Case Report Open Access
Novel Therapy for Unresectable Hilar Cholangiocarcinoma ‘Klatskin Tumor’ Utilizing Percutaneous Irreversible Electroporation: A Case Report
Mazal N1* and West D1,21Department of Diagnostic and Interventional Imaging, The University of Texas Health Science Center, Houston, USA
2Department of Nanomedicine and Bioengineering, The University of Texas Health Sciences, Houston, USA
- *Corresponding Author:
- Nicolas Mazal
Department of Diagnostic and Interventional Imaging
The University of Texas Health Science Center
Houston, USA
Tel: 7135007700
Fax: 7135007639
E-mail: nicolas.j.mazal@uth.tmc.edu
Received Date: March 28, 2017; Accepted Date: April 06, 2017; Published Date: April 12, 2017
Citation: Mazal N, West D (2017) Novel Therapy for Unresectable Hilar Cholangiocarcinoma ‘Klatskin Tumor’ Utilizing Percutaneous Irreversible Electroporation: A Case Report. OMICS J Radiol 6:258. doi: 10.4172/2167-7964.1000258
Copyright: © 2017 Mazal N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Unresectable hilar cholangiocarcinoma ‘Klatskin Tumor’ is a rare malignancy with limited treatment options and an overall poor prognosis. Percutaneous Irreversible Electroporation (IRE) is a relatively new ablative procedure with potential for treating unresectable cholangiocarcinoma, improving morbidity, and ultimately prolonging survival. The main benefit of IRE relies in the non-thermal technology which can be considered in patients with hilar tumors given the criticality of the adjacent vessels and bile ducts. This case report describes a 71 year old female with unresectable Bismuth-Corlette Stage IV cholangiocarcinoma who underwent IRE with disease control 13 months after treatment.
Keywords
Irreversible electroporation; Cholangiocarcinoma; Klatskin tumor; Tumor ablation; Percutaneous ablation
Introduction
Cholangiocarcinoma is the 2nd most common primary hepatic malignancy with an incidence in the United States ranging from 0.4- 0.9/100,000 with 5 year survival estimated at 2.6-4.4% [1]. The average age at diagnosis of cholangiocarcinoma is 50 years old with curative options including surgical resection, neoadjuvant chemoradiation, and liver transplantation [2]. Staging is based on anatomic location in accordance with Bismuth–Corlette staging classification used for perihilar tumors. Given most tumors, remain asymptomatic until later stages surgical resection is often unavailable which further decreases prognosis. For unresectable tumors, treatment is limited to chemoradiation and stenting for palliation of obstructive symptoms. Given these limitations, alternative treatment options and therapies need to be considered.
One such method currently described in the literature is Irreversible Electroporation (IRE). Percutaneous irreversible electroporation is a cutting edge method which delivers short high-voltage electric pulses to create pores in the cell’s lipid bilayer and induces cell death while sparing adjacent vessels and bile ducts [3]. Given the unresectable nature of this patient’s tumor IRE allowed locoregional ablative therapy to whom otherwise would only have the option to receive chemoradiation. The unique ability of IRE allows preservation of adjacent vessels/bile ducts while maintaining the ability to induce tumoral cell death independent of any heat or cold-sink effect. Heat and/or cold sink in addition to damaging adjacent structures are the main limiting factors in current thermal ablative methods [4]. While the current data is preliminary IRE shows promising results for treatment of pancreatic, hepatic, and renal malignancies with the most significant benefit seen in patients with pancreatic malignancies [3].
Case Study
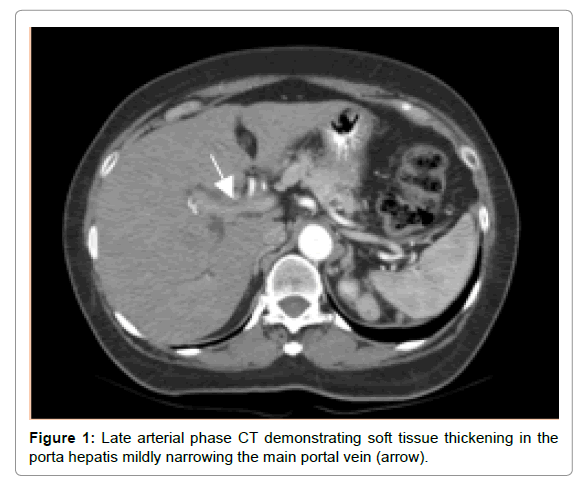
A 71-year-old female with obstructive jaundice, weight, loss, and low energy presented to our institution for evaluation. Initial laboratory studies demonstrated total bilirubin of 21.5 mg/dL. Triphasic liver protocol computed tomography (CT) demonstrated a 1.5 cm hilar mass encasing the right and left portal veins/hepatic ducts, compatible with stage IV cholangiocarcinoma. Based on type IV classification (Bismuth-Corlette staging) of the tumor, it was deemed unresectable by the transplant team (Figure 1).
Patient initially underwent endoscopic placement of a left sided plastic internal biliary stent. However, a right-sided biliary stent was not endoscopically placed secondary to tight strictures within right hepatic bile duct. Subsequently, the patient was referred to Interventional Radiology (IR) for right sided biliary stenting and to evaluate for percutaneous ablative therapy. IR then performed Percutaneous Transhepatic Cholangiography (PTC) with right sided internal-external biliary drain placement and chest port placement. Following PTC the patient’s lab values were as follows: ALP: 316 unit/L, ALT: 49 unit/L, AST: 80 unit/L, and total bilirubin 11.0 mg/dL.
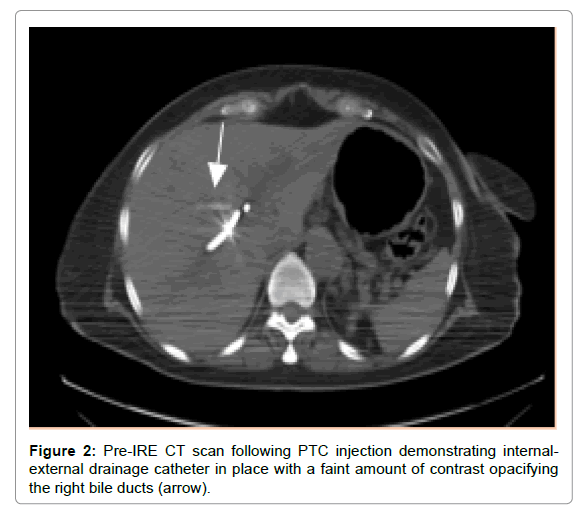
Three months following diagnosis the patient underwent IRE. To completely visualize the biliary system and the extent of intra-luminal tumor, the patient was first brought to the fluoroscopy suite. Dilute contrast was infused under fluoroscopic observation into the right sided internal external biliary drain. Contrast was seen in the internal and external biliary systems. The patient was then moved to the CT suite (Figure 2).
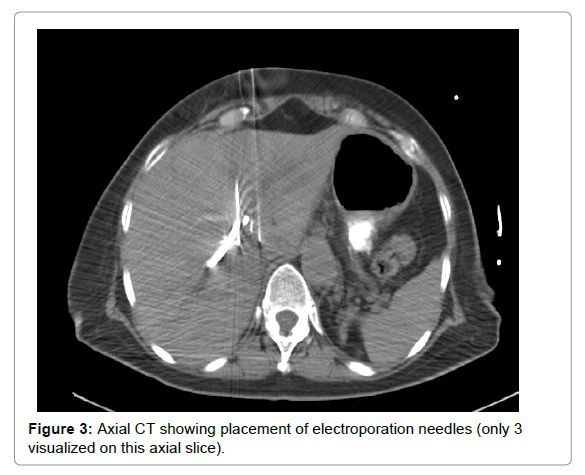
After intubation and sedation by general anesthesia, percutaneous needle routes of access were determined. Subsequently, six 18-gauge unipolar electroporation needles were guided into the hilar liver parenchyma and biliary ducts that demonstrated significant tumor involvement (Figure 3).
Under medically induced paralysis, a clinical electroporator was used to administer 90 pulses of 1300 Volts per centimeter to each paired combination between the implanted needles. After IRE, the patient recovered and was subsequently discharged without significant complication. On discharge, the patient was started on Xeloda (capecitabine) 100 mg by mouth twice daily.
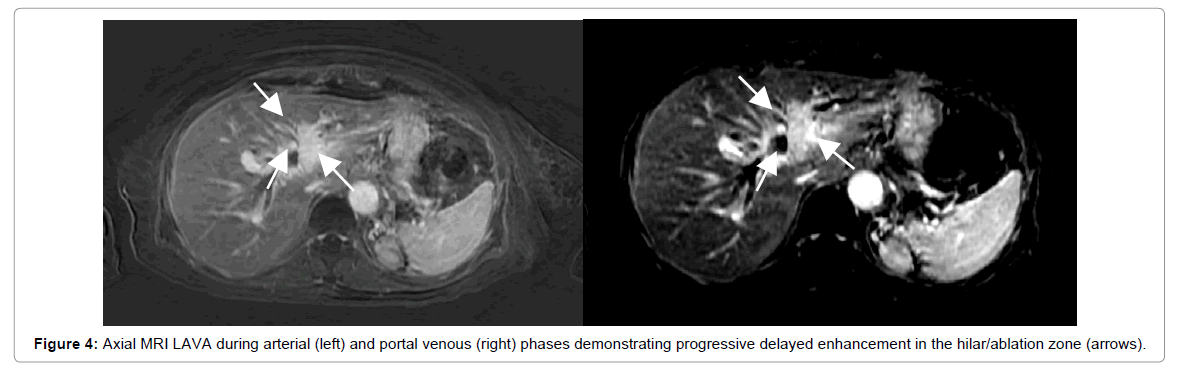
Two months following IRE patient’s total bilirubin continued to trend down 1.4 mg/dL. MRI imaging showed stable disease at 4 months (Figure 4).
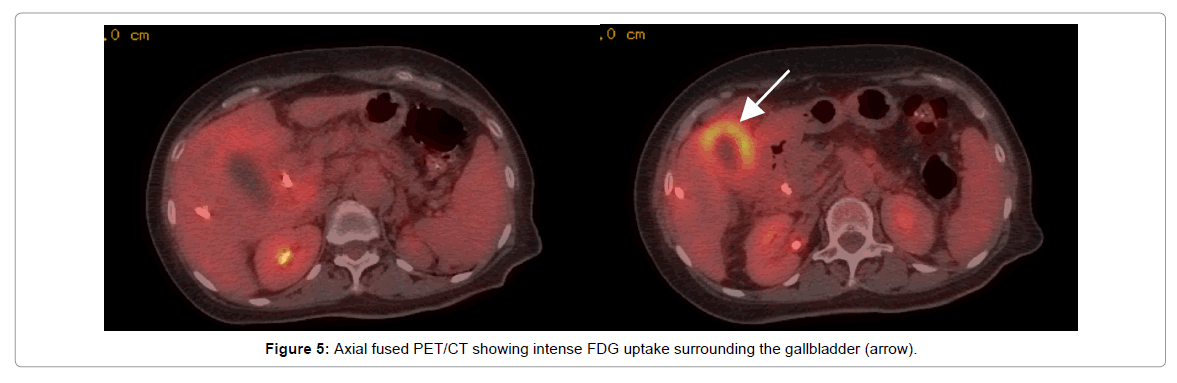
PET/CT five months after diagnosis (two months after IRE) demonstrated minimal/no FDG uptake at IRE site/hilum, but intense uptake was seen surrounding the gallbladder concerning for residual tumor versus inflammation/infection (Figure 5).
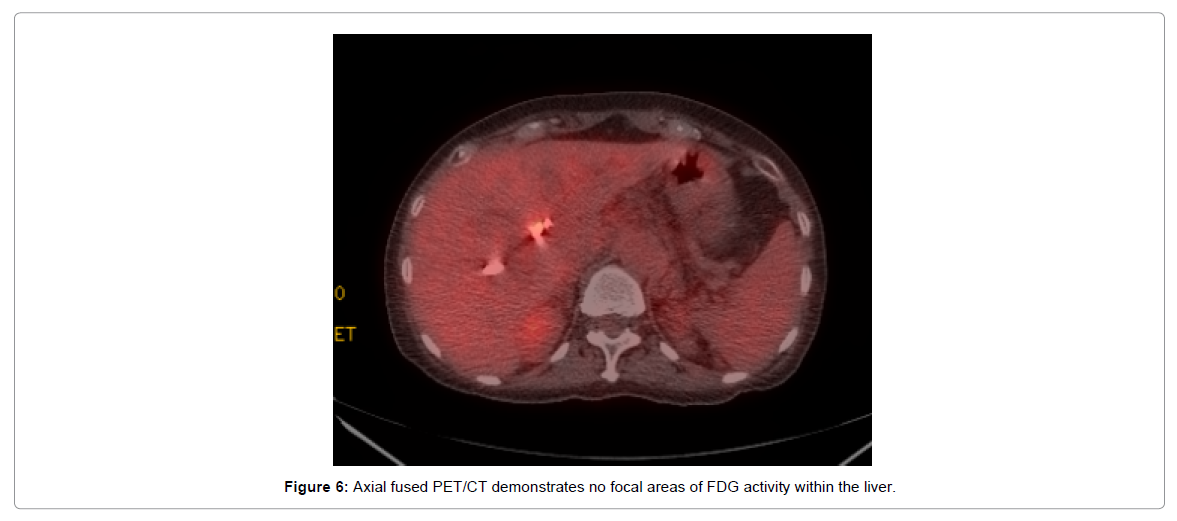
At that time the patient underwent intensity-modulated radiation using 6 MV photons and Varian Trilogy linear accelerator for a total of 50.4 Gy in 28 fractions, with a field reduction performed after 45 Gy with concurrent infusion of 5-Fluorouracil at 250 mg/m2 daily. Follow up PET/CT ten months after diagnosis showed interval resolution FDG avidity throughout the liver consistent with complete response to treatment (Figure 6).
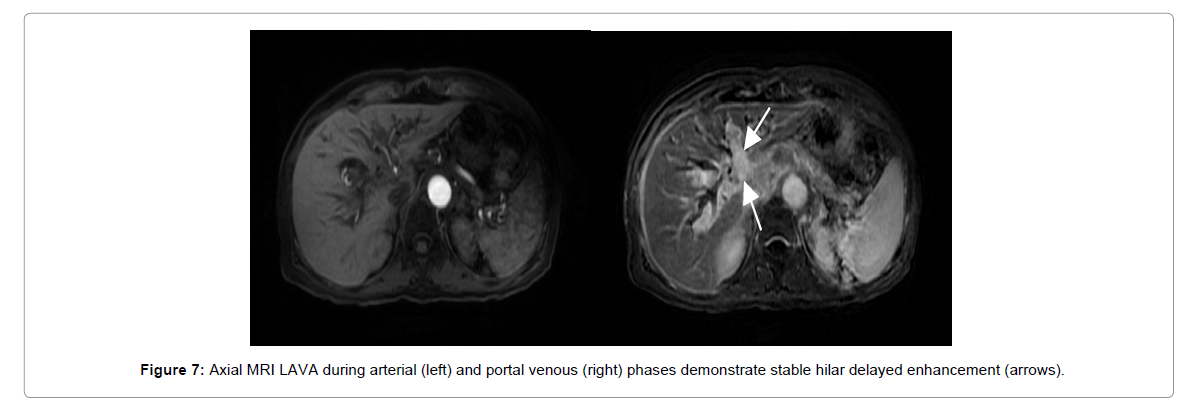
Approximately, one year after diagnosis repeat MRI continued to demonstrate stable hilar cholangiocarcinoma with treatment changes related to IRE/radiation; however, continued delayed enhancement (similar to MRI 6 months prior) (Figure 7) which remained indeterminate for residual disease.
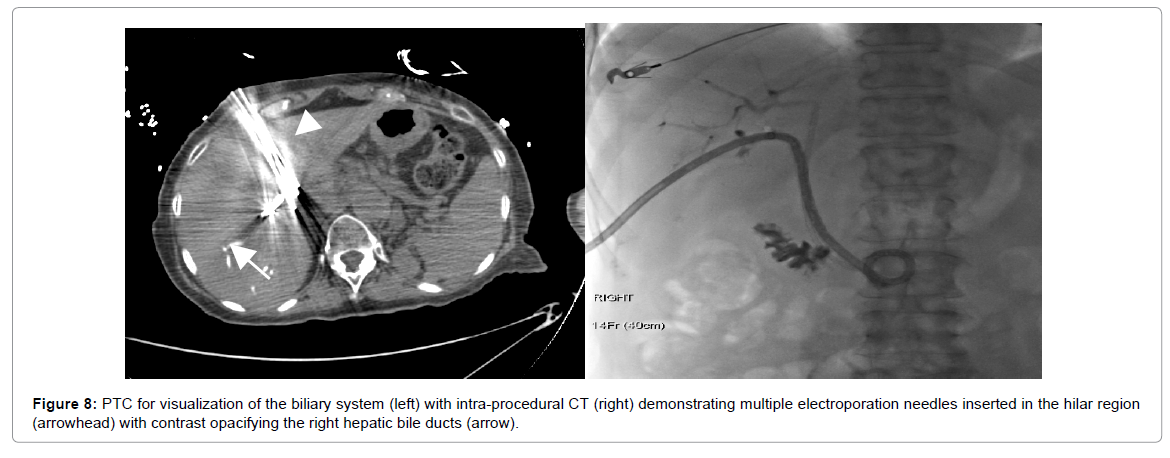
The patient underwent a second IRE ablation with the same parameters set forth in the first treatment course (Figure 8).
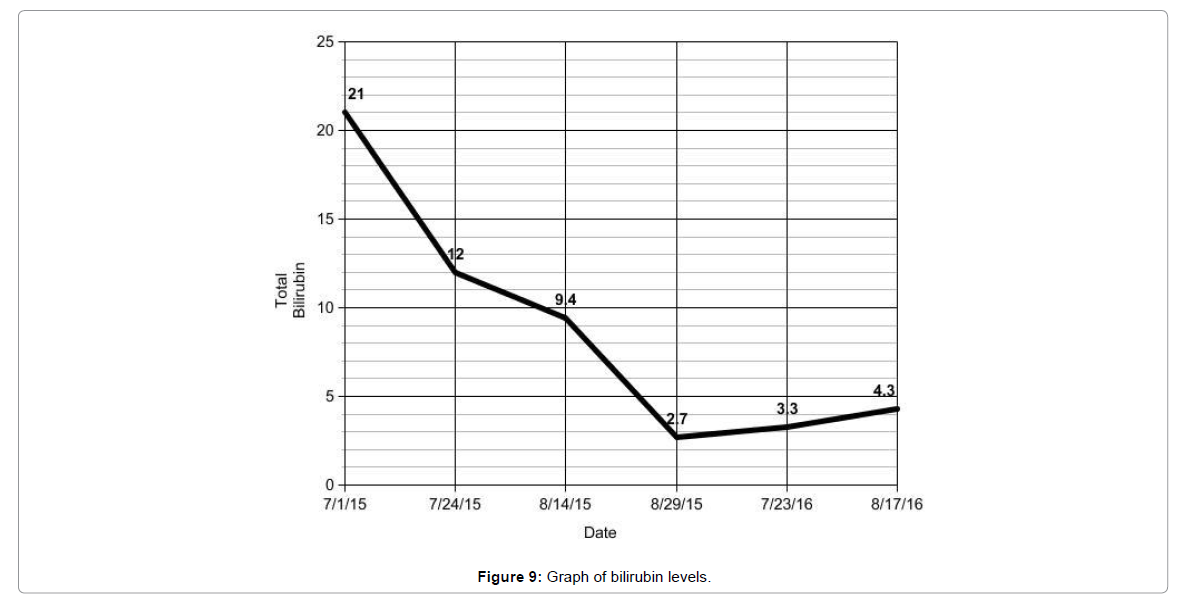
The repeat IRE one year after diagnosis was complicated by a moderate sized postprocedural subcapsular hematoma. The hematoma which was likely a result of electrode placement was drained and there were no further sequelae from the hematoma. Patient was then hospitalized for pain, low grade fever (100.4 F), and up trending white blood cell count (22,000) all of which subsequently resolved. The bilirubin reached a nadir at 2.7 mg/dL and remained stable afterwards through 13 months post follow up (Figure 9). The patient’s overall condition gradually improved and continues to follow with our multidisciplinary team.
Discussion
Cholangiocarcinoma although a relatively rare malignancy portends a poor prognosis especially in patients declared unresectable. Unfortunately, due to the late presentation less than 50% of patients at presentation are surgical candidates limiting the patient to chemotherapy and/or radiation therapy. Patients with unresectable cholangiocarcinoma undergoing chemotherapy alone (cisplatingemcitabine combination) in one study achieved a median overall survival of 11.7 months and a median progression free survival of 8 months [5,6]. External beam radiation alone has been studied as a palliative measure for biliary decompression has shown modest survival benefit at 1 and 2 years (36% and 5.2 %) versus no therapy (19% and 4.7%) [7]. The data for a combination of chemotherapy and radiation has shown mixed results thus far and is another potential area which could be further studied [8].
This case report discusses our experience in a patient with an unresectable hilar cholangiocarcinoma with the main purpose aimed at encouraging further scientific clinical examination of IRE as a potentially viable treatment option in patients with unresectable cholangiocarcinoma. In our technique, we injected dilute contrast into the biliary system to delineate the amount of intraluminal tumor burden. Using this, we were able to visualize intraluminal targets for needle placement under CT. In this particular case, the patient has far outlived the median survival for chemotherapy or external beam radiation alone.
The potential complications of IRE are mainly attributed to electrode placement and therefore similar to that of image guided liver biopsies and current percutaneous thermal ablative procedures. Absolute contraindications to IRE include patients with metallic Wallstent in the common bile duct or other metallic objects within the electroporation zone [8]. However, there is recent literature describing successful IRE in patients with indwelling metallic Wallstent [8].
Conclusion
IRE which remains a novel ablative method allowed for a successful ablative option in our patient with an unresectable hilar cholangiocarcinoma with promising results as far as 13 months post procedure. Continued research and clinical trials with higher power or combinational therapy with chemotherapy and/or external beam radiation could carry forth promising results not only for IRE applications and patients, but continue to open more doors for the future of interventional radiology.
References
- Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, et al. (2002) Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol 37: 806-813.
- Scheffer HJ, Nielsen K, de Jong MC, van Tilborg AA, Vieveen JM, et al. (2014) Irreversible electroporation for nonthermal tumor ablation in the clinical setting: a systematic review of safety and efficacy. J Vasc Inter Rad 25: 997-1011.
- Lee EW, Thai S, Kee ST (2010) Irreversible electroporation: a novel image-guided cancer therapy. Gut and Liver 4: 99-104.
- Nakeeb A, Pitt H (2005) Radiation therapy, chemotherapy and chemoradiation in hilar cholangiocarcinoma. HPB 7: 278-282.
- Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, et al. (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Eng J Med 362: 1273-1281.
- Zeng ZC, Tang ZY, Fan J, Zhou J, Qin LX, et al. (2006) Consideration of the role of radiotherapy for unresectable intrahepatic cholangiocarcinoma: a retrospective analysis of 75 patients. Cancer J 12: 113-122.
- Ramírez-Merino N, Aix SP, Cortés-Funes H (2013) Chemotherapy for cholangiocarcinoma: An update. World J Gastrointest Oncol 5: 171-176.
- Melenhorst MC, Scheffer HJ, Vroomen LG, Kazemier G, van den Tol MP, et al. (2016) Percutaneous irreversible electroporation of unresectable hilar cholangiocarcinoma (klatskin tumor): a case report. Cardiovasc Inter Rad 39: 1 17-121.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 5380
- [From(publication date):
April-2017 - Aug 18, 2025] - Breakdown by view type
- HTML page views : 4405
- PDF downloads : 975