Research Article Open Access
Living on the Edge: The Role of Critical Incidents on the Development of Secondary Resilience in Physicians
Svyatoslav Petrov*USA
- *Corresponding Author:
- E-mail: spetrov1@bu.edu
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
This qualitative, phenomenological case-study focuses on physician-reported experiences related to caring for refugees, in order to investigate what experiential factors contribute to effective therapeutic relationships. Findings and medical literature show that caring for refugees can have adverse psychological and physiological repercussions for physicians. Extensive exposure to trauma narratives and vivid examples of human suffering can lead to burnout, vicarious trauma, and/or secondary traumatic stress – affecting physicians’ ability to care for patients effectively. Nonetheless, emerging psychological literature indicates that, over time, providers may be able to develop vicarious resilience by mirroring the resiliency of their patients. This notion is based on theory that chronic exposure to patient suffering can bolster social advocacy and altruistic behavior in providers. Supplementing this theory, the data shows that providers can develop “secondary resilience” after a single exposure to a critical incident, that evaluation of critical incidents is the link between secondary traumatic stress/vicarious trauma and secondary and/or vicarious resilience, and that secondary/vicarious resilience can coexist with vicarious trauma or secondary traumatic stress, allowing physicians to continue caring even as they witness suffering and suffer with their patients.
Keywords
Critical Incidents; Vicarious Trauma; Secondary Traumatic Stress; Burnout; Resilience; Secondary Resilience; Vicarious Resilience; Refugees; Clinicians; Physicians
Introduction
So I had this lady, who was an asylum seeker, who had been pregnant as the result of rape during her detention, where she'd been tortured and raped. And...um...so I took care of her through her whole pregnancy...we tend not to discuss...you know... their trauma history in detail, other than to know that it occurred and....you know...try to make sure they get services, that they’re OK and go over the whole 'how's mental health?' and...you know...make resources, but to talk about the details of what happened we didn't do, but then she needed her asylum affidavit, so she came back to me for that...[tears began to well up in the doctor's eyes]...she had her new baby on her lap, this little boy that's the result of rape from someone who tortured her, she is sitting there telling me this story and suddenly she completely flashes back, she dissociates and starts rocking and saying 'God help me, God help me, God help me' and her little boy, sitting on her lap, starts to cry because he sees that mommy is, you know, in distress and that's what grounds her (her little boy's cry) and brings her back to reality and she goes 'I'm sorry honey I didn't mean…’ I'm going to cry [tears streak down the doctor’s cheeks]... (sobs)...’I didn't mean to upset you (the little boy)’... and it just showed me the resilience and the deep quality of the people that I deal with...(sniffles)...and what great people they are as they survived their trauma and...um... it kind of makes the work feel very rewarding that you can at least help somebody to get back to their survival potential…(sniffles and dries tears)...1
Dr. Lindquist’s narrative is a powerful testament to the emotional cost of caring for vulnerable populations, for physicians. During the interview process, as the physicians I interviewed recounted their experiences of caring for refugee and asylee patients, they showed deep emotional reactions. Chronic exposure to patient narratives of loss, grief, and trauma can elicit intense emotions such as profound sadness, helplessness, frustration, and hopelessness in clinicians. Such emotional responses are frequently termed vicarious trauma or secondary traumatic stress. My research findings and that of other studies (Hesse, 2002; Holmqvist & Andersen, 2003; Hernandez- Wolfe, Killian, Engstrom & Gangsei, 2014) indicate that when providers engage in empathetic relationships with vulnerable patient groups (i.e. refugees), they undergo inner, transformative processes that impact them on the emotional, psychological, and intellectual levels.
These transformations often occur after clinicians have experienced a critical incident – “any event that has a stressful impact sufficient enough to overwhelm the usually effective coping skills of an individual” – during his or her interaction with a patient (Mitchell & Bray, 1990). If left unaddressed, critical incidents can have a detrimental effect on physicians’ ability to process and move past vivid images of patient suffering, death and dying. Additionally, evidence shows that unchecked vicarious trauma can lead to professional burnout and compassion fatigue and, thereby jeopardize effective physician-patient relationships.
In the context of my research, I refer to the “physician-patient relationship” not as a long-standing interaction or a deeply affiliative emotional exchange, but as a synonym for clinical empathy that harnesses physicians’ ability to understand a refugee patient’s cultural background, health needs, and narratives of suffering, and emotional experiences. I argue that this strengthens rather than undermines objective diagnostic and therapeutic processes. Clinical empathy can supplement or complement the clinical objective knowledge to produce a more comprehensive understanding of a refugee patient:
Empathetic communication enables patients to talk about stigmatized issues that relate to their health that might otherwise never be disclosed, thus leading to a fuller understanding of patients’ illness experiences, health habits, psychological needs, and social situations (Halpern, 2001)
But does the presence of empathy mean that clinical objectivity is lost? That clinicians can no longer offer quality, effective care if clinicians pay too much attention to their own or their patients’ emotions? Does emotional distance remain valid when clinicians working with vulnerable populations develop professional burnout, psychiatric disorders, or suicidal ideations? What does it mean to be an empathetic clinician? According to More (1996), “the empathic physician is neither objective nor subjective, neither detached nor identified, but dialogically linked to the patient in a continuing cycle of reflexive interpretation that integrates the objective and subjective” (245).
This qualitative, phenomenological case-study focuses on physician-reported experiences caring for refugees in order to investigate what experiential factors contribute to effective therapeutic relationships. My choice to focus on “experiential” factors is based on my interest in the practical knowledge and skills learned by physicians through their lived-experiences caring for refugee and asylee patients. In other words, I was interested in the “process whereby knowledge is created through transformation of experience” (Kolb, 1984). In an attempt to answer this research question as thoroughly as possible, this study also aimed to:
(1) explore physicians’ experiences caring for refugees/asylees;
(2) identify thoughts about, and clinical challenges associated with, working in refugee care;
(3) identify whether or not physicians experience critical incidents during their career in refugee care, and how (if) these critical incidents impacted their professional and/or moral development.
Based on accounts such as Dr. Lindquist’s, my physician-informants were not distant from their patients but present empathetically. In many ways, their experience of deep emotional connection to their patients challenges the traditional and contemporary notions that emphasize “affective neutrality” or “neutral empathy” commonly taught in medical schools in the U.S. My informants’ input indicates that emotions have a place in medicine. The level of emotion conveyed by clinicians in this study indicated that empathy is not so detached and limitless; it has a tipping point. It can be broken; indeed, shattered. When this occurs, the protective walls of emotional neutrality crumble. In these instances, burnout, vicarious trauma, or secondary traumatic stress can ensue and debilitate highly intellectual, well-meaning practitioners who chose medicine out of a deep concern and desire to help people.
However, newly emerging evidence indicates that clinicians can move beyond and cope with vicarious trauma through vicarious resilience, or what I introduce as, “secondary resilience.” This notion is based on theory that clinicians’ exposure to patient suffering can bolster their desire to help patients and to advocate and harness social resources for specific patient groups (e.g. refugees, torture survivors, asylees). In this sense, resiliency is both a protective trait and a factor that mitigates symptoms of vicarious trauma. Moreover, one of the central arguments produced from this study is that there is a missing link between vicarious trauma or secondary traumatic stress and vicarious resilience or “secondary resilience.” I argue that the missing link is the systematic evaluation of critical incidents.
Methods
During 2013-2015, I developed and carried out an intensive qualitative, phenomenological study focusing on the lived experiences of physicians in a refugee center at a New England, safety-net hospital. As stated by Bernard (2011), "in a phenomenological study, the researcher tries to see reality [the lived-experiences] through another person's eyes." In this sense, the purpose of this study was not necessarily to produce generalizable data about physicians as a whole, but to contribute knowledge valuable for better understanding and evaluating the delivery of quality care, improvement of health outcomes, policy origination, and resident education. In particular, I sought to explore what physicians who care for some of the most vulnerable patients might say about how this type of health care work affects them as providers.
On theoretical grounds, I sought "to understand the perspective of those being studied," hence the decision to utilize qualitative research methodology (Bryman, 1988). Additionally, due to the small number of informants available in the research site, qualitative research methods were both more feasible and optimal for reliable data collection (Harding, 2013).
In order to best address the research questions, I used purposive, nonrandom sampling to select physicians who care for diverse refugee/asylee populations at a large safety net hospital in the Boston area (Harding, 2013). Due to the number of clinicians affiliated with the refugee center, purposive sampling allowed me to focus on the depth and quality of information provided by each informant, and to emphasize their unique experiences with the patient population.
In total, I interviewed all of the clinicians affiliated with the center, for an n of six physicians, as well as one key informant patient at the Center, who I met outside of the clinical context, at the center’s annual Gala. Of the six physician informants, two were male and four were female. Two specialized in psychiatry, two in OB/GYN, one in infectious diseases, and one in Family Medicine. The mean length of time specializing in caring for refugees/asylees was approximately twenty years.
With these principles in mind, the operationalization, data collection and qualitative analysis process was triangulated to cross-reference informants' input with field and cyber-participant observation (participant observation of virtual or online content), systematic observation of digital content provided by the Center, and respondents' own publications, and video content.
I conducted in-depth, semi-structured interviews in order to capture physicians' experiences and perspectives caring for refugee groups. The duration of each interview was approximately 60 minutes. I recorded and transcribed each interview using Word and Audacity - a secure, sound editing software. Additionally, I imported the typed transcripts into NVivo10 qualitative data analysis software and coded with a combination of thematic apriori and empirical codes that stemmed from narrative and discursive analysis.
Further, because informants had emotional responses speaking about their experiences caring for refugee patients, I performed a second round of coding to capture the meaning and context of their emotions. As accentuated by Saldana (2012), "since emotions are a universal human experience, our acknowledgement of them in our research provides deep insight into the participants' perspectives, worldviews, and life conditions." Accordingly, I used emotion codes - "label[ing] the emotions recalled and/or experienced by the participant, or inferred by the researcher about the participant " - for cathartic interview segments (Saldana, 2012).
Pre and post coding, I employed the constant comparative method to identify similarities and differences between each interview. The key reason for using the constant comparative method is identified by Dey (2004): 'Comparison is the engine through which we can generate insights, by identifying patterns of similarity or difference within the data'" (Harding, 2013). To triangulate the data, I conducted field participant observation in two public events sponsored by the refugee Center and analyzed document and online content produced by the Center and its clinicians applying the identical coding process utilized for interview data.
Empathy is the Proximal Risk Factor for Secondary Traumatic Stress & Vicarious Trauma
Physicians who care for vulnerable populations may be at an increased risk of experiencing adverse psychological and physiological effects. Psychological and medical literature tends to define these psychological effects with overlapping, yet unique concepts such as compassion fatigue, burnout, secondary traumatic stress, vicarious trauma, secondary victimization, counter-transference, empathetic strain, and emotional contagion (Miller, Stiff, & Ellis, 1988; Perry, Conroy & Ravitz, 1991; Joinson, 1992; Figley, 1995a; Eisenman, Bergner, & Cohen, 2000; Kinzie, 2001; Hesse, 2002; Holmqvist & Andersen, 2003; Trippany, White, & Wilcoxon, 2004).
Despite the related and interchangeable nature of the above effects, each one has distinct characteristics. According to theorists (Figley, 1995a; Figley & Kleber, 1995; Hesse, 2002; Pines & Aronsen, 1988; Trippany, White, & Wilcoxon, 2004), burnout develops over a long period of time, is often work-related, predictable and is the outcome of emotional exhaustion, while secondary traumatic stress (also synonymized with “compassion fatigue”) is less predictable and can emerge suddenly after a critical incident. Figley (1995a) suggests that secondary traumatic stress can occur in professionals who provide care to the directly traumatized individuals. In other words, the trauma experienced by a client/patient transitions into a traumatizing event for the provider (Perry, Conroy & Ravitz, 1991). In some cases, caregivers can relate to the traumatic experiences of patients with PTSD to such an extent that they begin to mirror the same symptoms the patient is experiencing (Baird & Kracen, 2006). Consequently, symptoms of secondary traumatic stress are often identical to symptoms associated with post-traumatic stress disorder. Although the symptoms of secondary trauma are nearly identical to vicarious trauma, the onset of secondary trauma can occur immediately after a single incident while vicarious trauma develops as a response to prolonged exposure to patient suffering (Figley, 1995).
Emotionally, symptoms such as sadness, irritability, hyper-arousal, cynicism, as well “feelings of being helpless, hopeless and/or powerless, feelings of lack of safety [and] trust, alienation from others, shattered assumptions about basic beliefs about life or people, [and/or] loss of faith (anger with God)” are strong indicators for the presence of vicarious or secondary trauma (BSRC, 2012; Smith, Keller & Lhewa, 2007). Providers may also experience behavioral changes such as increased substance abuse, and work-related changes such as tardiness and absenteeism (Smith, Keller & Lhewa, 2007). In addition, providers may report changes in their sociability, mood swings, heightened irritability, social withdrawal, and impatience (Kahill, 1988; Kinzie, 1994; Kleber & Fingley, 1995, Smith, Keller & Lhewa, 2007)
Although vicarious or secondary trauma is understudied in physicians caring for refugee/asylee patients, hypothetically speaking, all are “at risk.” The danger is that when high levels of stress become normalized or expected in medical settings, they are easily overlooked. The emotional burden providers experience has physiological ramifications. These include stress-related sleep disorders, heart disease, high blood pressure, joint pain, general fatigue, increased susceptibility to colds/flu, addiction, headaches, eating problems, nervous ticks, etc (BSRC, 2012; Smith, Keller & Lhewa, 2007). At the environmental level, factors such as “ineffective supervision, large caseloads, lack of recovery time between client contacts, traumatized or complex clients, lack of team approach in the workplace, and a lack of supports to meet client/patient needs” may increase the risk of some providers to develop vicarious or secondary trauma (BSRC, 2012). Acknowledging these realities, through a short paragraph and bullet points, the Center’s “Caring for Survivors” online course and a slide presentation on the “Ethnocultural Aspects of Refugees and Survivors of Torture” urge providers to prepare themselves to hear difficult narratives and warn health professionals of potential vicarious traumatization. Further, under the section related to preparatory interview considerations, the course provides a few sentences that state that having discussions with a mentor or other colleagues about emotions that occur before and/or after clinical interviews can help providers avoid symptoms associated with vicarious trauma. This is especially advised for new clinicians entering refugee/asylee care.
Interestingly, the risk factor that is sometimes absent in modern literature on physician burnout or vicarious or secondary trauma is empathy itself. According to Smith, Keller & Lhewa (2007), a work produced by physicians and clinical social workers, empathy is both a “hallmark of a caregiver’s ability to engage in effective therapeutic treatment with traumatized clients” and “one of the primary factors that contribute to secondary traumatic stress” (397). Empathy can help the provider to understand a patient’s experiences, yet it may make providers vulnerable to becoming traumatized themselves (Figley, 1995b; Wilson & Lindy, 1994, Smith, Keller & Lhewa, 2007).
Providers and theorists posit that caregiver expectations, ideals, outlooks, and hopes can have a significant impact on the development of adverse psychological reactions such as burnout, secondary traumatic stress or vicarious trauma. Kleber (2003) argues that some providers may feel a sense of powerlessness when they care for individual people but are unable to address the core of world-scale tragedies that produce their client/patient population. Maslach & Jackson (1981), Hesse (2002), and Trippany, White & Wilcoxon (2004) propose that providers may have a decreased sense of overall competence and self-image if they feel that they are unable to effectively intervene in order to help their client/patient. Sometimes cultural and linguistic barriers may influence providers’ perception of competence. Additionally, the perceived failings providers describe may be worsened by instances when caregivers “internalize an ‘idealized image’ of the client as deserving the best treatment and outcomes” and fall short of their effort to provide high quality care (Eisenman, Bergner, & Cohen, 2000; cited Smith, Keller & Lhewa, 2007). On the other hand, “the caregiver may harbor ‘savior’ fantasies which can also erode reasonable expectations as to the probable outcomes of treatment” (Kinzie 1994; Smith 2003, cited in Smith et al. 2007; Papadopoulos 2005).
Further, although such topics did not surface in my interviews, studies show that providers may find it difficult to engage with trauma victims who are manipulative and unthankful, who inflate their trauma history in order to secure asylum status and social benefits, and/or who have themselves been perpetrators of human rights violations (Eisenman, Bergner, & Cohen 2000, Smith, Keller & Lhewa, 2007).
Stemming from the material presented above, it is without a doubt that caring for refugee/asylee patients is demanding and stressful. Thus, the discussion throughout this section has not been about whether stress is present as the result of exposure to patient trauma, but to what extent, what effect stress can have on the caregiver, and what risk factors or caregiver dispositions initiate the development of burnout, secondary traumatic stress, or vicarious trauma. At the heart of the matter, empathy is the leading and proximal cause for adverse psychological reactions in providers working in refugee/asylee care. Generally, “the more empathic a provider is, the greater the risk” (BSRC, 2012). However, this does not mean that all empathetic practitioners will experience secondary or vicarious stress or that they will terminate their practices or switch fields/specialties if they do.
The deeply emotional accounts of clinicians in my study indicated to me that they may have at one point experienced (or are experiencing) secondary traumatic stress or vicarious trauma. However, despite their exposure to highly charged traumatic patient narratives, they continue to work with this patient population. In fact, most of the stories these clinicians shared occurred fairly early in their medical careers (either during or shortly post residency). Nonetheless, these clinicians continue to care for refugees and have done so, on average, for the past twenty years. What keeps them going? After all, refugee care, as with most health care fields, is self-selected. Why do they continue to care for refugee/asylee patients if such encounters are proven to be highly distressing and traumatizing? Is it their deep sense of empathy and loyalty towards this particular patient population? What gives them the psychological and physiological endurance to continue? According to Dr. Forster, a primary care physician I interviewed,
This is what inspires me...just knowing that I could play some part in the healing process and contribute to the lives of these extraordinary individuals…it’s really the resiliency of the people I see that keeps me in awe of the human capacity to go on…
In other words, this provider draws strength from witnessing the resiliency of his patients and seeing his role in their healing process. Emerging literature describes this phenomenon as vicarious resilience. I prefer, instead, to talk about what I refer to as “secondary resilience.”
Secondary Resilience: An Antidote for Vicarious Trauma or Secondary Traumatic Stress
All humans have the capacity for resilience. Ungar (2008) provides an eloquent definition of resilience:
In the context of exposure to significant adversity, whether psychological, environmental, or both, resilience is both the capacity of individuals to navigate their way to health-sustaining resources, including opportunities to experience feelings of well-being, and a condition of the individual’s family, community and culture to provide these health resources and experiences in culturally meaningful ways (225).
In this sense, resilience is a transformational, contextual and socially constructed process rather than a static individual characteristic. Just like people who have overcome great adversity, persecution, and tragedy, caregivers who care for vulnerable populations may have the capacity to endure and process exposures to traumatic narratives and human suffering.
From a theological angle, a clinician’s willingness to enter the realm of a patient’s pain and suffering is what defines a good, empathic healer. In his theological work, The Wounded Healer, Henri Nouwen argues that “...the minister is called to recognize the sufferings of his time in his own heart and make that recognition the starting point of his service…his service will not be perceived as authentic unless it comes from a heart wounded by the suffering about which he speaks…” (xvi).
Medicine, like ministry, is about serving people. When I asked clinicians about why they entered refugee care they stated that “they recognized a need and wanted to help,” that it was “simply the right thing to do,” and that they felt “called into this ministry.” The decision to care for refugee patients also exposed these providers to vivid traumatic material. At times, such exposures made clinicians emotionally vulnerable. In essence, in the words of Nouwen, it made them “wounded” healers; healers who were “[n]ot ‘up there’ far away or [emotionally insulated] from people [in their care], but in the midst of [their patients], with the utmost visibility” (40). Partaking of their patient’s experiences through empathy, clinicians are able to understand the magnitude of distress their patients endure.
Retrospectively, this understanding is precisely what makes these clinicians sensitive and compassionate healers. For as Nouwen states, “Who can take away suffering without entering it? The great illusion of leadership is to think that man can be led out of the desert by someone who has never been there…” (72). Nonetheless, just as a refugee patient can find healing, so too can a “wounded” clinician.
There is developing evidence that contact with client/patient stories of tragedy may contribute to personal and professional perspective and development. Hernandez, Gangsei, & Engstrom (2007) suggest that psychotherapists who work with torture survivors can develop “vicarious resilience” and convert vicarious trauma into social activism. They describe vicarious resilience as the “complex array of elements contributing to the empowerment of therapists through interaction with clients’ stories of resilience” (238). Based on their interviews with 12 therapists, they grouped several of the elements that contribute to therapists’ development of vicarious resilience:
Witnessing and reflecting on human beings’ immense capacity to heal; reassessing the significance of the therapists’ own problems; incorporating spirituality as a valuable dimension in treatment; developing hope and commitment; articulating personal and professional positions regarding political violence; articulating frameworks for healing; developing tolerance to frustration; developing time, setting, and intervention boundaries that fit therapeutic intervention in context; using community interventions; and developing the use of self in therapy (238).
In this sense, “vicarious resilience is founded on the assumption that client and therapist influence each other in the therapeutic relationship” (Hernandez-Wolfe, Killian, Engstrom & Gangsei, 2014). Despite the logical ramifications of the developing vicarious resilience model, there is a shortage of literature on the subject and quantitative measurement concerning the prevalence of vicarious resilience is absent. In addition, there are no studies that have focused on the utility of vicarious resilience specifically in physicians who work with vulnerable patient groups.
Conceptually, vicarious resilience is different from and does not parallel vicarious trauma. While vicarious trauma is founded on constructivist self-development theory (Saakvitne, Gamble, Pearlman & Lev, 2000) and is measureable via the Trauma Symptom Inventory (TSI) Belief Scale, vicarious resilience developed out of observation, grounded theory, and the juxtaposition of resilience and vicarious learning theory (Bandura, 1986; Luthar, 2003, 2006; Walsh, 2006). To clarify, constructivist self-development theory asserts that individuals construct their realities and adaptations based on past and present experiences, perceptions, and circumstances (e.g. a provider who cares for refugees or torture survivors may begin to view the world as an evil, unsafe place). Vicarious learning theory implies that behaviors are learned from the social environment through observation.
Following closely with the definition of vicarious trauma, vicarious resilience develops over time. However, Hernandez-Wolfe, Killian, Engstrom & Gangsei (2014) state that it is not yet known whether or not vicarious resilience is something experienced exclusively by seasoned therapists who have had the most exposure to trauma-filled narratives. However, the physician-informants in this study suggested that critical, one-time exposures to specific refugee patients and their tragic stories allowed them to witness the resilience of their patient population and galvanized their desire to continue to care and advocate for this vulnerable, yet resilient group.
With this in mind, I introduce the concept of “secondary resilience.” Similar to vicarious resilience, “secondary resilience” can be a protective factor in and have a moderating effect on vicarious trauma. However, despite the similarity between vicarious and “secondary resilience,” they are distinct. Paralleling the definition of secondary traumatic stress, “secondary resilience” can develop immediately after a one-time exposure to a highly influential or traumatic event. In other words, this suggests that a practitioner does not have to be exposed to multiple traumatizing incidents in order to develop resiliency. Dr. Bradford, a seasoned psychiatrist and co-founder of the Center, demonstrates this phenomenon:
There was a time when a Tibetan monk…patient…told me that one of his major concerns that he had, when he was in prison and tortured, was how he could use compassion towards his torturer...such cases are awakenings...things you do not expect but must be willing to learn and process...this touched me personally and I knew that there was something special about these people, and this... really stuck with me...and guided me as I worked with other refugees... torture survivors.
Here, Dr. Bradford reflects on the effect one Tibetan monk patient had on him. The Tibetan monk’s concern with “showing compassion towards his torturer” served as an “awakening” for Dr. Bradford. The shock associated with the unexpected and paradoxical nature of the monk’s words influenced Dr. Bradford’s perception and understanding of these “special” people. As he says, “it touched” him, “it stuck with” him, and “guided” him in his future encounters with patients from that region and culture.
Furthermore, both vicarious resilience and secondary resilience can function on a continuum. Resilience can be built either after one exposure or after long-term exposure to a trauma-inducing event(s). Nonetheless, “secondary resilience” does not suggest that vicarious or secondary traumatic stress is absent. In fact, because practitioners recounted a specific incident with a patient early on in their careers (during residency or soon after) and had deeply emotional responses during the interview (about 10-20 years after the incident), this shows the possibility that vicarious trauma may coexist with vicarious or secondary resilience.
Despite the many identified elements that bolster providers’ potential to transition from vicarious trauma to a state of vicarious or secondary resilience, there is disconnect between how this process occurs. Because some of my physician-informants shared very specific accounts, they took meaning from first-time incidents. These incidents changed providers’ perspectives, attitudes, and approaches to refugee/asylee care. Although such incidents produced raw emotional responses, these tragedy-filled incidents were learning experiences for my informants. Notwithstanding the unsettling nature of witnessing patient suffering and listening to traumatic narratives, my informants did not dwell on or remain in a state of vicarious trauma. They were able to process these incidents as tragic yet inspiring stories that showed them the resilience of their refugee patients and gave them motivation and a sense of calling to dedicate their lives to the care of refugee communities. In this vein, I argue that the constructive link between vicarious or secondary traumatic stress and vicarious or secondary resilience is providers’ ability to process, evaluate, and learn from critical incidents.
Critical Incidents: Bridging Trauma & Resilience
Branch (2005) defines critical incidents as the “short narrative accounts focusing on the most important professional experiences of medical students, residents, and other learners” (1063). Frequently,“critical incidents deliver the raw materials of key nodal points of experience” (Branch, 2005). Physicians’ narratives of clinical critical incidents have experiential and psychological value in medical education and training (Branch, 2005; Brady, Corbie-Smith & Branch, 2002; Bradley, 1992; Flanagan, 1954).
Critical incident reporting allows professionals to process and make meaning of subjective, existential material that can be highly influential, emotionally vested, and in conflict with a person’s morals, attitudes, and values. Generally, critical incident reporting is considered an effective method to focus on the ethical, emotional, and professional aspects of becoming a medical practitioner. Evidence shows that critical incident reports are used widely in medical and nursing education curricula (Branch, Pels, Lawrence & Arky, 1993; Brady, Corbie-Smith, & Branch, 2002; Hupert, Pels, & Branch, 1995; Branch, Pels & Calkins, 1995; Branch, Hafler, & Pels, 1998; Lichstein & Young, 1996; Niemi, 1997; Svahn, 2002; Baernstein & Fryer-Edwards, 2003; Locke, 2003; McDonannell-Baum, 1998; Ta, 1997; Parker, Webb & D’Souza, 1995).
Appraisal of critical incidents bolsters the value of experiential learning and facilitates the expansion of the empathic self and the development of the professional self. In certain cases, evaluation of critical incidents can “solidify or reawaken values in an environment where they are being challenged” (Branch, 2005). This is especially important during periods when medical practitioners experience high stress levels, uncertainty, sleep-deprivation, vicarious or secondary trauma, or burnout. The following example, shared by a second-year resident, paints a vivid image of why evaluation and open discussion of critical incidents is crucial for the development of secondary resilience and the reaffirmation of empathy:
When I was in the MICU, I was called by cross-cover to evaluate a patient for transfer. She had a slightly altered mental status and was hypotensive . . . We were giving her fluids, blood, pressors; it was around midnight. I got another admission and went to the ER to start seeing him. The first patient coded, and I went to take care of her again. It was a terrible, endless, isolated night. I went back to the ER to see the new admission, and another code was called. I went to that. I was the only resident who responded. The patient died . . .
The next morning on rounds, my attending asked me how many had survived. He said we didn’t need to talk about any that had died . . . It was a hellish night of nearly unbearable stress and in the morning it was never acknowledged, as if it had never happened, as if my patients had never existed . . . What bothers me most about it was that I felt completely flat. They were dead and I didn’t feel anything at all (Brady, Corbie-Smith, & Branch 2002, cited in Branch, 2005).
Contrary to contemporary medical education that emphasizes emotional neutrality, this resident is concerned that she did not feel anything. Interestingly, the resident did control her emotions and maintained her emotional neutrality by not talking about the patient deaths with the attending, but she felt that emotion should be there; that feeling emotions would be the natural human response given the nightmarish experience she went through the night before. As Branch (2005) suggests, this resident may have been close to burnout. Further, Branch (2005) recommends that focus group discussion of such critical incidents could be crucial for the resident to receive affirmation from her colleagues that she is a responsible and caring physician and that she is not alone in such experiences. In this sense, processing critical incident at the individual or group level can reframe and reconstruct experiences from “negative” to “positive” or from trauma to resilience.
In my own research, I have been privileged to hear critical incident accounts from each of my informants. Every story is a transformative, “awakening” for physicians I interviewed. If we recall Dr. Lindquist’s powerful story about her clinical critical incident with an asylee woman and her little boy, we can see that witnessing her patient experience a flashback invoked, in Dr. Lindquist, deep empathy and a strong emotional response. However, despite the emotional and potentially traumatizing critical incident Dr. Lindquist shared, she was able to bring herself into composure and focus on the resiliency of her patient. The ability of Dr. Lindquist to move from tears to a discussion of resilience and the rewarding nature of her work indicates that she may have developed “secondary resilience” after processing a singular critical incident with this asylee woman and her infant boy. In other words, Dr. Lindquist actively transformed her raw emotions into a tangible realization that she has the knowledge and skills to have a positive impact on the lives of her patients. In this sense, Dr. Lindquist’s narrative is not just a depiction of empathy as an emotion or feeling, but is a reflection of how she sees herself as a person and physician. Dr. Lindquist recognizes her role, or rather, her own agency in the lives of her patients. Rather than wallowing in her emotions, Dr. Lindquist can do something about it. This transformation in perception allows Dr. Lindquist to view herself as an agent, advocate, and a caregiver for individuals who survive the atrocities of this world. This is secondary resilience at its best.
Nonetheless, soon after this moving narrative, Dr. Lindquist vocalized that sometimes she found herself “living on the edge” – a kind of living that borders being both emotionally vulnerable and resilient. This statement and Dr. Lindquist’s emotional response during the interview may indicate that despite her development of “secondary resilience,” vicarious trauma may still exist. These realities point to the coexistence of secondary traumatic stress and/or vicarious trauma and secondary/vicarious resilience. With this in mind, neither secondary nor vicarious resilience is unidirectional. Just because someone is resilient, it does not guarantee that he or she is emotionally insulated from incidents of similar nature.
In another interview, Dr. Forster, a primary care physician, had a similar emotional response. However, Dr. Forster’s discussion depicts his struggle with maintaining emotional neutrality, addressing his patients’ cathartic moments, and “falling short” or not knowing how to handle his personal response to patient traumatic narratives. In many ways, the physician’s narrative is a mirroring of the emotional response of his patients, quite similar to the concordance between PTSD and vicarious trauma.
...maybe certain memories can trigger sadness (in refugee patients), that's a little bit more complicated, maybe in at least some situations that's OK, if it allows someone to feel and to speak and not to be silent about something and ultimately would be better off coming out, so but in both cases, whether it be anxiety, PTSD-like trigger - a trigger to something like PTSD or to something more like sadness but that is directly behind that (PTSD), I hope that any clinician would do the same, they can see eyes watering (of the patient), and see the message...and I suppose that particularly in the latter case, you know when that's an indication to get on with other things, that the discussion or conversation should continue along those lines or be put off to some other time or terminated, I'm sure it's not all bad or at least not always be avoided so it might... how do you...I don't know the answer to this...I going to fall short here but...when somebody's sadness is part of some therapeutic process and when is it just experiences of redundant pain that doesn't serve any purpose? You know, if they're crying every other week and they have been having a good week, why mess up that week? On the other hand, if they've been numbed to the world for the past six months and they may be on the verge of being able to be more alive or sensate, may that's a useful process...and I think that's the toughest thing actually ...[doctor's eyes began to fill with tears]...again I feel that I'm falling short here, I really have to go by instinct, and I have no way of knowing if my instincts are right...you know... there are so many amazing short stories...[tears pour down doctor's face, takes off glasses to dry his eyes]...(silence)....(brief laugh to himself as he regains composure)…
Comparatively, Dr. Lindquist was able to finish telling her critical incident, while Dr. Forster’s attempt to share a critical incident resulted in a self-reflective rumination that led up to a cathartic silence. Both reflected expressions of their compassion and vulnerability to refugee stories.
Additionally, because the physician reflected on his ambivalence to attend to the emotions of patients, this may indicate his deep empathetic desire to help his patients but at the same time shows his uncertainty about acting upon this desire knowing that patients may not want to return to the horrifying stories of their past. On the other hand, if Dr. Forster is struggling with vicarious trauma, he may prefer what Baranowsky (2002) calls “the silencing response.” This type of response refers to the caregiver’s inability to listen and attend to the narratives or experiences of patients/clients by sidestepping to less distressing or traumatic material. In some cases, both the patient and the provider may avoid discussion of painful or uncomfortable information (Hesse, 2002). Holmqvist & Anderson, (2003) described this type of avoidance as “collusive resistance” (294).
Furthermore, although Dr. Forster was unable to share a particular incident, this does not mean that he has not developed vicarious or secondary resilience caring for refugee patients. Later in the interview, Dr. Forster’s statement reveals that he has converted or processed raw emotions born from critical incidents into a realization that tragedy and suffering is inevitable in his line of work. In other words, similar to Dr. Lindquist, Dr. Forster is a resilient provider who draws strength from knowing that his expertise has a positive impact on his patients. He continues,
Just by entering medicine, by default, I learned that I will be exposed to tragedy and suffering…in a general sense, suffering - it’s universal in medicine, it’s unavoidable…but what really resonates with me are stories that patients tell, stories of resiliency and hope, stories in which people have lost everything…stories about people who have seen their brothers, sisters, mothers, fathers killed, people who have a deep sense of guilt that they could have saved their family from harm, people who have been shot, maimed and yet still decide to return to areas of civil strife to fight for liberty…and after having gone through such tragedies these people find a thread of hope to thrive and to start life anew. This is what inspires me…just knowing that I could play some part in the healing process and contribute to the lives of these extraordinary individuals…it’s really the resiliency of the people I see that keeps me in awe of the human capacity to go on…
In the words of this doctor, we see a similar statement to that of Dr. Lindquist’s. Dr. Forster draws inspiration from witnessing the resilience of his patients and recognizes his agency “in the healing process.” Dr. Forster did not dwell on his emotions but moved to a discussion of his patients’ resiliency and his role in their lives. This is precisely what makes him an empathetic and resilient provider.
From another perspective, Dr. Forster’s resiliency is not only demonstrated in his words but also in his long-term commitment to this patient population. He has cared for refugee and asylee patients for over a decade and articulates that it is an honor and privilege to serve this patient population. Likewise, because this practitioner had such a strong emotional response, this, yet again, indicates that vicarious or secondary trauma may coexist with either vicarious or secondary resilience. Dr. Forster’s unsaid critical incident, the bare silence and tears, tells a story of compassion, but also exhibits the “symptoms” of burnout and vicarious trauma in tandem with resiliency and deep loyalty to his patients.
These said and unsaid "critical incidents" have molded each clinician’s disposition towards patients and his or her approach to care. My informants’ emotionally vested clinical experiences helped them to acquire knowledge, skills, motivation, attitudes, and sensitivity. All in all, my physician-informants mirror the resiliency of their patients and become advocates for those who flee their homeland to escape political violence, torture, persecution, and death.
Conclusion
Caring for refugees can have psychological and physiological repercussions for physicians. Exposure to trauma narratives and vivid examples of human suffering can undermine physicians’ ability to maintain emotional neutrality and can lead to burnout, vicarious trauma, or secondary traumatic stress.
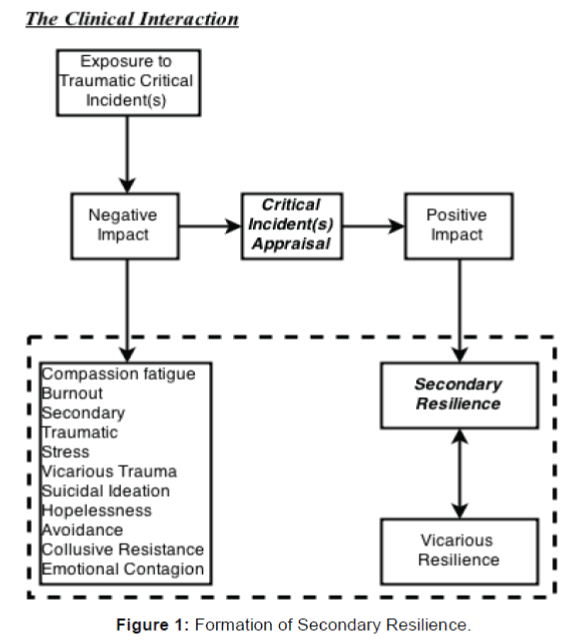
However, emerging literature indicates that providers may be able to develop vicarious resilience by mirroring the resiliency of their patients. Provider resiliency has the potential to transition into social advocacy. Aligning with this growing theory, I have argued that providers can develop “secondary resilience” after a single exposure to a critical incident, that critical incident(s) appraisal is the link between vicarious trauma and secondary or vicarious resilience, and, as signified by the dotted box housing the lower box and the two resilience boxes, that secondary or vicarious resilience can coexist with vicarious trauma or secondary traumatic stress and their related synonyms. The following flowchart depicts these processes (Figure 1).
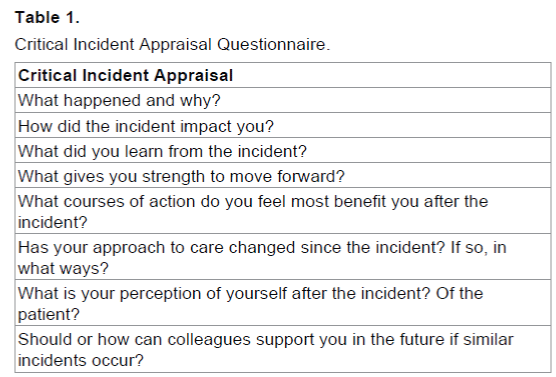
Moreover, critical incident appraisal is especially important considering that vicarious trauma and secondary traumatic stress is understudied in refugee physician practices. Reconciliation of critical incidents may be instrumental for psychological conflict resolution and for the solidification of vicarious or secondary resilience among providers who work in challenging areas. Although there is an abundance of literature on the utility of critical incidents in medical education, this literature does not provide explicit models for critical incident assessment. One way to reconcile critical incidents is through self-reflective or group discussion questionnaires. The questions shown in the Table 1 below may be useful for effective critical incident appraisal.
Furthermore, studies show that approximately four hundred physicians commit suicide each year (Andrew, 2014). Some of the potential factors that contribute to suicidal ideation are burnout, depression, secondary traumatic stress, and vicarious trauma stemming from critical incidents (Shanafelt, Sloan, & Habermann, 2003; Shanafelt et al. 2011; Andrew, 2014). Considering that an average primary-care physician sees about 2,300 patients annually, this means that about one million Americans will lose a physician to suicide this year (Altschuler, Margolius, Bodenheimer & Grumbach, 2012). With this in mind, the impact of physician suicide on public health is paramount and warrants further study. One potential approach to mitigate this loss of lives is through critical incident appraisal. This may not be the panacea, but it might be a crucial building block for bolstering physician resilience.
Additionally, as the Affordable Care Act brings approximately 30 million previously uninsured U.S. residents into publicly funded health systems, case-loads as well as stress levels are sure to rise and we need to know from what sources physicians gain psychological and physical stamina. This knowledge may prove pivotal in how policy makers and healthcare organizations help physicians to work effectively, unencumbered by burnout, vicarious trauma or secondary traumatic stress. In addition, those physicians who work in the context of refugee/asylee care may need practice-based support systems, support-focused CME, and patient-population-specific training in medical school or residency programs. To start, however, it may be wise to focus on the processing and transformation of trauma and stress, so that “secondary resilience” produces “unencumbered” physicians in the midst of traumatizing situations.
In order to create the most effective preventive and interventional approaches to mitigate psychological strain at the individual and systemic levels, the proposed questionnaire and the effect of critical incidents on the transition from vicarious trauma/secondary traumatic stress to secondary or vicarious resilience should be validated quantitatively across multiple medical sub-fields.
Ultimately, although it may not be possible to eradicate the distress associated with caring for vulnerable populations, it may be mitigated through self-reflection, gaining satisfaction from small gains with patients, and focusing on the resilience of the people being served. Perhaps one of the most important takeaways from this study is that there should be no shame or stigma in experiencing burnout, vicarious trauma, or secondary traumatic stress. Without empathy and without compassion for people, medicine would be a voyeuristic practice engulfed in a personal pursuit of prestige, financial gain, and intellectual arrogance.
References
- Altschuler, J., Margolius, D., Bodenheimer, T., & Grumbach, K. (2012). Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. The Annals of Family Medicine, 10(5), 396-400
- Andrew, L. (2014). Physician Suicide (B. Brenner, Edn.) Retrieved May 1, 2015, from http://emedicine.medscape.com/article/806779-overview
- Baernstein, A. & Fryer-Edwards, K. (2003) Promoting reflection on professionalism: a comparison trial of educational interventions for medical students. Academic Medicine, 78, 742–747
- Baird, C. & Kracen, A.C. (2006). Vicarious traumatization and secondary traumatic stress: A research synthesis. Counselling Psychology Quarterly, 19(2), 181-188.
- Bandura, A. (1986). Social foundations of thought and action (pp. 5-107). Prentice Hall.: Englewood Cliffs, NJ
- Baranowsky, A.B. (2002). The silencing response in clinical practice. In C.R. Figley (Ed.), Treating compassion fatigue. New York: Brunner-Routledge
- Bernard, H.R. (2011). Research methods in anthropology. Rowman Altamira
- Best Start Resource Centre (BSRC). (2012). When Compassion Hurts: Burnout, Vicarious Trauma and Secondary Trauma in Prenatal and Early Childhood Service Providers. Toronto, Ontario, Canada
- Bradley, C.P. (1992) Turning anecdotes into data-the critical incident technique. Family Practice, 9(1), 98-103.
- Brady, D.W., Corbie-Smith, G., & Branch, W.T. Jr. (2002) ‘‘What’s important to you?’’: the use of narratives to promote self-reflection and to understand the experiences of medical residents. Annals of Internal Medicine, 137, 220–223
- Branch, W.T. (2000). Supporting the moral development of medical students. Journal of general internal medicine, 15(7), 503-508
- Branch, W.T. (2005). Use of critical incident reports in medical education. Journal of general internal medicine, 20(11), 1063-1067
- Branch, W.T. Jr., Hafler, J.P., & Pels, R.J. (1998) Medical students development of empathic understanding of their patients. Academic Medicine, 73, 361-362
- Branch, W.T. Jr., Pels, R.F., Harper, G., Calkins, D., Forrow, L., Mandell, F., et al. (1995) A new educational approach for supporting the professional development of third year medical students. The Journal of General Internal Medicine, 10, 691-694
- Branch, W.T. Jr., Pels, R.J., Lawrence, R.S., & Arky, R.A. (1993) Becoming a doctor: ‘‘critical-incident’’ reports from third-year medical students. The New England Journal of Medicine, 329, 130-132
- Bryman, A. (2003). Quantity and quality in social research, Routledge
- Dey, I. (2003). Qualitative data analysis: A user friendly guide for social scientists, Routledge
- Eisenman, D., Bergner, S., & Cohen, I. (2000). An ideal victim: Idealizing trauma victims causes traumatic stress in human rights workers. Human Rights Review, 1(3), 106-114
- Figley, C. (1995a). Compassion fatigue as secondary traumatic stress disorder. In C. Figley (Ed.), Compassion fatigue: Coping with traumatic stress disorder in those who treat the traumatized (pp. 1-18). New York: Bruner/Mazel, Inc
- Figley, C.R. (1995b). Compassion fatigue: Coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner/Mazel
- Figley, C.R., & Kleber, R.J. (1995). Beyond the “victim”. In Beyond trauma (pp. 75-98). Springer US
- Flanagan, J.C. 1954. The critical incident technique. Psychological bulletin, 51(4).
- Halpern, J. (2001) From Detached Concern to Empathy: Humanizing Medical Practice. New York: Oxford University Press
- Harding, J. (2013). Qualitative data analysis from start to finish. Sage
- Hernández, P., Gangsei, D., & Engstrom, D. (2007). Vicarious resilience: A new concept in work with those who survive trauma. Family process, 46(2), 229-241
- Hernandez-Wolfe, P., Killian, K., Engstrom, D., & Gangsei, D. (2014). Vicarious Resilience, Vicarious Trauma, and Awareness of Equity in Trauma Work. Journal of Humanistic Psychology, 0022167814534322
- Hesse, A.R. (2002). Secondary trauma: How working with trauma survivors affects therapists. Clinical Social Work Journal, 30(3), 293-309
- Holmqvist, R., & Andersen, K. (2003). Therapists’ reactions to treatment of survivors of political torture. Professional Psychology: Research & Practice, 34(3), 294-300
- Hupert, N., Pels, R.J., & Branch, W.T. Jr. (1995). Learning the art of doctoring: use of critical incident reports. Harvard Student BMJ; 3, 99-100
- Joinson, C. (1992). Coping with compassion fatigue. Nursing, 22(4), 116-122
- Kinzie, J. (2001). Psychotherapy for massively traumatized refugees: The therapist variable. Portland: Oregon Health and Sciences University
- Kolb, D.A. (1984). Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice Hall
- Lichstein, P.R., & Young, G. (1996) ‘‘My most meaningful patient.’’ Reflective learning on a general medicine service. Journal of General Internal Medicine, 11406–11409
- Locke S. (2003) Controversies. Interview with Gordon Harper. Medical Encounter, 17, 17–21
- Luthar, S.S. (2006). Resilience in development: A synthesis of research across five decades.
- Luthar, S.S. (Edn.). (2003). Resilience and vulnerability: Adaptation in the context of childhood adversities. Cambridge University Press
- Mann, T., & Woods, J.E. (1995). The magic mountain: A novel. New York: A. Knopf
- Marcum, J.A. (2008). An introductory philosophy of medicine: Humanizing modern medicine. Springer, 99
- Maslach, C., & Jackson, S.E. (1981). The measurement of experienced burnout. Journal of Occupational Behavior, 2, 99 113
- McDonannell-Baum, B. (1998). Dilemmas in nursing care: a student’s reflection of a critical incident. Contemporary Nurse, 7, 32-34
- Miller, K.I., Stiff, J.B., & Ellis, B.H. (1988). Communication and empathy as precursors to burnout among human service workers. Communication Monographs, 55(9), 336-341
- Mitchell, J. T., & Bray, G. (1990). Emergency services stress: Guidelines for preserving the health and careers of emergency services personnel. Ellicott City, MD: Chevron Publishing Corporation
- More, E.S. (1996). Empathy as a hermeneutic practice. Theoretical Medicine, 17(3), 243-254
- Niemi, P.M. (1997). Medical students’ professional identity: self-reflection during the preclinical years. Medical Education, 31, 408-415
- Papadopoulos, R.K. (Edn.). (2005). Therapeutic care for refugees: No place like home. London:Karnac
- Parker, D.L., Webb, J., & D’Souza, B. (1995) The value of critical incident analysis as an educational and its relationship to experiential learning. Nurse Education Today, 15, 111-116
- Perry, B.D, Conroy, L., & Ravitz, A. (1991). Persisting psychophysiological effects of traumatic stress: The memory of “states”. Violence Update, 1(8), 1-11, From the Child Trauma Academy. Retrieved from:www.childtrauma.org/ctamaterials/memory_states.asp
- Pines, A., & Aronson, E. (1988). Career burnout: Causes and cures. Free press
- Saakvitne, K.W., Gamble, S., Pearlman, L., & Lev, B. (2000). Risking connection: A training curriculum for working with survivors of childhood abuse. Lutherville, MD: Sidran Press
- Saldaña, J. (2012). The coding manual for qualitative researchers, Sage, 14
- Shanafelt, T.D., Balch, C.M., Dyrbye, L., Bechamps, G., Russell, T., Satele, D., et al. (2011). Special report: suicidal ideation among American surgeons. Archives of surgery, 146(1), 54-62
- Shanafelt, T.D., Sloan, J.A., & Habermann, T.M. (2003). The well-being of physicians. American Journal of Medicine, 114(6), 513-519
- Smith, H.E., Keller, A.S., & Lhewa,D.W. (2007). “…Like A Refugee Camp On First Avenue”- Insights And Experiences From The Bellevue: NYU Program For Survivors Of Torture
- Svahn, D.S. (2002). Let Me Listen to Your Heart. Writings by Medical Students, Collected by Alan J. Kozak. New York: Bassett Healthcare
- Ta, L. (1997). Critical incident analysis: nursing a dying man. Contemporary Nurse, 6, 72-74
- Trippany, R., White, V., & Wilcoxon, S. (2004). Preventing Vicarious Trauma: What Counselors Should Know When Working With Trauma Survivors. Journal of Counseling and Development, 82(1), 31-37
- Ungar, M. (2008). Resilience across cultures. British journal of social work, 38 (2), 218-235.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11756
- [From(publication date):
specialissue-2015 - Sep 01, 2025] - Breakdown by view type
- HTML page views : 10777
- PDF downloads : 979