 scores than those with localised periodontitis but the association was not significant (Table 4).
| Variable Oral Hygiene Index Simplified |
N | Low Impact (0- 18.9) N% |
ModerateImpact (19- 37.9) N% |
High Impact (38- 56) N% |
Mean SD OHIP14 |
|---|---|---|---|---|---|
| Good Fair Poor |
10 25 13 |
714.58 1531.25 816.67 |
36.25 510.42 48.33 |
00 510.42 12.08 |
14.70 ± 7.86 15.76 ± 11.70 18.15 ± 8.60 |
| Total | 48 | 3062.501225.006 | 12.50 | ||
| Gingival Index | χ2= 46.75df= 8p = 0. 1 | 96 | F =1.026P= 0.475 | ||
| Mild Moderate Severe |
23 19 6 |
1837.50 36.25 1020.84 612.50 24.17 36.25 |
4.17 6.25 12.08 |
12.61 ± 9.77 18.36 ± 9.71 23.00 ± 8.27 |
|
| Total | 48 | 3062.501225.006 | 12.50 | ||
| Probing Pocket Depth | χ2= 54.15df= 8p = 0.00 1 | ** | F=1.277P=0.002* | ||
| Shallow Moderate Deep |
32 15 1 |
2450.0 612.50 612.50 510.42 00 00 |
24.17 48.33 12.08 |
13.71 ± 9.58 20.86 ± 9.86 29.00 ± 0.00 |
|
| Total | 48 | 3062.501122.927 14.58 | |||
| Clinical Attachment Level | χ2=50.1 | 0df= 8p = 0.002 | ** | F=1.040P=0.004* | |
| Mild Moderate Severe |
30 17 1 |
2245.82 816.67 00 |
612.50 510.43 00 |
24.17 48.33 12.08 |
14.26 ± 9.48 19.05 ±10.81 28.00 ± 0.00 |
| Total | 48 | 3062.501122.927 | 14.58 | ||
| Extent of Periodontitis | χ2= 49.82df= 8p = 0.005** | F=1.015P=0.008* | |||
| None 30 Localised12 Generalised 6 |
2245.82 612.50 24.17 612.50 36.25 36.25 24.17 24.17 24.17 |
14.22 ± 7.52 24.05 ± 9.42 28.16 ± 8.68 |
|||
| Total 48 | 3062.501122.92714.58 | ||||
| χ2= 37.11df= 8p = 0.824 | F=1.222P=0.918 | ||||
Table 4: Association between the OHRQOL of the subjects and their baseline periodontal status.
-For data analysis, subjects with moderate and high impacts were merged. χ2 = Chi Square * Significant F= Anova
6. Changes in glycaemic parameters
A comparison of baseline and six months glycaemic parameters demonstrates statistical significant reductions in the FBS (4.09 mg/dl; p=0.04) and 2 hrs PPD (6.06 mg/dl; p=0.00) values. There was a small reduction in the HBA1C which was not statistically significant. (0.01 mg/dl; p=0.24) (Table 5).
| Paired Differences | T test | P value | |||||
|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) |
6 Months Mean (SD) |
Difference | 95% Confidence Interval of the Difference |
||||
| Lower | Upper | ||||||
| Fasting Blood Sugar |
104.42 (±14.08) |
100.33 (±15.32) |
4.09 | 0.17 | 7.99 | 2.10 | 0.04* |
| 2 hrs Post prandial | 126.10 (±16.35) |
120.04 (±16.28) |
6.06 | 1.64 | 10.47 | 2.76 | 0.00* |
| HBA1C | 5.33 (±0.22) |
5.32 (±0.36) |
0.01 | -0.14 | 0.03 | -1.17 | 0.24 |
* Significant
Table 5: Comparison of glycaemic parameters at baseline and at 6 months
7. Comparison of mean periodontal parameters and CPITN scores at baseline and at 6 months
There was a statistical significant improvement in all periodontal parameters using the paired T test. There was a mean reduction in OHI-S scores by 1.10 (p=0.000) while there was a mean reduction in Gingival Index scores by 0.61. (p=0.000) The mean PPD reduced by 0.44mm (p=0.000) while there was a mean CAL gain of 0.45 mm. (p=0.000). There was a decrease in the periodontal treatment needs of the subjects at the 6 months review when compared to the baseline scores. The number of sextants with CPITN scores of 4 reduced from 9.7% to 2.8%. There was an increase in the number of sextants with a score of 0 from 0.35% to 11.45%. Overall, there was an improvement in the periodontal status of the respondents using the CPITN index (Table 6).
| Paired Differences | T test | P value | |||||
|---|---|---|---|---|---|---|---|
| PERIODONTAL PARAMETERS | Baseline Mean (SD) | 6 Months Mean (SD) | Difference | 95% Confidence Interval of theDifference | |||
| Lower | Upper | ||||||
| OHIS | 2.37 (±1.10) | 1.27 (±0.73) | 1.10 | 0.92 | 1.28 | 12.36 | 0.000* |
| GINGIVAL INDEX | 1.36 (±0.75) | 0.88 (±0.59) | 0.48 | 0.37 | 0.59 | 8.82 | 0.000* |
| PPD | 3.00 (±1.26) | 2.56 (±1.22) | 0.44 | 0.36 | 0.54 | 10.01 | 0.000* |
| CAL | 3.30 (±1.17) | 2.85 (±1.18) | 0.45 | 0.31 | 0.58 | 6.84 | 0.000* |
| CPITNscores | No. of sextants at baseline | PercentageNo. of sextants at (%) 6 months | Percentage (%) | ||||
| 0 | 1 | 0.35 33 | 11.45 | ||||
| 1 | 61 | 21.18 111 | 38.54 | ||||
| 2 | 115 | 39.9352 | 18.06 | ||||
| 3 | 83 | 28.82 84 | 29.17 | ||||
| 4 | 28 | 9.72 8 | 2.78 | ||||
| TOTAL | 288 | 100 288 | 100 | ||||
* Significant
Table 6: Comparison of mean periodontal parameters and CPITN scores at baseline and at 6 months.
8. Comparison of the OHRQOL of the subjects at baseline and 6 months
There was a significant reduction in the overall and all sub-domain OHIP-14 scores in the subjects. The highest reduction in the scores was observed in the subdomain of discomfort (1.13); pain (1.02); Selfconsciousness (1.00) and embarrassment (0.88). The least reduction was noted in the sub-domain of jobs (0.23). The mean OHIP-14 scores and t test values are summarized in Table 7.
| OHIP-14 Sub-domains |
Paired | Differences | T test | P value | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline Mean |
6 Months Mean |
Difference | 95% Confidence Interval of the Difference |
|||||
| Lower | Upper | |||||||
| WORDS | 1.04 | 0.38 0.66 | 0.41 | 0.92 | 5.23 | 0.000* | ||
| TASTE | 0.90 | 0.43 0.47 | 0.26 | 0.70 | 4.30 | 0.000* | ||
| PAIN | 1.85 | 0.83 1.02 | 0.77 | 1.27 | 8.20 | 0.000* | ||
| DISCOMFORT | 1.92 | 0.79 1.13 | 0.87 | 1.38 | 8.76 | 0.000* | ||
| CONSCIOUS | 1.73 | 0.73 1.00 | 0.68 | 1.32 | 6.24 | 0.000* | ||
| TENSE | 1.06 | 0.40 0.66 | 0.43 | 0.91 | 5.54 | 0.000* | ||
| DIET | 1.19 | 0.48 0.71 | 0.41 | 1.01 | 4.76 | 0.000* | ||
| INTERRUPT | 1.33 | 0.42 0.91 | 0.62 | 1.22 | 6.18 | 0.000* | ||
| RELAX | 0.98 | 0.35 0.63 | 0.36 | 0.89 | 4.73 | 0.000* | ||
| EMBARRASS | 1.48 | 0.60 0.88 | 0.60 | 1.15 | 6.47 | 0.000* | ||
| IRRITABLE | 0.94 | 0.35 0.59 | 0.26 | 0.88 | 3.93 | 0.000* | ||
| JOBS | 0.48 | 0.25 0.23 | 0.00 | 0.37 | 2.03 | 0.048* | ||
| SATISFYING | 0.65 | 0.25 0.40 | 0.19 | 0.60 | 3.88 | 0.000* | ||
| FUNCTION | 0.65 | 0.21 0.44 | 0.19 | 0.73 | 3.45 | 0.001* | ||
* Significant
Table 7: Paired sample t test of baseline and 6 months OHIP-14 scores.
Discussion
The socio-demographic profile of the subjects in this study was similar to that observed by other researchers who aimed to determine the impact of oral prophylaxis on the OHRQOL of the general population. Majority of subjects in this sample were female and there was a preponderance of middle aged and elderly subjects. Type 2 diabetic patients made up 89.6% of the study population, which represents the prevalence in the general population which is about 90%. A history of dental visits based on symptoms was observed among the subjects. The prevailing reason for dental visits was toothache followed by mobile teeth, dental infections, gingival swelling and missing teeth. It was alarming that one of the subjects had presented in a dental clinic with Ludwig’s angina. These findings highlight the importance of preventive interventions and oral health promotion directed at diabetic patients to reverse this trend.
The study subjects reported negative impacts on their OHRQOL in all subdomains at baseline. The highest impacts were reported in the subdomains of discomfort on chewing and pain, psychological discomfort and psychological disability confirming the findings of previous researchers [23,24]. None of the subjects reported high impact in the sub-domain of occupation (jobs). This was probably because many of the subjects were in the retirement age bracket. These outcomes suggest that periodontal pain and aesthetics concerns have the greatest impact on the OHRQOL of the subjects. The study subjects also experienced more impacts on their quality of life with increasing age. Poor oral health has been shown to have a negative impact on daily life for a substantial proportion of older people [25]. These findings are not surprising, since periodontal status has been observed to decline with increasing age [7]. In the present study, females were also observed to report more impacts on their OHRQOL than males. Other researchers have also reported poorer OHRQOL in women [26]. One possible explanation for this tendency is that women care more about their health and their appearance and have greater aesthetic concerns than men.
At baseline, about half of the study subjects had moderate to severe gingivitis while the majority had fair or poor oral hygiene. About a third of the subjects had moderate clinical attachment loss and probing pocket depth. Subjects in this study that had higher glycaemic parameters were observed to have worse attachment levels and pocket depth. The highest mean OHIP-14 scores were also observed in patients with severe gingival inflammation, deep pockets and severe attachment loss. The extent of periodontitis was however not significantly associated with the OHRQOL of the subject confirming the findings of previous researchers [27]. It is important to note that even though type 1 and type 2 diabetes have dissimilar pathogenesis, there was no significant difference in the mean OHIP-14 scores of patients with type 1 and those with type 2 diabetes. The findings of this study, when considered with previous investigations, thus show, that periodontal disease is unequivocally linked with poor OHRQOL in diabetic patients.
Comparison of the glycaemic parameters at baseline and at 6 months shows significant reductions in the FBS and 2hrs PPG readings even though the overall reduction in HBA1C was not significant. Some researchers were unable to demonstrate a significant improvement in glycaemic parameters after oral prophylaxis [28]. The consensus of most recent investigators however is that oral prophylaxis has a positive impact on the glycaemic parameters of diabetic patients. A recent meta-analyses by Teeuw et al. [29] found that oral prophylaxis reduced HbA1c by 0.39% after 3 months of the periodontal treatment. This metaanalysis was in agreement with the researches of other investigator [30] who demonstrated that oral prophylaxis improves glycaemic control and reduces the level of inflammatory mediators. Oral prophylaxis leads to a reduction in these inflammatory mediators and may improve metabolic control by 0.4%. The effect of oral prophylaxis may thus be comparable to the effect of additional pharmacotherapy and hence, might find its place in the treatment of diabetic patients.
The study subjects also had statistically significant reduction in all periodontal parameters at the 6 months follow up visits when compared to baseline levels. This observation was in agreement with a systematic review by Heitz-Mayfield [31] on oral prophylaxis which showed that in patients with moderate CAL, oral prophylaxis resulted in 0.4 mm more clinical attachment gain and 0.4 mm less probing depth reduction. Measurements done with the CPITN index at baseline and at 6 months similarly demonstrated an improvement in the subjects periodontal treatment needs. These findings are encouraging since they demonstrate that oral health education and oral prophylaxis may reduce the need for advanced periodontal surgery procedures in this group of patients.
Simply improving clinical parameters like PPD reduction or CAL gain may however not be su cient if these improvements do not result in the establishment and maintenance of a functioning, disability free dentition for life. It is the improvement of the well-being and quality of life of the patients which should be the ultimate aim of healthcare professionals. The interventions provided in this study appeared to have led to a reduction in the impacts experienced by the subjects at 6 months. The OHRQOL of the subjects in this study measured with the OHIP-14 at 6 months showed an improvement in all subdomains. High impacts on the quality of life were experienced by less than 6.3% of the study subjects in all the subdomains while less than 18.8% experienced moderate impacts. The highest reduction in impact scores was in the sub-domain of discomfort with a mean reduction of 1.13. These findings corroborates that of other authors who noted that domains which improved after oral prophylaxis were the subdomains of discomfort and pain as well as that of psychological disability [23,24].
The social disability and handicap domains of OHIP-14 were reported earlier not to be associated with periodontal disease severity 23,24 and this might explain why these two subdomains were not significantly affected both at baseline and after oral prophylaxis. The results of this present study when considered with those previously documented by other researchers should stimulate further research since the principal goal of the dental profession is to improve the patients’ quality of life. The current report does not provide definitive evidence for the effectiveness of oral prophylaxis and oral health education on improving of OHRQOL. Even though we observed an improvement, the study methodology did not include a comparison control group(s) that could have clearly established the impact of the interventions. The study also did not establish with certainty that good glycaemic control and the subjects’ adherence to their medication did not contribute to the improvement observed. Future studies could compare the impact of these interventions on healthy non-diabetic patients, controlled diabetic patients and poorly controlled diabetic patients.
Conclusion
The study showed an improvement in the OHRQOL of the diabetic subjects at 6 months compared to their baseline recordings. This study observed this improvement through reduction of periodontal pain, improvement in mastication and self-esteem. However, there is insufficient evidence to prove that the improvement was solely as a result of the interventions given because of the absence of a comparison control group. Further studies with a randomized controlled trial design will be required to validate the findings of this research.
References
- Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2000) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 23 Suppl 1: S4-19.
- Zhang Y, Dall TM, Mann SE, Chen Y, Martin J, et al. (2009) The economic costs of undiagnosed diabetes. Popul Health Manag 12: 95-101.
- National Institute of Diabetes and Digestive and Kidney Diseases. National DiabetesStatistics, 2007 fact sheet. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, 2008.
- Akinkugbe OO, Akinyanju OO (1997) Final Report-National Survey on Non-Communicable Diseases in Nigeria: Federal Ministry of Health, Lagos 65-8.
- Nyenwe EA1, Odia OJ, Ihekwaba AE, Ojule A, Babatunde S (2003) Type 2 diabetes in adult Nigerians: a study of its prevalence and risk factors in Port Harcourt, Nigeria. Diabetes Res ClinPract 62: 177-185.
- Adeleye JO1, Agada NO, Balogun WO, Adetunji OR, Onyegbutulem HO (2006) Diabetes care in Nigeria: time for a paradigm shift. Afr J Med MedSci 35: 155-159.
- Collin HL1, Niskanen L, Uusitupa M, Töyry J, Collin P, et al. (2000) Oral symptoms and signs in elderly patients with type 2 diabetes mellitus. A focus on diabetic neuropathy. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 90: 299-305.
- Guggenheimer J, Moore PA, Rossie K, Myers D, Mongelluzzo MB, et al. (2000) Insulin-dependent diabetes mellitus and oral soft tissue pathologies. II. Prevalence and characteristics of Candida and candidal lesions. Oral Surg Oral Med Oral Pathol Oral RadiolEndod89:570-6.
- Löe H1 (1993) Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care 16: 329-334.
- Offenbacher S1, Salvi GE (1999) Induction of prostaglandin release from macrophages by bacterial endotoxin. Clin Infect Dis 28: 505-513.
- Stewart AL1, Greenfield S, Hays RD, Wells K, Rogers WH, et al. (1989) Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA 262: 907-913.
- Mayou R1, Bryant B, Turner R (1990) Quality of life in non-insulin-dependent diabetes and a comparison with insulin-dependent diabetes. J Psychosom Res 34: 1-11.
- Oyapero A, Adeniyi AA, Ogunbanjo BO, Ogbera AO. Periodontal Status and Oral HealthRelated Quality of Life among Diabetic Patients in Lagos State University Teaching Hospital, Ikeja. N J Clin. Med. 2011; 3(1): 78-85.
- Reisine S, Locker D. Social, psychological and economic impacts of oral conditions and treatments. In: Cohen LK, Gift HC, editor. Disease Prevention and Oral health Promotion. 1. Copenhagen: Munksgaard. 1995. pp. 33-72.
- Stewart JE1, Wager KA, Friedlander AH, Zadeh HH (2001) The effect of periodontal treatment on glycemic control in patients with type 2 diabetes mellitus. J ClinPeriodontol 28: 306-310.
- Matthews DC1 (2002) The relationship between diabetes and periodontal disease. J Can Dent Assoc 68: 161-164.
- Mealey BL, Rethman MP (2003) Periodontal disease and diabetes mellitus. Bidirectional relationship. Dent Today 22: 107-113.
- Almas K1, Al-Lazzam S, Al-Quadairi A (2003) The effect of oral hygiene instructions on diabetic type 2 male patients with periodontal diseases. J Contemp Dent Pract 4: 24-35.
- Moore PA1, Orchard T, Guggenheimer J, Weyant RJ (2000) Diabetes and oral health promotion: a survey of disease prevention behaviors. J Am Dent Assoc 131: 1333-1341.
- Ayanbadejo PO1, Savage KO, Jeboda SO (2004) Awareness of periodontal diseases amongst Nigerian diabetics. Odontostomatol Trop 27: 13-16.
- Ohrn K, Jonsson B. Oral health-related quality of life among patients with periodontal disease. https://dalea.du.se/research. Accessed February 20, 2012.
- Slade GD1 (1997) Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 25: 284-290.
- Pereira LJ1, Gazolla CM, Magalhães IB, Ramos-Jorge ML, Marques LS, et al. (2011) Treatment of chronic periodontitis and its impact on mastication. J Periodontol 82: 243-250.
- Aslund M, Suvan J, Moles DR., D’Aiuto F, Tonetti MS (2008) Effects of two di erent methods of non-surgical periodontal therapy on patient perception of pain and quality of life: a randomized controlled clinical trial. J Periodontol 79:1031-1040.
- Simpson TC1, Needleman I, Wild SH, Moles DR, Mills EJ (2010) Treatment of periodontal disease for glycaemic control in people with diabetes. Cochrane Database SystRev : CD004714.
- Einarson S1, Gerdin EW, Hugoson A (2009) Oral health impact on quality of life in an adult Swedish population. ActaOdontolScand 67: 85-93.
- Spangler L1, Reid RJ, Inge R, Newton KM, Hujoel P, et al. (2010) Cross-sectional study of periodontal care and Glycosylated Hemoglobin in an insured population. Diabetes Care 33: 1753-1758.
- Westfelt E, Rylander H, Blohme G, Jonasson P, Lindhe J (1996) The effect of periodontal th181. Smith GT, Greenbaum CJ, Johnson BD, Persson GR. Short-term responses to periodontal therapy in insulin-dependent diabetic patients. J Periodontol 67:794-802.
- Teeuw WJ1, Gerdes VE, Loos BG (2010) Effect of periodontal treatment on glycemic control of diabetic patients: a systematic review and meta-analysis. Diabetes Care 33: 421-427.
- Koromantzos PA1, Makrilakis K, Dereka X, Katsilambros N, Vrotsos IA, et al. (2011) A randomized, controlled trial on the effect of non-surgical periodontal therapy in patients with type 2 diabetes. Part I: effect on periodontal status and glycaemic control. J ClinPeriodontol 38: 142-147.
- Heitz-Mayfield LJ1, Trombelli L, Heitz F, Needleman I, Moles D (2002) A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J ClinPeriodontol 29 Suppl 3: 92-10 2.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 16392
- [From(publication date):
September-2015 - Sep 03, 2025] - Breakdown by view type
- HTML page views : 11481
- PDF downloads : 4911