Perceptions of Infertility as a Barrier to Cervical Cancer Screening in Rural Botswana: A Qualitative Study
Received: 14-Nov-2018 / Accepted Date: 26-Nov-2018 / Published Date: 28-Nov-2018 DOI: 10.4172/2161-0711.1000634
Abstract
Background: Cervical cancer screening in Botswana and in particular the use of visual screening in rural areas has been on the rise in the past several years. Despite increased awareness and the introduction of less invasive methods of screening, qualitative data indicate that socio-cultural factors such as infertility related stigma, and beliefs about impaired fecundity affect overall efficacy of screening campaigns.
Objective: This study sought to explore barriers to the utilization of cervical cancer screening in rural communities in northern Botswana.
Methods: In-depth interviews were conducted in this qualitative research study. All interviews were transcribed and coded both manually as well as with the use of MAXQDA software to elicit themes.
Results: The respondents all had high awareness of the current visual screening with acetic acid (VIA) and the Pap smear tests but reported non-utilization of these tests when available due to concerns over potential fertility impairment. While awareness of cervical cancer was high, a relatively high lack of understanding and education about cervical cancer and its relation (or not) to fertility outcomes was reported. The major factors identified by women in this qualitative study included lack of desire to screen prior to childbearing, beliefs and fears about inevitability of cervical cancer and lack of treatment options, financial burdens, lack of familial support, geographic burdens and stigma/emotional barriers to results of screening.
Conclusion: This study provides new data on the myriad reasons for women’s lack of participation in cervical cancer screening programs. These data suggest potential cultural barriers and fears of fertility related stigma that may impact the efficacy of ongoing cancer prevention strategies. Interventions that take social and gendered beliefs about fertility into account are needed to better implement future strategies for success.
Keywords: Cervical cancer screening; Qualitative research; Cultural barriers; Infertility
Introduction
Globally, cervical cancer is one of the leading causes of death and the second most common cancer in women. Studies suggest too that those infected with HIV are at an even greater risk for contracting the disease and in a more aggressive rate [1,2]. Access to screening and use of culturally competent educational tools can be essential in lowering rates of cervical cancer and increasing prevention in rural and low to middle income contexts.
In Southern Africa, the regional prevalence of cervical cancer is 15.5% and in Botswana in particular, cervical cancer is the leading cause of cancer-related deaths [3]. In a country of just over 2 million people, over the last decade and a half, cervical cancer accounted for almost 14% of all cancers [4]. That rate has steadily risen, particularly given high incidence and prevalence of HIV and AIDS (approximately 27.5%) and the correlation of HIV and AIDS with cervical cancer [4-6]. Botswana is a stable, economically strong and democratic country and former British protectorate and has had concerted, ubiquitous and well-funded HIV and AIDS prevention programmes in place over the last several decades. Despite these programmes and attention to the AIDS epidemic, the number of women at-risk of cervical cancer will likely continue to increase until effective primary prevention efforts are established and funded in similar ways.
In 2015, the Ministry of Health in Botswana was engaged in strategies to engage rural and urban populations in cervical cancer screening through local clinics and hospitals with particular emphasis in and around the capital city of Gaborone and areas with oncology resources. In addition, in that same year, HPV vaccination programmes for youth (girls) was ramping up and implementation in schools throughout the country was planned [7,8]. While efforts to increase cervical cancer screening and preventative measures have been rolled out, it is clear that challenges to effective cervical cancer screening in Botswana remain. Lack of awareness, limited educational campaigns, lack of trained personnel (particularly in more northern, rural areas of the country) and delays in treatment and follow-up care have all hindered optimal cervical cancer prevention strategies in the nation.
Given that cervical cancer is preventable, screening techniques should be widely available and cost-effective [9-12]. Evidence shows that Pap smear screening is both efficacious and highly recommended and in contexts where Pap screening is challenged as a result of lack of resources, infrastructure or access, the use of visual inspection using acetic acid (VIA) can be both effective and more culturally acceptable [13].
Similar to anthropological studies of the acceptability of HIV and AIDS prevention and education campaigns in Botswana, current cervical cancer awareness efforts must take into consideration the cultural significance of fertility in Tswana life [14,15]. Reproductive health and decision-making remain heavily influenced by cultural imperatives for childbearing. This is particularly true in the more northern and rural areas of the country that have fewer reproductive health care resources, and cervical cancer screening and care facilities and who may rely on social networks and local/traditional healers for information.
Previous studies on obstacles to uptake of cervical cancer screening indicate that knowledge about the types of screening, education levels of women, family history of disease and availability of long-term treatment have been significant barriers in Botswana and other environments [4,5,16-22]. Little is known however about the more socio-cultural factors that may hinder women from seeking screening in this particular context. Fears about infertility, and the stigma associated with sterility or impaired reproductive health can be significant impediments to acceptance and adherence to cervical cancer screening measures. Understanding the reasons for underutilization of Pap and VIA in Botswana is key to the design of more far-reaching and efficacious cancer reduction programmes. This study seeks a more comprehensive cultural analysis of the perception and barriers that prevent women in northern rural villages in Ngamiland, Botswana from getting cervical cancer screening.
Methodology
This study was conducted in northern Botswana, in the rural villages of Maun and Shorobe as part of a longitudinal study on infertility and women’s health in the Ngamiland region of the country. Data for this particular study were gathered in June-July 2015. A qualitative study was utilized to explore perceptions of and barriers to efficacious implementation of both Pap and VIA cervical cancer screening methods through the use of in-depth interviews.
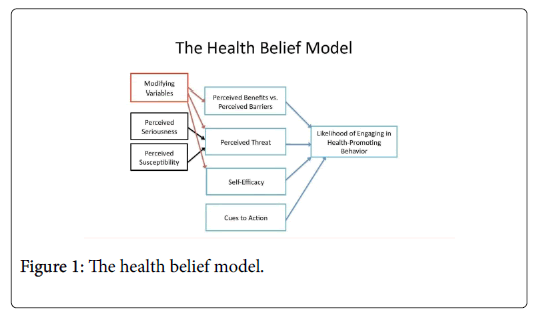
The framework used to interpret the data in this study is the Health Belief Model (HBM). The model is useful in thinking about perceptions of and barriers to screening for cervical cancer in this research. Specifically, the model can help predict behavior and potential uptake of health care, services and practices and the role that knowledge and perceptions play in personal responsibility. While the model was designed to predict behavioral response to the treatment received by chronically ill patients, and was then adapted further and used to predict more general health beliefs and practices. In this research, it was used to assess the knowledge and attitudes that rural Tswana women had about cervical cancer screening and the potential barriers associated with infertility.
In-depth interviews were conducted with 23 women. These interviews were conducted in English and SeTswana utilizing a semistructured interview guide that was developed by the author. The interview guide included background demographic information as well as specific questions about perceptions of infertility, gender and cancer screening. Snowball sampling was utilized to identify participants from the Maun and Shorobe villages in the Ngamiland region of northern Botswana.
Each interview was conducted by a trained qualitative researcher and interview facilitator. Each interview lasted between 45-90 mins in length. Detailed notes were kept during the interviews and compared with the transcribed, recorded transcripts. The notes and transcriptions formed the basis for the data that were then coded first by hand and then through the use of MAXQDA software for significant themes. Saturation was achieved, though a relatively small study and themes clearly emerged through the coding process and were reiterated consistently throughout the data. Per Patton, saturation can be achieved through the use of careful ethnographic techniques and can rely upon smaller sample sizes as long as thorough attention to question design is present and researcher experience is essential [23]. This study is part of a larger, ongoing ethnographic study on the intersections between perceptions of infertility and reproductive health outcomes. Participant observation over the past decade, demographic data as well as newly emergent data from more quantitative studies on cervical cancer in Botswana have been relied upon to help frame and support the claims made from these qualitative data. In qualitative research, “the validity of the findings is related to the careful recording and continual verification of the data that the researcher undertakes during the investigative practice” [24]. All participants were provided informed consent per IRB best practices.
By placing cervical cancer screening in larger cultural discourse about fertility and public health, the stigma and social suffering of many could be ameliorated [25]. While studying beliefs about screening and fertility in general may not directly change behaviors of patients and/or providers directly, using the Health Belief Model can capture the implications of this work [25-27]. For example, beliefs about the social significance of fertility outweighed or were considered in relation to perceptions of cancer screenings as well as women’s feelings of empowerment to seek cervical cancer education and testing.
The model illustrates how perceptions as to the seriousness and susceptibility of disease [27-33] and modifying variables such as fertility imperatives (the desire for childbearing in rural Botswana remains high for example) as well as understandings of outcomes and empowerment can determine health behaviours in general. In this study, it was clear that the HBM is a useful framework for understanding participant decision making. Use of the HBM takes qualitative, narrative beliefs and statements by participants as significant data and as important variables when considering the most efficacious interventions.
Rigor, validity and reliability are often imagined as difficult to capture in qualitative research. As others suggest, “whereas reliability in quantitative research depends on instrument construction, in qualitative research, the researcher is the instrument of the study” [24], and researcher bias should be recognized and controlled for using best practices such as multiple coders and analyses. Also, as many studies note [29-31] and as this research demonstrates, the use of multiple sources of data, particularly the long-term ethnographic commitment on the part of the researchers, to the larger research project from which this study has sprung, help to ensure rich, holistic and reliable data. As Cypress (2017) reiterates, “the strategies for ensuring validity in a qualitative study are prolonged engagement, persistent observation, thick and rich description, negative case analysis, peer review or debriefing, clarifying researcher's bias, member checking, external audits, and triangulation” [24]. All of which were present as part of the research design for this qualitative study of perceptions of infertility and utilization of cervical cancer screening in Botswana.
Results
Characteristics of women participants
A total of 23 research participants were included in this study. All were women between the ages of 25-53 years of age. Just over half, or 12 of the 23, (52%) were married at the time of the in-depth interview and 18 of the 23 (78%) had at least one child. Seven of the women (30%) had a secondary or higher education and more than half (56%) stated that they were the primary earners in their households. Three of the participants had had a Pap test in her lifetime six others stated that they had been offered or participated in a VIA screening at the clinic. The remaining participants had never had any type of cervical cancer screening.
Awareness of cervical cancer and causality
Women reported that they were increasingly aware of cervical cancer and cancers more generally but there was lack of knowledge about what caused cervical cancer in particular. Several mentioned that health care professionals were talking about cervical cancer to them more regularly and that messages to increase knowledge were being placed on billboards and on the radio. Emphases on younger populations and increasing their knowledge was something that many respondents described,
“It reminds me of when HIV and AIDS were what they were trying to educate us about, there are messages about cancer and women all the time on the radio nowadays and you are asked about what you know every time you go to a doctor.”
“I think that there is more knowledge of cancers for women, mostly like in the US it has been about breast cancer but now in this country we are focused on making sure people are tested for cervical cancer. I don’t think that most people in the more rural areas, the home 6 villages and the older people, will know about it, but they are trying to teach this and get the message out there to the younger ones.”
“I think the problem is that nobody knows where it [cervical cancer] comes from so we are aware of the testing but it is hard to know if you are someone who should get tested now or if it is something that can be just treated later.”
“The Pap test or visually looking for cancer…that is something to do once you have your child, or once you are married…I don’t think that is something that we (younger women) have to worry about.”
Clearly while awareness of cervical cancer was present and knowledge that there were tests to screen for it, levels of knowledge about how the tests were conducted and actual causes of cervical cancer were low. Many respondents believed that those who already had children were the ones who should seek screening.
Infertility and cervical cancer screening
A key factor in a majority of the responses from women in this study was the role of fertility and childbearing in relation to preventative screening. Most stated that it was important to have children prior to any testing for cervical cancer, a refrain not unlike some earlier beliefs about HIV and AIDS and other STDs.
“Having children is good for the body…for women and men but mostly women. There is a belief that if you do not have a child your blood and body become weak. There are women I know here (in this village) who say that if you go for screening it will block your blood, that when they look at you with the (VIA) or use the tool (Pap) that it will hurt the womb, that it will make it so the child, the baby, will not want to latch on and stay in the womb. So that is the reason that many women are telling younger ones not to get tested for this right away.”
For many respondents, infertility emerged as a key theme and reason for lack of testing and of participation in prevention programs. Certain socio-cultural beliefs about menstrual and blood associated with childbirth were often cited as reasons for these decisions. In particular women talked about the SeTswana verb, “go thaya ”, which means “to strengthen” or ‘cleanse’ as essential to women’s reproductive health. Specifically,
“Women’s blood is strengthened when we have children, you don’t want to have ‘weak’ blood, that is when you worry. You worry if you cannot fall pregnant and you worry if a man says he feels that you have weak blood, or that your blood does not agree with his…then you will not be able to have children…many women are thinking that having the screens [Pap/VIA] will make their blood weak, make it so they cannot have children after the test.”
“I’m worried that if I go for screening that it will make it harder for me to fall pregnant again. I have one daughter and it took many years for her and I’m afraid that if I go for the screen that I will not be able to have another child. I will wait until I have more and then go because I do know that our doctors and the clinics are telling women to get tested.”
Positive and negative perceptions of cervical cancer screening
Women in this study expressed both positive and negative reactions to cervical cancer screening although were largely wary of being tested prior to childbearing. Both Pap and VIA were considered invasive and something to be done in a clinic or hospital setting but several women in these rural areas noted that once someone had cervical cancer it was a disease more treatable by traditional healers or midwives.
“There is a problem in telling women to get tested for this…mostly women will be older when they get tested, they have their children but when they get this disease they will not have very long to live…I don’t think that women will go to get tested because there isn’t anything to do.”
“The screenings are fine but there is no cure I don’t think. Most people will go to see a local (traditional) healer if there is anything wrong…since we are in a rural area that is also the best option we have.”
Several women spoke about the stigma associated with testing and positive results, noting the potential shame of both having the test (perceived of as invasive whether it was a Pap or VIA) as well as having to undergo treatment if the tests were positive.
“My sister went for screening, she lives down south [in a more urban area] and more people go for tests there. Here they are telling us that the VIA is the better test, the other has a metal instrument and that will be uncomfortable. Either test though means that women have to be examined up close and by a doctor and for many women here I don’t think that will happen.
Nobody will want to have that done. Giving birth, bleeding, those are more private matters for a lot of women here. If you have cancer too, well, even though there are billboards about this it isn’t something talked about.”
“It is odd, here in Botswana we have talked about HIV and AIDS for so many years, there is little stigma around that, around testing for that. But cancer? And cancers that women have, that is something that many people still do not want to discuss…it won’t matter what kind of test you give them, they aren’t going to come because they don’t want to have it and they think few people do.”
Infertility and cervical cancer as public health concerns
Many women, even in these remote regions of the country, expressed awareness of cancer and reproductive health related diseases as significant public health concerns. While rates of cervical cancer have declined in more high income and urban areas worldwide, it is clear that all women can benefit from early detection and prevention strategies. Women in this study reiterated however just how important and socially significant fertility can be as a public health problem as well.
“Few people will tell you that not having children is a problem… health officials, at the clinics, those people will not tell you that there is a problem if you aren’t having children. But in our villages, in the community, it is a big problem. It is like having a disease if you don’t have children, but it is not one that anyone will put on a billboard.”
“I know many people who say that they know about cancer and that it is a problem and something they can prepare for and prevent. But I know more people, mostly women, who say that they will get checked out once they have their kids because there is a fear that doctors will only treat the cancer…they won’t treat infertility.”
“Both (infertility and cervical cancer) are problems. We know about them. But only cancer is what doctors want to see, what they want to treat. Infertility is invisible to them.”
Discussion
This study begins to explore the connections between perceptions of infertility and screening for cervical cancer in northern Botswana. In this research, most women participants were unfamiliar with symptoms of cervical cancer and believed that screening could help prevent fatalities however most reiterated their belief in a supposed connection between fertility risks and cervical cancer screening.
Women reported receiving information about cervical cancer and screening options through their social networks (conversations with other women) as well as via media advertising that is typical of Ministry of Health messaging campaigns in Botswana (the use of billboards, and radio programmes for example). Many noted that similar to prior public service awareness campaigns (for HIV and AIDS) over the years, the stigma that is associated with reproductive health and diseases may lessen, but that at present, many still felt that it might be problematic and even shameful if their test showed a need for cervical cancer treatment.
Concurrent with this study, the Botswana Ministry of Health began a nationwide HPV vaccination programme for girls aged 9-13. Given that the majority of patients in Botswana who present with cervical cancer are at a more advanced stage of the disease, the potential for a national HPV vaccination plan is tremendous [34]. Care should be given however to understanding the cultural barriers and beliefs, such as infertility fears, that may impede the vaccination programme particularly in more rural communities that have not been the target of trials.
The cultural fears of infertility as well as lack of knowledge in more rural parts of the country mean that perceptions of susceptibility to cervical cancer greatly affect screening in this region. Many women noted that they did not feel personally at risk for cervical cancer given their fertility status having already had children. Nor did they feel at risk due to misperceptions about the links between cervical cancer, HPV, other STDs and overall awareness of the screening procedures themselves.
The perceived benefits of the VIA and Pap screening methods were minimal in these rural areas. Women acknowledged that screening for cervical cancer was becoming more common and is something that health officials as well as some local and traditional healers were discussing more often, however cultural beliefs about the possible negative effects of screening on fertility hampered the benefits. Thus, perceptions of individual susceptibility as well as broader sociocultural beliefs about benefits of testing versus avoidance mean that many women felt that it was unnecessary to pursue VIA or Pap screening. The Health Belief Model demonstrates that analysis of these qualitative data can help better predict the likelihood of women engaging in health promotion behaviours in particular contexts.
Women in rural areas of Botswana were not using screening services for several reasons. Potential stigma, lack of susceptibility and socio-cultural beliefs about the potential for cervical cancer screening to affect fertility hinder use of those services. Most respondents also mentioned maternal age and childbearing status as reasons why women may not get screened. Many responses suggested that younger women should wait to get screened and yet most women acknowledged that the health education and awareness campaigns (such as those for HPV vaccination of girls) were targeted toward younger populations. These conflicting messages, beliefs about susceptibility and stigma associated with sterility all suggest potential barriers to the success of the VIA and Pap screening throughout the country.
Conclusion
This research has demonstrated that while awareness about cervical cancer is growing in rural Botswana, considerable barriers to screening remain. Women are aware of both the Pap smear test and VIA screening options but overwhelmingly reported that cultural factors related to fertility impairment and stigma associated with screening exist. There is clearly a need for ongoing awareness and education about cervical cancer prevention and screening options should be linked to culturally-competent and sensitive interventions and messaging in order to better empower women to utilize these options.
Acknowledgements
The author is grateful to all the participants who agreed to participate in this study. Furthermore, sincere thanks to regional health care administrators in Ngamiland and Gaborone, Botswana who helped to facilitate this research. No financial support was directly received for this study and the author declares no competing interests or conflict of interest. Special thanks to Joanne Angel and Nicky Thornley for assistance with an initial cost effectiveness analysis in preparation of this research.
References
- Brankovic I, Verdonik P, Klinge I (2013) Applying a gender lens on human papillomavirus infection: Cervical cancer screening, HPV DNA testing, and HP vaccination. Int J Equity Health 12: 14.
- Carmen D, Wallace M (2013) Effect of health care disparities on screening. Clin Obstetr Gynecol 56: 65-75.
- Grover S, Raesima M, Bvochora-Nsingo M, Chiyapo SP, Balang D, et al. (2015) Cervical cancer in Botswana: Current state and future steps for screening and treatment programs. Front Oncol 5: 239.
- Ramogola-Masire D, de Klerk R, Monare B, Ratshaa B, Friedman HM, et al. (2012) Cervical cancer prevention in HIV-infected women using the “See and Treat†approach in Botswana. J Acquir Immune Defic Syndr 59: 308-313.
- Suneja G, Ramogola-Masire D, Medhin HG, Dryden-Peterson S, Bekelman JE (2013) Cancer in Botswana: Resources and opportunities. Lancet Oncol 14: e290-291.
- Efstathiou JA, Nsingo MB, Gierga DP, Kayembe MKA, Mmalane M, et al. (2014) Addressing the growing cancer burden in the wake of the AIDS epidemic in Botswana: The BOTSOGO collaborative partnership. Int J Radiat Oncol Biol Phys 89: 468-475.
- Sankaranarayanan R, Budukh AM, Rajkumar R (2001) Effective screening programmes for cervical cancer in low and middle-income developing countries. Bull World Health Organ 79: 954-962.
- Mandelblatt JS, Lawrence WF, Gaffikin L, Limpahayom KK, Lumbiganon P, et al. (2002) Costs and benefits of different strategies to screen for cervical cancer in less-developed countries. J Natl Cancer Inst 94: 1469-1483.
- Denny L, Kuhn L, De Souza M, Pollack AE, Dupree W, et al. (2005) Screen-and-treat approaches for cervical cancer prevention in low-resource settings: A randomized controlled trial. JAMA 294: 2173-2181.
- American College of Obstetricians and Gynecologists (2014) College statement of policy: Cervical cancer prevention in low and middle-income countries. Washington, DC.
- Carr KC, Sellors JW (2004) Cervical cancer screening in low resource settings using visual inspection with acetic acid. J Midwifery Women’s Health 49: 329-337.
- Daher M (2012) Cultural beliefs and values in cancer patients. Ann Oncol 23: 66-69.
- Upton RL (2011) Sterility and stigma in an era of HIV/AIDS: Narratives of risk assessment among men and women in Botswana. Afr J Reprod Health 15: 95-102.
- Fang CY, Ma GX, Tan Y (2011) Overcoming barriers to cervical cancer screening among Asian American women. North Am J Med Sci 4: 77-83.
- Olowokure B, Caswell M, Duggal HV (2006) What women want: Convenient appointment times for cervical screening tests. Eur J Cancer Care (Engl) 15: 489-492.
- Thomas VN, Saleem T, Abraham R (2005) Barriers to effective uptake of cancer screening among Black and minority ethnic groups. Int J Palliat Nurs 11: 564-571.
- Williams M, Ku Our G, Ekuadzi E, Yeboah M, ElDuah M, et al. (2013) Assessment of psychological barriers to cervical cancer screening among women in Kumasi, Ghana using a mixed methods approach. Afr Health Sci 13: 1054-1061.
- Oscarsson MG, Wijma BE, Benzein EG (2008) ‘I do not need to...I do not want to...I do not give it priority...’-why women choose not to attend cervical cancer screening. Health Expect 11: 26-34.
- Mingo AM, Panozzo CA, DiAngi YT, Smith JS, Steenhoff AP, et al. (2012) Cervical cancer awareness and screening in Botswana. Int J Gynecol Cancer 22: 638-644.
- Francis SA, Nelson J, Liverpool J, Soogun S, Mofammere N, et al. (2010). Examining attitudes and knowledge about HPV and cervical cancer risk among female clinic attendees in Johannesburg, South Africa. Vaccine 28: 8026-8032.
- Patton MQ (2014) Qualitative research and evaluation methods: Integrating theory and practice. Thousand Oaks, CA: Sage.
- Cypress BS (2017) Rigor or reliability and validity in qualitative research: Perspectives, strategies, reconceptualization, and recommendations. Dimens Crit Care Nurs 36: 253-263.
- Denny L, Anorlu R (2012) Cervical cancer in Africa. Cancer Epidemiol Biomarkers Prev 21: 1434-1438.
- Tavafian SS (2012) Predictors of cervical cancer screening: An application of health belief model. In Topics on Cervical Cancer with an Advocacy for Prevention.
- Gillam SJ (1991) Understanding the uptake of cervical cancer screening: The contribution of the health belief model. Br J Gen Pract 41: 510-513.
- Ackerson K, Pohl J, Low LK (2008) Personal influencing factors associated with pap smear testing and cervical cancer. Policy Polit Nurs Pract 9: 50-60.
- Morse JM (2015) Critical analysis of strategies for determining rigor in qualitative inquiry. Qual Health Res 25: 1212-1222.
- Houser J (2013) Nursing research: Reading, using, and creating evidence. (2nd edn). Burlington, MA: Jones and Bartlett Learning.
- Merriam SB, Leahy B (2005) Learning transfer: A review of the research in adult education and training. PAACE J Lifelong Learn 14: 1-24.
- Rosenstock, Irwin M (1974) Historical origins of the health belief model. Health Edu Behav 2: 328-335.
- Sadeghi R, Hashemi M, Khanjani N (2018) The impact of educational intervention based on the health belief model on observing standard precautions among emergency center nurses in Sirjan, Iran. Health Educ Res 33: 327-335.
- Republic of Botswana Ministry of Health (2012) National cervical cancer prevention program.
Citation: Upton RL (2018) Perceptions of Infertility as a Barrier to Cervical Cancer Screening in Rural Botswana: A Qualitative Study. J Community Med Health Educ 8: 634. DOI: 10.4172/2161-0711.1000634
Copyright: © 2018 Upton RL. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5618
- [From(publication date): 0-2018 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 4697
- PDF downloads: 921