Research Article Open Access
Latrine Utilization and Associated Factors in the Rural Communities of Gulomekada District, Tigray Region, North Ethiopia, 2013: A Community Based Cross-Sectional Study
Neguse Debesay1, Lalit Ingale2, Azeb Gebresilassie2, Huruy Assefa2 and Dejen Yemane2*
1Adigrat District Health Office, Adigrat, Ethiopia
2Department of Public Health, Mekelle University, Mekelle, Ethiopia
- *Corresponding Author:
- Dejen Yemane
Department of Public Health
Mekelle University
Mekelle, P.O. Box-1871, Ethiopia
Tel: +251-914420436
E-mail:yemaned@yahoo.com
Received date:February 05, 2015 Accepted date: March 11, 2015 Published date: March 14, 2015
Citation: Debesay N, Ingale L, Gebresilassie A, Assefa H, Yemane D (2015) Latrine Utilization and Associated Factors in the Rural Communities of Gulomekada District, Tigray Region, North Ethiopia, 2013: A Community Based Cross-Sectional Study. J Community Med Health Educ 5:338.doi: 10.4172/21610711.1000338
Copyright: © 2015 Debesay N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited..
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Though the Ethiopian government continued investing to increase access to improved latrine facilities, high access rates to household latrines are often not matched by high usage rates and open defecation still remains the predominant norm by rural households. Consequently, this study was conducted to assess latrine utilization and its determinant factors in the rural communities of Gulomekada district, Ethiopia. Method: A community based quantitative cross-sectional study was conducted on 759 rural households of Gulomekada district from February to July 2013. Multistage sampling technique was employed to select the sampled households and data was collected using a pre-tested, structured questionnaire and observational checklist. The data entry, cleaning and analysis were performed using SPSS version 16. Bi-variate and multivariate analysis was carried out to ascertain the association between dependent and independent variables. Results: A total of 756 households with latrines were assessed for their latrine utilization status. The rate of latrine utilization was 57.3% in the rural communities. Husband’s educational status of primary and above (AOR=3.71, 95%CI: 1.52-9.09), presence of school age children (AOR= 4.45, 95%CI: 1.32-14.97), family monthly income [AOR=10.85, 95%CI: 8.09-15.44], ownership of pit latrine with pit cover (AOR=7.86, 95%CI: 3.61-17.10), latrine construction material [AOR=2.55, 95%CI: 1.96-3.85], duration of owning latrine by the household [AOR=3.19, 95%CI: 2.04-4.98] were factors associated with latrine utilization. Conclusion: This study concluded that the latrine utilization rate of the households is not satisfactory. Presence of school age children, Husband’s educational status of primary and above, family monthly income, duration of owning latrine by the household, latrine construction materials and type of latrine were the major factors affecting utilization of latrines. Therefore, participatory approaches must be used to promote behavioral change of communities for sustainable and consistent latrine utilization.
Keywords
Latrine utilization; Prevalence; Associated factors; Rural community of Gulomekeda district; Northern Ethiopia
Introduction
Globally, about 2.6 billion people (39%) and almost half the population of developing regions were not using an improved form of sanitation in 2008. An estimated, 1.1 billion people did not use any facility at all and practiced open-defecation. The food and water contaminated with fecal matter can cause up to 2.5 billion cases of diarrhea among children under five, resulting in 1.5 million child deaths annually. Attaining better sanitation can reduce child diarrhea by 30%, and raise school attendance among girls [1,2].
In developing countries, like Southern Asia and Sub-Saharan Africa more than 80% of the diseases are caused due to inadequate and unsafe water supply, and improper disposal of waste [3,4]. In these regions, open defecation is still most widely practiced by 44% in Southern Asia and 27% in Sub-Saharan Africa [5]. Globally, an urban resident is 1.7 times more likely to use an improved sanitation facility than rural resident is. Around 2.6 billion people without improved sanitation of which 75% live in rural areas [1].
According to United Nations Children’s Emergency Fund (UNICEF), on community approaches to total sanitation globally 2.5 billion people including 840 million children do not use improved sanitation. Most of the rural population of Africa does not have access to safe and reliable toilets and for nearly 1 in 3 people practice the trend [6-8]. A cohort study conducted in semi-arid rural communities in Zimbabwe, reported that the latrine coverage was about 62%, but missed data in assessing utilization rate [9].
In India, improvements in water quality have reduced disease prevalence, lack of access to sanitation facilities and clean drinking water continues to be associated with diarrheal illness. Educational attainment was the only significant predictor of accurate disease prevention strategies or knowledge [10,11]. UNICEF observed that the sanitation and hygiene promotion based on community participatory approaches could lead to significant reduction of diarrhea in children in Turkana district in Kenya [12,13].
In Ethiopia, 60% of overall diseases are related to poor sanitation and lack of hygiene [3]. The case study conducted in Alaba and Mirab Abaya districts showed that a substantial increase in the number of household latrines, in a few years, and all latrines made of local materials. Regarding utilization, the study pointed 93% of households with latrines were utilized [14]. However, the Health Sector Development Plan – IV (HSDP-IV) shows that the utilization coverage in 2010 was 20% only [15,16].
A cross-sectional study conducted in Alaba special district revealed that households have limited access to sanitation and hygiene information. It also informed the importance of communication and behavioral factors in the sanitation and hygiene information access and level of latrine utilization [17]. Another study conducted in rural community of Hulet Ejju Enessie district, showed that latrine coverage in 2006 was 90%, and most (61%) households with traditional pit latrines had utilizing latrines [18].
In Ethiopia, still the national open defecation rate in 2010 was 46% (53% rural, and 9% at urban) [16]. The proportion of households with private improved toilet facilities was only 8%, 14% in urban areas and 7% in rural areas [16]. According to 2011 WASH report, the total latrine coverage in Tigray was 87%, and the utilization rate was only 34% [19].
Latrine utilization practice of community can be affected by different factors such as socio-demographic factors, access to health information, behavioral factors, socio-economic and latrine conditions like bad smell, lack of privacy if the shelter is inadequate, childhood habits that are hard to break. For example, elderly or uneducated people in rural areas may find it difficult to get used to new technologies and may resist the adoption of new behaviors [5,16,20].
Therefore, studies conducted in different parts of Ethiopia showed that the latrine utilization level differ from region to region of the country and from district to district within the same region depending on many factors. In Tigray region, there is no available research conducted to assess the latrine utilization rate. Hence, this study was designed to assess the latrine utilization level and associated factors of rural community separately in Gulomekada district, Tigray region, Northern Ethiopia.
Methods
Study area
The Gulomekada district is located at 912 km North of Addis Ababa and about 135 km North East of the Tigray regional city, Mekelle. There are 19 villages, 17 rural and 2 small towns in the district. In 2012, the total population is about 98,302 (48,167 are male and 50,134 are female), and of whom 86,038 live in rural area and the rest 12,260 in urban areas. In this district, the total number of households is 18,539, and out of it 16,158 Households live in the rural villages [21]. The geographic feature and settlement of households in the district is suitable for latrine construction. This study was conducted from February 2013–July 2013.
Study design
A community based cross-sectional study design was employed.
Sample size determination
The sample size was determined using single population formula with prevalence estimates of 34% (19), with a margin of error of 0.05% at the 95% confidence level. Then multiplying by a design effect of 2 and adding a 10% non-response rate, the total sample size was calculated to be 759.
Inclusion criteria
In selected kebeles of the district, households owned private latrine were included in the study and family members of 18 and above years old were interviewed for the study.
Exclusion criteria
Households who have not functional latrine were excluded from this study. The household with less than 18 years child were excluded from the study.
Sampling technique and procedures
A proportional sample size was allocated according to the number of kebeles in each stratum. Finally, 10 kebeles were selected from the 32 rural kebeles in the district. After the study kebeles had been identified the households were selected by systematic sampling method using the existing list of all households (obtained from registration books of health extension workers in the selected kebeles) as a sampling frame. A multistage sampling technique was employed to select the sample households. 5 kebeles (the smallest administrative unit in Ethiopia) were selected by simple random sampling using lottery method out of the 17 rural kebeles of Gulomekada district. Then, the sample size (759) was allocated using proportional to population size (PPS) to each of the selected kebeles. Interval (Kth) for selecting households was determined by dividing the number of households with the sample size allocated for each kebeles. After determining the Kth interval, the first household was selected randomly. The next households were identified systematically onwards by adding cumulatively Kth intervals to the first selected household.
Study variables
In the present study, dependent variable is latrine utilization and the independent variables are age, sex, educational status, religion, occupation and marital status, monthly household income, access to health information, individual perception, type of latrine, and duration since latrine constructed.
Data collection procedures
The data was collected using a structured face-to-face interview questionnaire, which includes socio-demographic and other characteristics that would measure the latrine utilization and associated factors after reviewing relevant literatures. The questionnaire was prepared in English first and then translated in to the local language, Tigrigna, and back translated to English to ensure the consistency of the thought of the questions.
Six (6) experienced data collectors were hired to collect the data and two days training on the content, objective and methods of data collection and interviewing technique was given to data collectors and supervisors. The supervision was done at each step of data collection by principal investigator and supervisors. An observational checklist was also used to observe the materials used for latrine construction, worn path to latrine, presence of fresh feces in the latrine, presence of water container, presence of water in the container, and presence of feces around the home.
Data quality control
One-week prior to the actual data collection period pretest was conducted and based on the finding, minor modifications of questions, wordings, phrases and time required to interview a respondent was made. During data collection time, a clear introduction that explains the purpose and objectives of the study was provided to respondents. A close supervision, honest communication and on spot decisions were conducted during data collection
Data processing and analysis
Collected data was checked for completeness, missing values and unlikely responses daily. The coded data was then entered, sorted and analyzed using Statistical Package of Social Sciences (SPSS) version 16.0. Descriptive statistics like frequency, distribution and percentage calculation were worked out for most of the variables. Bivariate and multivariate logistic regression analyses were performed to identify the factors affecting latrine utilization. Finally, 95% confidence interval (CI) and adjusted odds ratios (AORs) were computed in order to identify statistically significant associations between latrine utilization and associated factors. The level of statistical significance was set at P<0.05. The goodness of fit of the final model was checked using Hosmer and Lemeshow test of goodness of fit considering good fit at P-value>0.05 level of significance.
Ethical considerations
Ethical approval and clearance was obtained from the Institutional Review Board of College of Health Sciences, Mekelle University and Tigray Regional Health Bureau. Kebele administrators and interviewers were informed about the purpose of study, importance and duration of the study in order to get their free time and prior informed consent for the survey. Confidentiality was maintained and respondents were informed that participation was voluntary and they could withdraw at any time from the study. The right of participants to anonymity and confidentiality was ensured by making the questionnaire anonymous.
Results
Socio-demographic characteristics
A total of 756 households who have latrine were included in the study with 99.6% response rate. Of the total respondents 465 (61.5%) were males and 685(90.6%) of the respondents were head of the households. Men headed most of the households (63.47%). The mean age of the respondents was 50.48 years with an average household family size of 5.24. Regarding the educational status, about 78.9% of mothers and 50% of husbands were illiterates. From the interviewed households, about 50% have a medium (250-500 birr) monthly income (Table 1).
| Variables | Variable Category | Number (%) |
|---|---|---|
| Is respondent head of household | Yes | 685(90.6) |
| No | 71(9.4) | |
| Sex of respondents | Male | 465(61.5) |
| Female | 291 (38.5) | |
| Age (n=756) | Below mean (<50.48) | 402 (53.2) |
| Above mean (>50.48) | 354 (46.8) | |
| Marital status (n=756) | Single | 45(6.0) |
| Married | 550(72.8) | |
| Separated | 59(7.8) | |
| Widowed | 102(13.5) | |
| Head of household (n=685) | Father | 434(63.4) |
| Mother | 251(36.6) | |
| Educational status of husband (n=434) | Illiterate | 217(50) |
| Read & write | 83 (19.1) | |
| Informal or religious school | 32(7.4) | |
| Primary & above | 102(23.5) | |
| Educational status of wife (n=251) | Illiterate | 198(78.9) |
| Read & write | 27(10.8) | |
| Informal or religious school | 1(.4) | |
| Primary & above | 25(10) | |
| Husband occupation (n=434) | Farming and cattle rearing | 377(86.9) |
| Petty trader | 36(8.3) | |
| Formal employer(monthly salary) | 10(2.3) | |
| Daily laborer | 9(2.1) | |
| Other | 2(.5) | |
| Wife occupation (n=251) | House wife | 199(79.3) |
| Cattle rearing | 39(15.5) | |
| Petty trader(business) | 6(2.4) | |
| Formal employer(monthly salary) | 7(2.8) | |
| Monthly Income in Ethiopian birr (n=756) | Low (<250) | 48(6.3) |
| Medium(250-500) | 378(50) | |
| High(500-750) | 196(25.9) | |
| Very high(>750) | 134(17.7) | |
| Children in the household (n=756) | No school age children | 42(5.6) |
| Not attending formal education | 48(6.3) | |
| Some, but not all school age children attend | 452(59.3) | |
| Attending formal education | 214(28.3) | |
| Family size | Below average(<5.24) | 418(55.3) |
| Above average(>5.24) | 338(44.7) |
Table 1: Socio-demographic characteristics of the respondents in the rural community of Gulomekada district.
Assessment of latrine utilization status
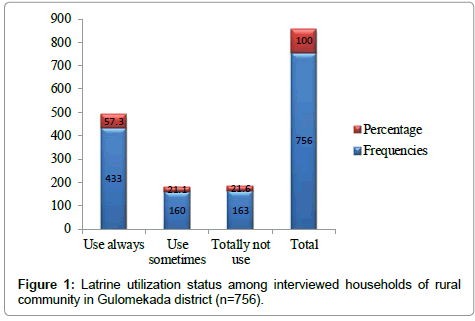
Out of the 756 households who have latrine, only 433 (57.3%) reported that they use latrine always, 160 (21.1%) use sometimes and 163 (21.6%) did not use latrine at all (Figure 1).
Reasons to use latrine
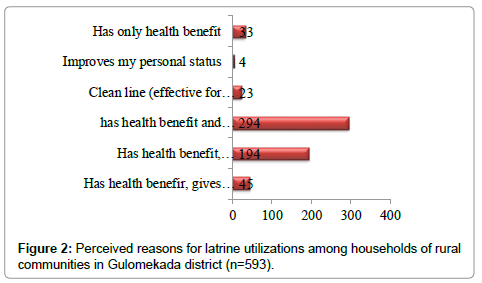
Individual perception (behavioral factors): The respondents who utilize latrine were asked for reasons why they utilize. Accordingly 294 (49.6%) of the respondents reported latrine utilization has health benefit and effective for environmental sanitation, followed by 194 (32.7%) were reported it has health benefit and effective for environmental sanitation, as well it improves personal status (Figure 2).
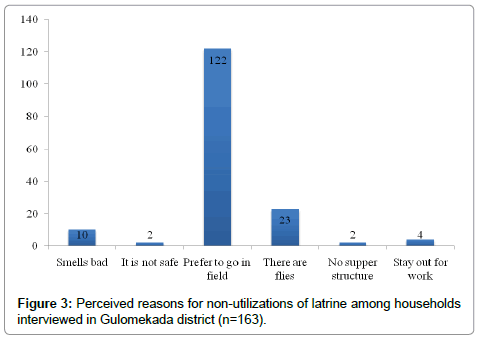
Perceived reasons not to use latrine: The reasons for nonutilization were also asked to 163 household who did not use latrine at all. Hence, preferring to go in field was the most frequent rated reason 122 (74.8%) followed by the presence of flies in the latrine which is 23(14.1%) (Figure 3).
Access for information (environmental factors): All respondents of this study (756) revealed that they were advised by different sources to use latrine. Two hundred ten (27.8%) and 173 (22.9%) respondents witnessed that they were advised by only health professionals and by health professionals and NGO’s respectively (Table 2).
| Variable | Variable category | Number (%) |
|---|---|---|
| Advisedto use latrine | Yes | 756(100) |
| No | 0 | |
| By whom do you advised to use latrine | Health professionals | 210(27.8) |
| Health Extension Workers | 61(8.0) | |
| NGO’s | 39(5.2) | |
| Public media | 23(3.0) | |
| Health professionals & administrators | 108(14.3) | |
| Health professionals & NGOs | 173(22.9) | |
| Health professionals, NGOs & public media | 76(10.1) | |
| Health professionals, administrators, Health Extension Workers & public media | 52(6.9) | |
| By All sources | 14(1.8) |
Table 2: Access of information on latrine utilization by respondents in the rural community of Gulomekada district.
Latrine condition (sanitation facility factors): The study observed that 563(74.5%) of available latrines are pit latrines with pit cover, and 149(19.7%) are VIP latrines. More than half (54%) of the latrines were constructed before 3 years and 62.8% of latrines were made up of local and industrialized materials (Table 3).
| Variable | Variable category | Number (%) |
|---|---|---|
| Type of latrine | Traditional pit without pit cover | 45(6.0) |
| Pit latrine with pit cover | 562(74.5) | |
| VIP latrine | 149(19.7) | |
| Latrine year of construction | <2 years | 218(28.8) |
| 2-3 years | 130(17.2) | |
| > 3 years | 408(54) | |
| Latrine construction materials | Locally available materials | 278(36.8) |
| locally unavailable materials | 6(.8) | |
| Mixedmaterials | 472(62.4) | |
| Clearly worm path | Yes | 604(79.9) |
| No | 152(20.1) |
Table 3: Households latrine condition in the rural community of Gulomekada district (n=756).
Predictors of Latrine Utilization
The selected variables were tested their individual contribution for latrine utilization through binary logistic analysis. The variables showed significant association were the mean age, marital status, husband educational status, presence of school age children in the household, head of the household, family size, family income, latrine type; years since latrine constructed, and latrine construction materials (P-value ≤ 0.2).
After that these predictors were entered together to determine their effect on the outcome variable (latrine utilization) through logistic regression model and six of the predictor variables, husband educational status, presence of school age children, family income, type of latrine, years since latrine constructed, and latrine construction materials remained significant predictors of latrine utilization.
The households with husbands educational status of primary and above were 3.71 times [AOR=3.71, 95%CI: 1.52-9.09] more likely to utilize latrine than households with illiterate husbands. The households with school age children, all attending the school were 4.45 times [AOR=4.45, 95%CI: 1.32-14.97] more likely to use latrine than households without school age children. The households with high monthly income were 10.86 times [AOR=10.85, 95%CI: 8.09-15.44] more likely to utilize latrine than households with very low income. The households who use mixed materials (locally available and unavailable materials) for construction of latrine were 2.55 times [AOR=2.55,95%CI: 1.96-3.85] more likely to utilize latrine than households who use locally available materials.
Concerning to latrine type, households owned pit latrine with pit cover were 7.86 times [AOR=7.86, 95%CI: 3.61-17.10] more likely to use latrine. The likelihood of using latrine was increased more and more by households owned VIP latrine. Regarding to construction year, households owned latrine for more than 3 years were 3.19 times [AOR=3.19, 95%CI: 2.04-4.98] more likely to use latrine (Table 4).
| Variables | Latrine utilization | COR (95%CI) | AOR (95%CI) | |
|---|---|---|---|---|
| Yes Freq (%) | No Freq (%) | |||
| Educational status of husband | ||||
| Illiterate@ | 160(73.7) | 57(26.3) | 1 | 1 |
| Read and Write | 67(80.7) | 16(19.3) | 1.49(.80-2.78) | 1.22(.61-2.44) |
| Primary and above | 95(93.1) | 7(6.9) | 4.84(2.12-11.03) | 3.71(1.52-9.09)** |
| Educational status of mother | ||||
| Illiterate@ | 139(70.2) | 59(29.8) | 1 | 1 |
| Read and Write | 26(96.3) | 1(3.7) | 11.04(1.46-83.23) | 10.44(1.37-79.62) |
| Primary and above | 22(88.0) | 3(12.0) | 3.12(.89-10.81) | 2.558(.72-9.09) |
| Monthly income(in Birr) | ||||
| <=250@ | 20(41.7) | 28(58.3) | 1 | 1 |
| 251-500 | 288(76.2) | 90(23.8) | 4.48(2.41-8.34) | 2.83(1.03-7.81) |
| 501-750 | 159(81.1) | 37(18.9) | 6.02(3.06-11.83) | 3.29(1.12-9.72) |
| >750 | 126(94.0) | 8(6.0) | 22.05(8.82-25.14) | 10.86(8.09-15.44)*** |
| Presence of School Age Children | ||||
| No school age children@ | 18(42.9) | 24(57.1) | 1 | 1 |
| Not attending formal education | 26(54.2) | 22(45.8) | 1.57(.68-3.63) | 1.23(.32-4.83) |
| Some attending formal education | 355(78.5) | 97(21.5) | 4.88(2.55-9.36) | 2.12(.73-6.08) |
| All attending formal education | 194(90.7) | 20(9.3) | 12.93(6.02-27.80) | 4.45(1.32-14.97) ** |
| Type of latrine | ||||
| Traditional pit without pit cover @ | 10(22.7) | 34(77.3) | 1 | 1 |
| Pit latrine with pit cover | 435(77.3) | 128(22.7) | 11.55(5.56-24.03) | 7.86(3.61-17.09)** |
| VIP latrine | 148(99.3) | 1(.7) | 503.20(62.23-4.063) | 226.01(27.02-1.893) |
| Duration of owning latrine by the household | ||||
| <2 years @ | 143(65.6) | 75(34.4) | 1 | 1 |
| 2-3 years | 96(73.8) | 34(26.2) | 1.48(.92-2.39) | 1.63(.95-2.79) |
| > 3 years | 354(86.8) | 54(13.2) | 3.44(2.31-5.13) | 3.19(2.04-4.98)** |
| Latrine construction materials | ||||
| Locally available materials @ | 171(61.5) | 107(38.5) | 1 | 1 |
| Locally unavailable materials | 5(83.3) | 1(16.7) | 3.13(.36-27.15) | .59(.055-6.47) |
| Mixed materials | 417(88.3) | 55(11.7) | 4.74(3.27-6.87) | 2.55(1.96-3.85)*** |
Significant at *P<.05; **P<0.01; ***P<0.001
AOR: Adjusted Odds Ratio.
COR: Crude Odds Ratio.
Table 4: The main predictors of latrine utilization in Gulomekada district (n=756).
Discussion
The findings of this study revealed that the rate of latrine utilization in rural community of Gulomekada district was about 57.3% similar with study commissioned in community of Hulet Ejju Enessie district, East Gojjam Zone, Amhara Region 60.7% [18] and differs from study done in Alaba and Mirab Abaya districts 93%, Ethiopia [4]. Result of this study is also comparable with Tigray 2011 baseline survey report on WASH, the utilization rate of latrine was 34% [19]. The disparity might be due to relatively better involvement of local Non-Governmental Organizations (NGO’s) and governmental interventions. In the present study district, there is no organized and continuous Community Led Total Sanitation and Participatory Hygiene and Sanitation Transformation intervention carried out except the advice and education provided by health extension workers, local administrators and local NGO’s (Catholic Church). The low use of latrines in our study area can be also explained health extension workers promote the benefits from constructing latrines among the rural communities, but have been less active in teaching proper utilization. The finding that,latrine utilization has health benefits and effective for environmental sanitation and personal status complemented this (Figure 2).
Though open defecation, which involves no method of excreta containment, increases human exposures to enteric pathogens and is considered a major risk to human health and development [22], this study revealed that preferring to go into open field (74.8%), and considering latrine as flies spreading place 23(14.1%) were perceived reasons for non-utilization of community latrine. This could be going to open field is perceived by the community to provide natural manure which would in turn improve the fertility of their fields as in case of cow dung and people were found unwilling to take responsibility of maintaining the cleanliness of these latrines. Similarly, study done in Denbia district, Northwest Ethiopia identified long live habit (60.4%) and considering open defecation comfortable (18.9%) as the most common reason for not utilizing of latrine by the households [23]. Study done in Hultu Ejju Enessie also identified non functionality of latrine and staying out for work as a reason for not using latrines [18].
The study observed that household with school age children, all attending the school were 4.45 times [AOR=4.45, 95%CI: 1.32-14.97] more likely to use latrine than households without school age children. This might be because school age children are “agent of change” in pacing the behavior and practice of their family and community at large. This finding is similar with a study done Denbia district, Northwest Ethiopia [23].
Households owned latrines for >3 years were utilizing more likely [AOR=3.19, 95%CI: 2.04-4.98] than owning latrines for less than two years. This might be because of the benefits they perceived to gain are immediate results like cleanliness, reduce flies and so on, and this encourages them to use latrine constantly. Latrine utilization was associated with type of latrine households owned. Households owned pit latrine with pit cover were more likely to use latrine [AOR=7.86, 95%CI: 3.61-17.10] than households with traditional pit latrine without pit cover. The probability of using latrine was increased more and more by households owned VIP latrine. This might be due to decrement in bad odor, which might be one of the reasons for not using latrine.
Households with husbands educational status of primary and above were 3.71 times [AOR=3.71, 95%CI: 1.52-9.09] more likely to utilize latrine than households with illiterate husbands. The possible elaboration for this is that education helps the literate household head to access the information from different sources than illiterate household head about the advantage of latrine utilization.
The likelihood of using a latrine was 10.86-fold higher in households that had a higher income than those with a lower income [AOR=10.85, 95%CI: 8.09-15.44]. This finding is in line with the results of a study conducted by Admassu M. in North Gondar, Ethiopia [24].
Regarding the latrine construction materials, households who use mixed materials (locally available and unavailable materials) for construction of latrine were 2.55 times [AOR=2.55, 95%CI: 1.96-3.85] more likely to utilize latrine than households who use locally available materials. This could be attributed to their income status.
Thus, households should be encouraged and enabled to improve the quality of their latrines. However, without being economically empowered to do so, many of the poor households, including many female-headed households will continue finding it difficult to adopt the measures since their financial positions may not permit them to do otherwise.
Since, the study has a limitation to formulate a casual association, recall bias and social desirability bias might have underestimated some of the findings.
Conclusion and Recommendations
This study concluded that almost the half of households with latrines was observed that they were not using latrine. The perceived reasons for not to use latrine by family members preferred to go in to field followed by the presence of flies in the latrine. Moreover, presence of school age children, educational status of husband and wife, family income, duration of owning latrine by the household, type of latrine and latrine construction materials were the major factors affecting utilization of latrines.
Based on the study findings, we recommend that;
Participatory approaches must be used to promote behavioral change of communities for sustainable and consistent latrine utilization.
Health professional at health facilities, health extension workers in outreach program, NGO’s, women’s development groups and other actors should provide more comprehensive and organized interventions.
Monitoring the community practice and provision of hygiene and sanitation education should be done regularly, repeatedly and continuously to adopt attitude, behavior and practice on latrine utilization among the communities.
Acknowledgements
We are grateful to the Mekelle University, Department of Public Health, College of Health Sciences for offering us such an opportunity to conduct this research. We would like to thank all the respondents participated in this study, data collectors and Mekelle Zonal Health Bureau Office. We also thank the anonymous reviewers for their great help, and the editor for their constant support.
Conflict of Interest
The authors declare that they have no competing interests.
Authors Contributions
ND: is responsible for generating the concept of this research paper, literature review and organization, preparation of draft proposal document, organizing data collection process, and preparation of draft data analysis and interpretation.
LI: is participated in research design process, interpretation process, preparation of scientific paper or the manuscript.
AG: is participated in research design process, presentation and interpretation process of result.
HA: is participated in research topic preparation process, research design process, data analysis, and interpretation process of result.
DY: is participated in research topic preparation process, research design process, data analysis, and interpretation process, and preparation of scientific paper or the manuscript and corresponding author of the manuscript.
These authors contributed equally to this work and approved the final manuscript.
References
- WHO/UNICEF (2010)Progress on Sanitation and Drinking Water. Geneva/New York, Switzerland/USA; WHO/UNICEF JMP
- Bill & Gates foundation. (2012) Water, Hygiene & Sanitation-Strategy Overview. Washington: Global Development program
- Seifu A (2011) Tilahun and AmsyS.Collick. Sanitation promotion and household latrine. Briefing note No-3.Bahir Dar, Ethiopia; Water Aid.
- Tefera W (2008) Technical Issues of Sanitation and Hygiene in Mirab Abaya and Alaba, a case study report from the Southern Nations Region (‘SNNPR’) of Ethiopia. Ethiopia; RiPPLE Working Paper 2
- United Nation (2001) The Millennium Development Goals Report. New York: UNITED NATION.
- EcoSanRes (2007) Toilets that make compost low cost, sanitary toilet that produce valuable compost for crops in an African context. SWEDEN: Stockholm Environmental institute.
- International Development Enterprise (IDE). Demand assessment for sanitary latrines in rural and urban areas of Colombia. Colombia: IDE
- International Development Enterprise (IDE) (2007) Supply chain assessment for sanitary latrines in rural and urban areas of Colombia. Colombia: IDE
- Root G (2001) Sanitation, community environments and childhood diarrhea in rural Zimbabwe. J Health PopulNutr 19:73-82.
- Gupta N, Mutukkanu T, Nadimuthu A, Thiyagaran I, Sullivan-Marx E (2012) Preventing waterborne diseases: Analysis of a community health worker program in rural Tamil Nadu India. J Community Health 37:513-519
- Nath K (2003) Home hygiene and environmental sanitation: a country situation analysis for India. International Journal of Environmental Health Research 13:S19-S28
- Kariuki JG, Magambo KJ, Njeruh MF, Muchiri EM, Nzioka SM, et al. (2012) Effects of Hygiene and Sanitation interventions on reducing diarrhea prevalence among children in resource constrained communities: case study of Turkana district, Kenya. J Community Health 37:1178-1184
- Kariuki JG, Magambo KJ, Njeruh MF, Muchiri EM, Nzioka SM, et al. (2012) Changing mothers hygiene and sanitation practices in resource constrained communities: case study of Turkana district. J Community Health 37:1185-1191
- RiPPLE(2008) Promoting sanitation and hygiene to rural households: lessons from the Southern Nations region of Ethiopia. SNNP, Ethiopia.
- FMoH. HSDP IV Annual Performance Report. Addis Abeba, Ethiopia: FMoH; 2011.
- WHO/UNICEF (2012) Estimate for the use of improved sanitation facilities. Addis Ababa, Ethiopia; WHO/UNICEF JMP.
- Regassa N, Rajan S, Ketsla K (2011) Access to, and utilization of information on sanitation & hygiene by rural households in Alaba special district. J Hum Ecol 33:102-112.
- Anteneh A, Kumie A (2010) Assessment of the impact of latrine utilization on diarrheal diseases in the rural community of HusetEjjuEnessie District, East Gojam Zone, Amhara Region. Ethiop J Health Dev 24:110-118.
- Admasu A, Kiros M, Memhur A (2011) Baseline Survey Report of Tigray Region on Wash.Tigray, Ethiopia; WASH Program
- Labspace(2011) Latrine utilization-Changing attitudes and behaviors, Ethiopia.
- WHO. Woreda annual Health plan for EFY 2005.Fasti, Gulomekada, Tigray, Ethiopia; EFY 2005.
- Waddington H, Snilstveit B, White H, Fewtrell L(2009) Water, sanitation, and hygiene interventions to combat childhood diarrhea in developing countries. Int. Initiative Impact Eval1:1-115
- Yimam YT, Gelaye KA, Chercos DH(2014) Latrine utilization and associated factors among people living in rural areas of Denbia district, Northwest Ethiopia, 2013, a cross-sectional study. Pan Afr Med J. 18:334.
- Admassu M, Wubshet M, Wubshet T (2004) Sanitary Survey in Gondar Town. Ethiop J Heal Dev 18:39-42.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 17983
- [From(publication date):
April-2015 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 12869
- PDF downloads : 5114