Review Article Open Access
Palliative – Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiotherapy (SBRT): Innovative and Effective Tool in the Management of Advanced Cancer Using Modern Radiotherapy Instrumentation
Beatriz E. Amendola*, Marco Amendola, Naipy Perez, Jesus M. Blanco and Xiaodong WuInnovative Cancer Institute 6141, Sunset Drive Suite 102 South Miami, FL 33143, USA
- *Corresponding Author:
- Beatriz E. Amendola
Innovative Cancer Institute 6141
Sunset Drive Suite 102
South Miami, FL 33143, USA
Tel: 1305-669-6833
E-mail: dramendola@innovativecancer.com
Received date: February 06, 2015; Accepted date: March 16, 2015; Published date: March 27, 2015
Citation: Amendola BE, Amendola M, Perez N, Blanco JM, Wu X (2015) Palliative – Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiotherapy (SBRT): Innovative and Effective Tool in the Management of Advanced Cancer Using Modern Radiotherapy Instrumentation. J Palliat Care Med 5:216. doi: 10.4172/2165-7386.1000216
Copyright: © 2015 Amendola BE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Radiation therapy remains an indispensable tool in palliative care. However, in the past, in order to achieve the results needed, palliative radiation therapy took weeks, a span of time which was often too long for terminal patients to bear. Advances in medical imaging and radiation therapy hardware and software have made possible to deliver high doses of focal radiation using shortened fractionation schemes. These may range from 1 to 5 fractions, targeting only the tumor area with optimized protection of normal tissue, which results in minimal toxicity, less physical demands to the patient and most importantly, more prompt palliative response. A novel radiation therapy technique, called “Stereotactic Radiosurgery” (SRS) or “Stereotactic Body Radiotherapy” (SBRT), originally developed and used as primary modality of treatment for many cancers with curative intent, is becoming an invaluable tool in the palliative care of patients with terminal cancer. In this article, we describe a typical case where SRS/SBRT demonstrates its value and efficacy and discuss present and future applications of this innovative technique in the palliative care of patients with terminal cancers.
Keywords
Metastases; Cancer; Radiation Therapy; Stereotactic radiosurgery; SRS; Stereotactic body radiotherapy; SBRT; Palliation; Brain; Extracranial
Introduction
The goal of palliative radiation therapy is to achieve meaningful relief of symptoms and promote quality of life in patients with advanced cancer instead of trying to achieve cure [1]. Due to the generally poor physical conditions of patients with terminal cancers, and the need to achieve a relatively fast relief response, the ideal would be to use a radiation modality that is delivered in a short time with minimal acute toxicity achieving durable palliation. This is virtually the definition of “Hypofractionation” a radiation therapy technique which prescribes fewer, larger-dose-per fraction treatments delivered over a shorter time period than the usually protracted conventional radiation scheme which uses daily fraction sizes of 1.8 to 2.0 Gy for several weeks [2]. This is actually nothing new as hypofractionation was used since the beginnings of Radiation Oncology through the early 1900’s. At that time its higher incidence of severe “late effects” caused many radiation oncologists across the world to abandon hypofractionation as a method for curative treatment. It was assumed that hypofractionation produces a higher risk of late complications due to irreversible damage in irradiated healthy tissues surrounding the target. The mainstream of radiation therapy has thus taken the path of the protracted fractionation scheme. Early application of hypofractionation was often limited to patients with advanced disease with the assumption that late effects would not be seen due to the patients’ short life expectancy. It was however often accompanied with severe acute toxicity.
Recently, hypofractionation has been making a comeback thanks to technical innovations including improvement in radiation treatment units with faster delivery of higher dose, intensity modulation, and improved radiation planning systems, use of image guided techniques and the acquisition of new radiobiological data [3]. The success of such comeback lies in the ability to deliver a large dose of radiation to the target with high precision avoiding excessive amount of radiation exposure to surrounding normal tissues. This innovative technology is usually called Stereotactic Radiosurgery or SRS when used in the brain and Stereotactic Body Radiotherapy or SBRT when used in the body. As defined by the America Society of Therapeutic Radiation Oncology (ASTRO) on June 2006 and reaffirmed in November 2009, “Stereotactic Radiosurgery (SRS) is a distinct discipline that utilizes externally generated ionizing radiation in certain cases to inactivate or eradicate (a) defined target(s) in the head and spine without the need to make an incision. The target is defined by high-resolution stereotactic imaging. To assure quality of patient care the procedure involves a multidisciplinary team consisting of a neurosurgeon, radiation oncologist, and medical physicist” [4].
Contrary to the popular perception of being a modern development, radiosurgery has a long history as impressive as conventional radiation therapy. It started with the creation of the first Gamma Knife by Dr. Lars Leksell in 1951 and it was perfected in the late 1960s in Sweden’s Karolinska Institute [5]. The GammaKnife was the first machine specifically designed to deliver ablative doses to achieve complete obliteration of intracranial arteriovenous malformations (AVMs) as an alternative to microsurgery. This application swiftly expanded to treat benign and malignant brain tumors. Its successful clinical outcome established the foundation for intracranial radiosurgery [6]. Following its success, intracranial radiosurgery with radiation delivery systems other than GammaKnife, was investigated since the 80’s and has achieved equivalent clinical efficacy. These systems are mainly linear accelerator-based platforms, with progressively improved technologies, notably, on-board image guidance (real-time or near real-time) and intensity modulation. These advances enabled the extension of radiosurgery to other body sites outside of intracranial region making it practical to deliver ablative radiation dose in 1 to 5 fractions. A new terminology, “Stereotactic Body Radiotherapy” or “SBRT” was introduced and it has rapidly gained popular recognition to describe this technical innovation in general. Stereotactic body radiation therapy (SBRT) is an external beam radiation therapy method used to very precisely deliver a high dose of radiation to an extracranial target within the body, using either a single dose or a small number of fractions. Specialized treatment planning results in high target dose and steep dose gradients beyond the target. SBRT can be applied using noninvasive or minimally invasive stereotactic localization and radiation delivery techniques. It requires significantly improved delivery precision over that required for conventional radiotherapy. Maneuvers to either limit or compensate for target movement during treatment planning and delivery are often useful and may be required as defined in the ASTRO guidelines for the performance of SBRT [7].
Although it has been generally acknowledged that radiosurgery (SRS) should refer to the delivery of a single-fraction ablative radiation dose to the treatment target volume, and SBRT should refer to 1 to 5 fractions of high dose (higher than 5 Gy) to the treatment target volume, there is no sharp differentiation between the two and they are often used interchangeably.
The goal of SRS or SBRT is to administer an ablative dose to treatment targets without damaging the surrounding normal tissue. Their unique physical characteristics are: high precision (sub-millimeter), high dose gradient outside of target volume (about 10% dose fall-off per mm outside of treatment margin), and high dose.
Much of early and present mainstream clinical applications of SRS/SBRT are with curative intent or with justification of favorable prognosis. We wish to draw attention to the possibility of advancing SRS/SBRT beyond its current scope applications, to the care of patients with terminal cancer. The justification is simple and sound: the higher fractional dose warrants a faster relief of symptoms, and the high dose gradient minimizes radiation toxicity of normal tissues and thus improves patients’ quality of life.
State of the Art
SRS/SBRT is an ideal technique for palliation in patients who develop symptoms such as pain, bleeding, and for example obstruction of the upper airway or urinary or gastrointestinal tracts making it possible to obtain excellent prompt results in a short treatment course. The management of patients with late-stage lung cancer, bone metastases and multiple brain metastases is briefly described below. As an institutional experience, we present a case in which SBRT was used for the care of a late-stage cancer patient.
Management of late-stage lung cancer patients
A clear advantage of a very short hypofractionated regimen is to palliate patients for example with advanced Non-Small Cell Lung Cancer (NSCLC) with a short expected survival time allowing them to spend more of their remaining time at home rather that in a hospital [8]. Respiratory symptoms are common in patients with locally advanced lung cancer and are effectively palliated with conventional single doses of 10 Gy to the thoracic inlet and mediastinum. A practical approach would be to use SBRT in these patients to ameliorate chest pain and hemoptysis, cough and dyspnea obtaining faster responses with longer local control [9-11].
Management of bone metastases and bone pain
Osseous involvement is a common cause of cancer pain. It is estimated that over 100,000 people in the United States develop bone metastases each year and 350,000 die annually with it [1]. These patients may benefit greatly from radiation therapy [12,13]. Takahashi, et al recently described in their mini-review published in 2014 the value and benefits of radiation therapy for the management of bone metastases and metastatic spine cord compression [14]. Although the appropriate fractionation regimen is still in debate, several meta-analyses and randomized studies have shown that single fraction (total dose 5 to 15 Gy) is as effective in pain relief as multifraction (total dose 15 to 30 Gy in three to 10 fractions) radiotherapy for painful bone metastases [11-13]. The brief course of treatment naturally shortens the time from treatment to pain relief. For localized bone pain, SBRT is clearly more advantageous in providing prompt pain relief without causing significant acute or long-term toxicity. Radiosurgery is an excellent technique for the management of spine metastases commonly using either 18 Gy in a single session or 3 sessions of 7 Gy depending on the volume to treat [15]. This usually achieves quick pain relief with a short treatment course without compromising concomitant chemotherapy [16]. This has also been shown to be a useful approach in patients with spinal cord compression where emergency radiotherapy is needed. This condition must be diagnosed and treated early to prevent irreversible neurologic injury. Back pain usually precedes neurologic deficit, which can evolve to paraplegia within hours or days.
Management of multiple brain mets
Owing to recent advances in systemic cancer treatment, an appropriately selected group of patients with brain metastases can now achieve longer survival with good quality of life if brain metastases are well controlled. This can be achieved using radiosurgery, which compared to the standard Whole-Brain Radiation Therapy (WBRT) has several advantages: 1) can be done in one day; 2) more than 80% of patients will have their tumor control by this treatment leading to early and lasting symptom palliation; 3) patients have lower incidence and severity of deterioration of neurocognitive function [17]. Single fraction is an effective scheme of radiation treatment that produces long-term survivals in many types of cancer without the toxicity of whole brain radiation with the classic protracted regimen. For several years there has been mounting evidence that patients with up to 10 metastases might be potential candidates for SRS alone [18]. A recent study suggests that SRS without WBRT in patients with 5 to 10 brain metastases is non-inferior to that in patients with 2 to 4 brain metastases [19].
Case Report
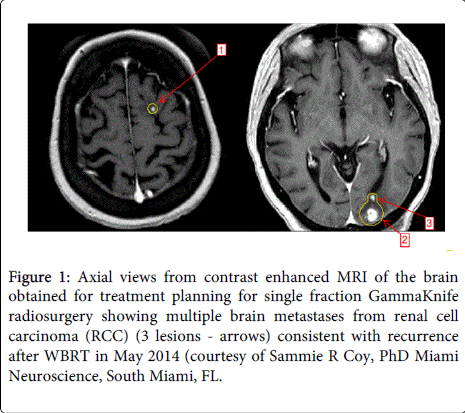
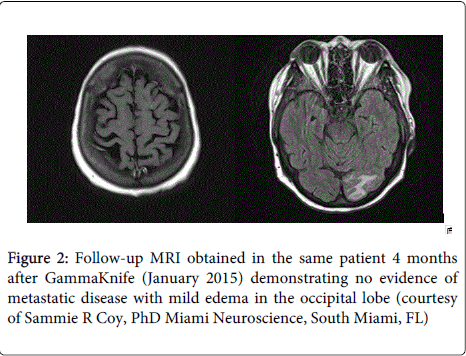
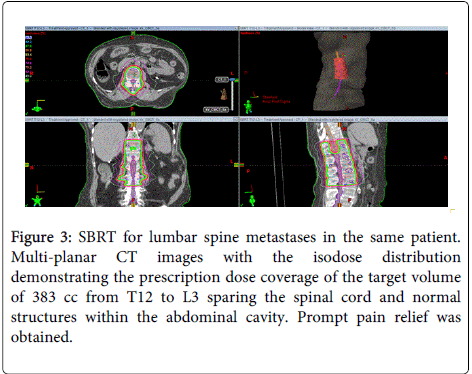
A 67 year old wheelchair-bound female with history of renal cell carcinoma (RCC) treated with a right radical nephrectomy in 2004 and left nephrectomy for recurrent tumor in 2008, who was undergoing regular dialysis at the time of consultation, presented in May 2014 with 6 small brain metastasis. She received 30 Gy in 3 Gy daily fractions over two weeks of whole brain radiation at another institution. She subsequently developed recurrent brain metastasis in early September of the same year, and was treated with single fraction of 11 Gy using Gamma Knife radiosurgery to three metastatic lesions (Figures 1 and 2). In October 2014, she presented with severe back pain, later proven to be due to metastatic disease to the lower thoracic and upper lumbar spine secondary to metastatic RCC. In November 2014 she received palliative SBRT, in 5 fractions of 5 Gy each to the T12 to L3 spine with a volume of 383 cc (Figure 3), using a Linear Accelerator (LINAC). The patient was pain-free immediately after the spinal SBRT and had a complete negative follow up brain MRI in January 2015 and continues to do well as of March 2015. This case demonstrates the feasibility and efficacy of using SRS for brain metastasis after WBRT, as well as the value of SBRT for large volume spinal metastasis for palliation of severe bone pain. The precise delivery of spinal SBRT avoided large dose of radiation to the adjacent spinal cord and bowels significantly minimizing toxicity.
Figure 1: Axial views from contrast enhanced MRI of the brain obtained for treatment planning for single fraction GammaKnife radiosurgery showing multiple brain metastases from renal cell carcinoma (RCC) (3 lesions - arrows) consistent with recurrence after WBRT in May 2014 (courtesy of Sammie R Coy, PhD Miami Neuroscience, South Miami, FL.
Figure 3: SBRT for lumbar spine metastases in the same patient. Multi-planar CT images with the isodose distribution demonstrating the prescription dose coverage of the target volume of 383 cc from T12 to L3 sparing the spinal cord and normal structures within the abdominal cavity. Prompt pain relief was obtained.
This case study demonstrates the value of the hypofractionation with SRS/SBRT in the management of an advanced cancer patient with bone and brain metastasis with improved quality of life.
Discussion
Radiation therapy is still not a widely used tool for palliation in advanced cancer patients even though is one of the best options available. It fulfills all palliative requirements including short treatment duration. As modern radiation therapy instrumentation advances, SRS/SBRT has become easily accessible, and with its minimal normal tissue toxicity, many patients could benefit from it instead of being treated with expensive systemic therapies with significant associated toxicity.
A recent study from Bernard et al. demonstrates that cancer patients have a greater financial burden than patients with other chronic illnesses: 13% of the cancer patients spend at least a 20% of their income on healthcare costs and insurance [20]. The newer equipment and resources costs associated with cutting-edge radiation oncology technologies can be partly mitigated by shorter treatment courses. Better tumor control and less toxicity, together with fewer treatment courses decrease the indirect costs of cancer care, including lost time and economic productivity secondary to treatment-related and cancer-related illness and death [21].
In general, we tend to use newer technologies only with curative intent and in early cancer where we expect long term results. However recent emerging clinical data including our own early institutional experience supports the use of newer localized radiation delivery in selected patients in need of rapid and effective palliation.
Conclusion
SRS/SBRT can achieve rapid and effective palliation with minimal toxicity and should be seriously considered as a modality for cancer palliation. This technique is convenient for the patient as well as for the family caring for the terminal patient. Furthermore, when applied adequately it can be more cost effective compared to systemic therapy.
References
- Brashears JH (2013) Palliation of Bone Metastases in: Brady LW, Yagger TE (eds) Encyclopedia of Radiation Oncology, Springer-Verlag, Heidelberg, Berlin.
- Alongi F, Scorsetti M (2012) Hypofractionation in current clinical practice: a flash forward to the near future of radiation oncology?Tumori 98: 395-397.
- Timmerman RD (2008) An overview of hypofractionation and introduction to this issue of seminars in radiation oncology.SeminRadiatOncol 18: 215-222.
- ACR Practice Guidelines: ACR/ASTRO Practice Parameter for the Performance of Stereotactic Radiosurgery March 2015
- Leksell L (1951) The stereotaxic method and radiosurgery of the brain.ActaChirScand 102: 316-319.
- Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, et al.(2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomized trial. 63: 1665-1672.
- Potters L, Kavanagh B, Galvin JM, Hevezi JM, Janjan NA, et al. (2010) American Society for Therapeutic Radiology and Oncology (ASTRO) and American College of Radiology (ACR) Practice Guideline for the Performance of Stereotactic Body Radiation Therapy. Int J Radiation Oncology BiolPhys 76: 326-332.
- Beli I, Koukourakis G, Platoni K, Tolia M, Kelekis N, et al. (2010) Hypofractionated radiotherapy in non small cell lung cancer: a review of the current literature.Rev Recent Clin Trials 5: 103-111.
- Aneja S, Yu JB (2014) Comparative effectiveness research in radiation oncology: stereotactic radiosurgery, hypofractionation, and brachytherapy.SeminRadiatOncol 24: 35-42.
- Ramella S, D’Angelillo RM (2013) Radiotherapy in palliative treatment of metastatic NSCLC: not all one and the same. Ann Palliat Med 2: 92-94.
- Chen AB, Cronin A, Weeks JC, Chrischilles EA, Malin J, et al.(2013) Palliative Radiation Therapy Practice in Patients with Metastatic Non-Small-Cell Lung Cancer: A Cancer Care Outcomes Research and Surveillance Consortium (CanCORS) Study. J ClinOncol 32: 558-564
- Zhu Y (2012) Palliative radiotherapy for painful bone metastases: Short-course or long course?Ann PalliatMed 1:78-80.
- Chow E, Harris K, Fan G, Tsao M, Sze WM (2007) Palliative radiotherapy trials for bone metastases: a systematic review.J ClinOncol 25: 1423-1436.
- Takahashi T, Nashimaru K, Yamano T, Gika M (2014) Role of Palliative Radiatiotherapy for Bone Metastasis. J Palliat Care Med 4:1
- Gerszten PC, Burton SA, Ozhasoglu C, Welch WC (2007) Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution.Spine (Phila Pa 1976) 32: 193-199.
- Folkert MR, Bilsky MH, Tom AK, Oh JH, Alektiar K, et al. (2014) Outcomes and toxicity for hypofractionated and single-fraction image-guided stereotactic radiosurgery for sarcomas metastasizing to the spine.Int J RadiatOncolBiolPhys 88: 1085-1091.
- Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, et al.(2012) Radiotherapeutic and surgical management for newly diagnosed brain metastasis (es): An American Society for Radiation Oncology evidence-based guideline. Practical Radiation Oncology 2: 210-225.
- Amendola BE, Wolf A, Coy S, Amendola MA (2002) Radiosurgery as palliation for brain metastases: a retrospective review of 72 patients harboring multiple lesions at presentation.J Neurosurg 97: 511-514.
- Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, et al. (2014) Stereotatic Radiosurgery for Patients with Multiple Brain Metastases (5LGK0901): A Multi Institutional Prospective Observational Study Lancet Oncol15:387-395.
- Bernard DS, Farr SL, Fang Z (2011) National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008.J ClinOncol 29: 2821-2826.
- Amendola BE (2013) Cost effectiveness in new technologies. Reports of Practical Oncology and Radiotherapy 18: S9-S11.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15361
- [From(publication date):
March-2015 - Aug 25, 2025] - Breakdown by view type
- HTML page views : 10733
- PDF downloads : 4628