Professional Risk Factors for Burnout among Medical Residents
Received: 22-Feb-2018 / Accepted Date: 09-Mar-2018 / Published Date: 12-Mar-2018 DOI: 10.4172/2161-0711.1000596
Abstract
Study background: We aimed to identify professional risk factors for burnout among residents in medicine and surgery.
Materials and methods: Epidemiological, observational, and cross-sectional study among trainee physicians working in the Champagne-Ardenne region, from 31 March to 3 May 2015. Burnout was assessed using the Maslach Burnout Inventory (MBI). Variables recorded included the location of the residency, the type of unit (hospitalisation ward, emergency department, consultations), workload, and exposure to patients’ suffering. Karasek’s Job Content Questionnaire was also administered. For each component of the MBI, univariate and binary logistic regression was performed to identify risk factors.
Results: In total, 191 out of 644 eligible residents (29.7%) completed the survey. The majority were working in conditions likely to pose a risk to their health: 42.4% were exposed to job strain, and 19.9% had iso-strain. Overall, 62.8% of residents presented at least one component of burnout as assessed by the MBI. By multivariate analysis, risk factors for emotional exhaustion were high psychological demands (Odds Ratio (OR) 1.16; 95% confidence interval (95% CI) 1.05-1.29) and iso-strain (OR 3.25; 95% CI 1.29-8.22), while high psychological demands were also a risk factor for depersonalization (OR 1.14; 95% CI 1.07-1.22). Working in a hospitalisation unit (OR 3.66; 95% CI 1.30-10.3) and not meeting patients’ families (OR 11.7; 95% CI 3.08-44.4) were risk factors for a feeling of low personal accomplishment, whereas increased decision latitude had a protective effect (OR 0.95; 95% CI 0.91-0.99).
Conclusion: This study identifies occupational risk factors for burnout among residents in training, and provides a useful basis for preventive measures aimed at changing the organisational structure in the hospital setting with a view to improving mental health among trainee physicians.
Keywords: Burnout; Medical students; Risk factors; Psychosocial factors
Introduction
Many developments in the working environment have come about through modernisation (including automation and increasing use of computers), yet the number of occupational diseases, such as musculoskeletal disorders, professional burnout or even Karôshi (literally, death from overwork) has considerably increased in recent years in tertiarised countries.
Professional burnout: Background concepts
The concept of burnout was first described in 1975 by the psychiatrist and psychoanalyst Herbert J. Freudenberger, to qualify a state of failure or exhaustion among the staff of alternative self-help institutions for drug addicts Maslach et al. [1], developed an instrument to measure the extent of burnout syndrome, namely the Maslach Burnout Inventory (MBI) [2]. This is a validated, selfadministered questionnaire designed for use among the helping professions, and it explores three dimensions of burnout, namely:
• Emotional, physical and psychological exhaustion (9 items), which is a key dimension characterized by intense fatigue.
• Depersonalization (5 items), characterized by cynicism, loss of empathy, a negative and detached attitude towards work, colleagues, clients or patients.
• Personal accomplishment (8 items), exploring beliefs of competence and successful achievements in work.
Burnout in healthcare professionals
Burnout among workers within the healthcare system can affect all job types, including administrative staff, physicians, nurses, nursing assistants [3].
Two Spanish studies have reported a higher prevalence of burnout among primary care staff. In one of these studies, carried out in the Navarro region of Spain [4], the authors reported that 39.3% of subjects presented at least one of the three dimensions of burnout to a significant degree. They compared to 46.2% with at least one of the three components in the second study, carried out in the Barcelona region [5]. The professions most affected by burnout in these two studies were administrative staff (80%) and family physicians (41.3%) in the Navarro-Gonzalez’s study, and social workers (64.3%) and administrative staff (53.3%) in the Vilà Falgueras’ study. Healthcare workers in oncology are also frequently affected by burnout. In the study by Zanatta et al. [6] carried out in an onco-hematological pediatric unit, 29.8% of nurses had a high depersonalization score and 27.8% of physicians had a low score on personal accomplishment at work. Risk factors for burnout in a population of French oncohematology workers included working in emergency care, poor communication at work, and a lack of appreciation of their work [7].
Burnout among physicians represents a major public health challenge for several reasons. Firstly, it is a frequent affliction, being twice as frequent as in other professions, with a prevalence among physicians ranging from 25 to 65% [8]. Secondly, the individual consequences can be drastic, including for example losing one’s job, increased risk of cardiovascular disease, increased risk of addictive behaviours, and higher levels of depression or even suicide. Indeed, suicide is reported to be 6 times higher in physicians than among the general population [9].
Thirdly, burnout among physicians has significant deleterious repercussions on the quality of care, and is namely associated with poorer quality of care [10]. Indeed, medical residents in Holland suffering from burnout reported making more errors in action or judgement than those not suffering from burnout [11].
Burnout among residents in medicine and surgery
In France, medical residents play a major role in healthcare delivery in the hospital setting. Although still in training, they shoulder significant responsibilities, face organisational constraints imposed by the hospital setting, and have a very high volume of working hours (including night duties, and a working week of 60 hours on average (ISNIH 2012)). In addition, they are confronted with the suffering of patients and families on a daily basis.
Then, at the end of their training, they often find themselves in competition with their peers to obtain the best jobs. In France, medical residency commences in the seventh year of medical studies after a national classifying examination, where the rank obtained by the students determines their ability to select the specialty and city in which they want to carry out their 3 to 5 years of residency.
It is thought that burnout may be highly prevalent among this population. Indeed, 60.8% of residents in anesthesiology-critical care in the west of France reportedly presented at least one component of the MBI in one study [12]. A French nationwide study of burnout among residents in family medicine (future general practitioners) showed that only 41.9% of them did not have an elevated MBI score [13].
Reported risk factors for burnout in this population include working more than 48 hours per week, lack of appreciation on the part of the medical team or patients, fear of making a mistake, and working in internal medicine or the emergency department. To date, the studies that have examined the risk factors for burnout in French medical residents have generally only included students from a single specialty.
However, to improve our knowledge of the risk factors for burnout, all medical specialties warrant investigation, so that appropriate preventive measures targeting at-risk residents can be implemented. Therefore, the aim of this study was to identify the risk factors for burnout among residents in medicine and surgery in the region of Champagne-Ardenne, in France.
Materials and Methods
Study design
We performed a observational, cross-sectional, and epidemiological study in the region of Champagne-Ardenne, in France, from 31 March to 3 May 2015.
Study population and data collection
We included all residents in medical and surgical disciplines who were duly registered at the Faculty of Medicine of the University of Reims-Champagne-Ardenne for the academic year 2014-2015 and who were performing their residency in the region of Champagne- Ardenne, including all those actively working, and those on sick leave or maternity leave during the semester from 3 November 2014 to 3 May 2015. Students who were performing their residency in hospitals outside the region of Champagne-Ardenne, as well as foreign students, and those registered in a university other than the University of Reims, were excluded.
An email explaining the study objectives and containing a link to an anonymous questionnaire online was sent to a reference resident (contact person) for each of the 27 medical and surgical specialties in the last month of the semester. This referent resident then forwarded the email with the link to the questionnaire to all the other residents in their specialty.
Questionnaire
The questionnaire was designed using the open-source survey application Limesurvey® (www.limesurvey.org), and comprised 3 parts:
The first part collected socio-demographic data: sex; age; marital status; number of children; whether or not the respondent had been able to choose the specialty and city of their choice after the national classification exam; the number of semesters of residency already performed; professional situation during the semester (actively performing residency, on a year of absence to perform research, on sabbatical, on sick leave, on maternity leave); whether they were also registered for any other university qualifications in the region or elsewhere; whether they were preparing their MD thesis to qualify as a medical doctor.
The second part of the questionnaire recorded psychological and organisational constraints: location of residency (university hospital or general (non-academic) hospital); type of work performed (emergency department, hospital ward, consultations, laboratory, residency in desired specialty); workload (number of hours worked per week, number of week-ends worked per month, number of night duties or nights on-call per month, whether they were able to take their mandatory rest-day after a night duty); extent of exposure to suffering (meet families and patients every day, announce diagnosis of serious disease or death, death of several patients since start of semester). Presenteeism (i.e. when workers are physically present at work even though their state of health would justify sick leave) was self-reported, and the number of days of presenteeism was estimated by the resident. The last component of the second section was the Karasek questionnaire. Karasek’s Job Content Questionnaire assesses the psychosocial work environment with 26 items regrouped in 3 domains, with responses on a 4-point Likert scale from 1 (totally disagree) to 4 (totally agree). This instrument measures 3 scales related to the psychosocial environment in the workplace, namely:
• Psychological demands (9 items), evaluating the respondent’s impressions of the quantity, intensity and interruptions;
• Decision latitude (9 items), describing the resident’s control over the performance of their job, particularly as regards use and development of their skills, and the freedom they have to make decisions;
• Social support (8 questions), assessing the support available to the resident from coworkers and/or supervisors.
These 3 dimensions make it possible to identify situations at risk of
• Job strain (low decision latitude (<71) and high psychological demand (>20));
• Or iso-strain (job strain + low social support (<24)).
The last part of our on-line questionnaire evaluated burn-out using a self-reported global question (“Do you feel that you are in burnout?”) and using the Maslach Burnout Inventory (MBI).
Answers were on a 7-point Likert scale from 0 (never) to 6 (every day). The sum of the responses was calculated for each subscale, to define mild, moderate or severe burnout for each subscale. Each subscale was considered as an explanatory variable, and scores were considered abnormal for:
• A score >29 on the emotional exhaustion subscale.
• A score >11 on the depersonalization subscale.
• Or a score <34 on the personal accomplishment subscale.
Lastly, there was a free-text zone to allow residents to provide more details regarding their responses, or to suggest other risk factors for suffering in the workplace that they felt were not addressed in our questionnaire.
Statistical analysis
For descriptive analysis, quantitative variables are described as mean ± standard deviation. Qualitative variables are described as number (percentage).
For each subscale of the MBI, univariate analysis was performed, followed by multivariate analysis by binary logistic regression to investigate the relation with explanatory variables.
All variables with a significance level of p<0.15 by univariate analysis were included in the multivariate analysis. Results are expressed as Odds Ratio (OR) with 95% confidence interval (95% CI). A p-value<0.05 was considered statistically significant. All analysis were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Ethical considerations
The study was approved by the Dean and the Management Committee of the Faculty of Medicine of the University of Reims.
The preventive medicine department of the University Hospital of Reims, which is responsible for the follow-up of residents in medicine and surgery, was informed about the study.
The National authority for the protection of privacy and personal data waived the need for approval to store the data from this study since it was entirely anonymous.
Results
Study population
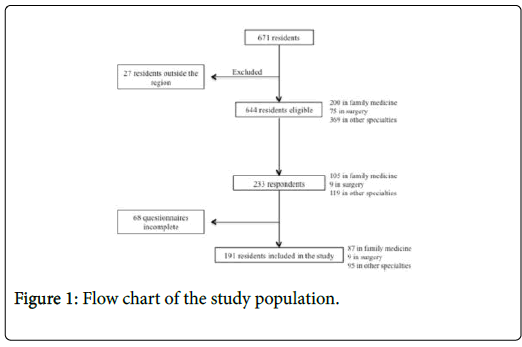
During the study period, 671 residents were registered in Champagne-Ardenne, of whom 644 were eligible for the study. Among these, 191 (29.7%) completed questionnaires were included in this analysis (87/200 (43.5%) family medicine; 9/75 (12%) surgery; 95/369 (25.7%) in other specialties (Figure 1).
The average age of the respondents was 27.4 ± 3.3 years, 65.5% were women. Most had been able to choose their desired specialty (85.9%) after the national classification examination, but almost one third did not have the choice of the city in which they were to perform their residency. The demographic and professional characteristics of the study population are shown in (Table 1).
| Variables | All (N=191) |
| Women | 125 (65.5%) |
| Married / living maritally | 141 (73.8%) |
| Were able to choose desired | |
| specialty | 164 (85.9%) |
| location of residency | 131 (68.6%) |
| Specialty | |
| Family medicine | 87 (45.6%) |
| Surgery | 9 (4.71%) |
| Other specialties | 95 (49.7%) |
| Status | |
| Actively working | 185 (96.9%) |
| On a research year | 4 (2.09%) |
| On sabbatical | 0 |
| On maternity leave | 1 (0.52%) |
| On sick leave | 1 (0.52%) |
| Registered for another university diploma | 81 (42.4%) |
| MD Thesis ongoing | 70 (36.7%) |
Table 1: Demographic and professional characteristics of the study population.
Organisational constraints
The respondents were exposed to a substantial number of psychological and organisational constraints (Table 2). Most residents were working in a hospital setting (83.3%), mostly in hospitalisation wards, and therefore had daily contact with patients and their families. Overall, the workload was high, with an average working week of 52 hours, up to a maximum of 82 hours. In total, 122 (63.9%) residents reported that they worked on Saturdays or Sundays, they worked 1.9 ± 0.74 weekends per month. Among the 136 (71.2%) residents who performed night duties, the average number of night duties per month was 3.49 ± 1.49, and 93.4% of these were able to take the mandatory rest day on the day after their night duty.
| Variables | All (N=191) |
|---|---|
| Residency being performed | |
| In the hospital setting | 159 (83.3%) |
| University hospital | 79 (49.7%) |
| Emergency department | 21 (13.2%) |
| Hospitalisation wards | 106 (66.7%) |
| Laboratory | 5 (3.14%) |
| Consultations (in-hospital or outside of hospital) | 43 (22.5%) |
| Residency corresponds to the specialty chosen | 106 (55.5%) |
| Daily contact with patients | 174 (91.1%) |
| Meets patients’ families | 166 (86.9%) |
| Has to announce serious disease / death | 132 (69.1%) |
| Reported presenteeism | 73 (38.2%) |
| Karasek’s Job Content Questionnaire | |
| Job strain | 81 (42.4%) |
| Iso-strain | 38 (19.9%) |
| Number of hours worked per week | 52.4 ±11.7 |
| Week-ends worked per month | 1.21 ±1.09 |
| Night duties / nights on call per month | 2.49 ±2.02 |
Table 2: Psychological and organisational constraints.
Over the course of the last month, 38.2% of respondents estimated that they had gone to work during the semester at times when their state of health would have justified sick leave. The average number of days of presenteeism was 6.51 ± 8.48.
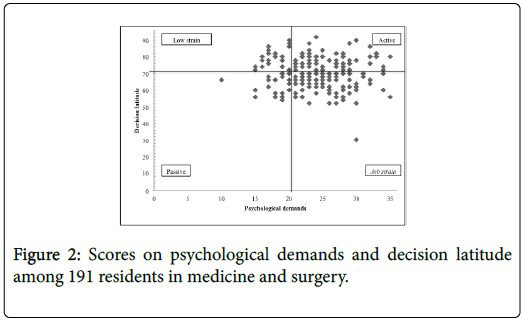
Karasek’s Job Content Questionnaire showed that the majority of residents were in a job that represented a hazard to their health, with 42.4% in a situation of job strain (i.e. situation combining high psychological demands with low decision latitude), and 19.9% in isostrain (i.e. job strain plus low social support from co-workers/supervisors) (Figure 2). Shows the distribution of scores on psychological demands and decision latitude among the respondents.
Emotional exhaustion
In total, 120 (62.8%) residents presented one or more components of burnout. Among the 15 residents who presented all three components of burnout, 6 were working in family medicine, and 9 in other specialties.
Despite the high number of respondents with at least one component of burnout as assessed by the MBI (Table 3), only 18 (9.42%) self-reported being in burnout. Among these, 4 had all 3 components of burnout, 4 were in situation of job strain and 10 in isostrain.
| Variables | All (N=191) |
|---|---|
| High emotional exhaustion | 41 (21.5%) |
| High level of depersonalization | 80 (41.9%) |
| Low level of personal accomplishment at work | 65 (34.0%) |
| Component (1) | 69 (36.1%) |
| Components (2) | 36 (18.8%) |
| High exhaustion & high depersonalization | 28 (14.7%) |
| Components (3) | 15 (7.85%) |
Table 3: Scores on Maslach Burnout Inventory among 191 residents in medicine and surgery.
Risk factors for burnout: Univariate analysis
Univariate analysis identified explanatory variables associated with burnout in medical residents (Table 4). Risk factors for high emotional exhaustion mainly concerned the work in a hospitalisation ward: high workload, high psychological demand, lack of latitude to make decisions and exercise skills. Certain risk factors were more focused on the individual’s behaviour, with presenteeism and self-reported burnout both associated with a higher risk of emotional exhaustion.
| Variables | High emotional exhaustion | ||
|---|---|---|---|
| OR | 95% CI | p | |
| Working in a hospitalisation ward | 3.05 | 1.25-7.44 | 0.01 |
| 1 additional hour of work per week | 1.06 | 1.02-1.09 | 0.0006 |
| 1 additional weekend worked per month | 1.48 | 1.08-2.04 | 0.02 |
| 1 additional night duty per month | 1.19 | 1.00-1.42 | 0.05 |
| Presenteeism | 2.25 | 1.12-4.53 | 0.02 |
| 1 additional day of presenteeism per semester | 1.12 | 1.04-1.21 | 0.003 |
| Psychological demand (per + 1 point) | 1.26 | 1.15-1.38 | < 0.0001 |
| Decision latitude (per + 1 point) | 0.95 | 0.92-0.99 | 0.01 |
| Exercise skills (per + 1 point) | 0.92 | 0.86-1.00 | 0.04 |
| Freedom to make decisions (per + 1 point) | 0.93 | 0.88-0.99 | 0.02 |
| Social support (per + 1 point) | 0.87 | 0.79-0.96 | 0.005 |
| Support from supervisors (per + 1 point) | 0.82 | 0.71-0.94 | 0.005 |
| Support from co-workers (per + 1 point) | 0.84 | 0.69-1.01 | 0.06 |
| Job strain | 3.43 | 1.67-7.09 | 0.001 |
| Iso-strain | 5.96 | 2.73-13.0 | < 0.0001 |
| Self-reported burnout | 47.4 | 10.3-219 | < 0.0001 |
| Variables | High depersonalization | ||
| OR | 95% CI | p | |
| Daily contact with patients | 13.3 | 1.73-102 | 0.01 |
| Meeting patients’ families | 3.3 | 1.18-9.20 | 0.02 |
| Having to announce serious disease / death | 2.26 | 1.17-4.36 | 0.02 |
| Death of several patients | 2.39 | 1.13-5.06 | 0.02 |
| Working in a hospitalisation ward | 2.22 | 1.13-4.33 | 0.02 |
| Working at the weekend | 2.63 | 1.39-4.97 | 0.003 |
| 1 additional weekend worked per month | 1.42 | 1.08-1.86 | 0.01 |
| Presenteeism | 1.79 | 0.99-3.24 | 0.05 |
| Psychological demand (per + 1 point) | 1.14 | 1.07-1.22 | 0.0001 |
| Decision latitude (per + 1 point) | 0.97 | 0.94-1.00 | 0.05 |
| Freedom to make decisions (per + 1 point) | 0.94 | 0.90-0.99 | 0.03 |
| Job strain | 2.68 | 1.48-4.85 | 0.001 |
| Iso-strain | 2.97 | 1.42-6.20 | 0.004 |
| Variables | Low personal accomplishment | ||
| OR | 95% CI | p | |
| Meeting patients’ families | 0.35 | 0.15-0.82 | 0.02 |
| Working in consultations | 0.44 | 0.19-0.97 | 0.04 |
| Decision latitude (per + 1 point) | 0.95 | 0.92-0.99 | 0.005 |
| Exercise skills (per + 1 point) | 0.91 | 0.85-0.97 | 0.006 |
| Freedom to make decisions (per + 1 point) | 0.94 | 0.89-0.99 | 0.02 |
Table 4: Univariate analysis of risk factors associated with emotional exhaustion, high depersonalization and low personal accomplishment.
Risk factors for depersonalization were dominated by the relationship with the patients and their families. Daily contact with patients and meeting patients’ families were the greatest risk factors for depersonalization. Having to announce serious disease or death to families and the death of several patients during the semester were also risk factors for depersonalization. Working at the weekend increased this risk.
Protective factors against low personal accomplishment at work were observed among residents working in consultations and meeting patients’ families. These situations were conducive to exercising skills and making independent decisions.
Risk factors for burnout: Multivariate analysis
The results of the multivariate analysis identifying risk factors for burnout among the 191 respondents are shown in (Table 5). Increased psychological demand was associated with higher emotional exhaustion and depersonalization. Iso-strain and self-reported burnout were also independent risk factors for high emotional exhaustion. There was a strong association between working in a hospitalisation ward and a feeling of low personal accomplishment at work. Conversely, meeting patients’ families and greater decision latitude had a protective effect against feelings of low personal accomplishment. No other factors in the model were statistically significantly related to the presence of burnout.
| Variables | High emotional exhaustion | ||
|---|---|---|---|
| OR | 95% CI | p | |
| Psychological demand (per + 1 point) | 1.16 | 1.05-1.29 | 0.005 |
| Iso-strain | 3.25 | 1.29-8.22 | 0.01 |
| Self-reported burnout | 18.5 | 3.74-91.2 | 0.0003 |
| Variables | High depersonalization | ||
| OR | 95% CI | p | |
| Psychological demand (per + 1 point) | 1.14 | 1.07-1.22 | 0.0001 |
| Variables | Low personal accomplishment | ||
| OR | 95% CI | p | |
| Not meeting patients’ families | 11.7 | 3.08-44.4 | 0.0003 |
| Working in a hospitalisation ward | 3.66 | 1.30-10.3 | 0.01 |
| Decision latitude (per + 1 point) | 0.95 | 0.91-0.99 | 0.008 |
Table 5: Factors associated with burnout (as assessed by the MBI) by multivariate analysis.
Discussion
This study identified work-related risk factors associated with high scores on the components of burnout as assessed using the MBI among residents in medicine and surgery in the region of Champagne- Ardenne in France.
In its original form designed by Maslach et al. [2], the MBI does not allow the calculation of a single score to assess burnout, and the authors of the instrument recommend analysing the burnout phenomenon in its three separate component dimensions. This approach is more informative, and we therefore chose to describe the risk factors for each dimension of burnout in our study among a population of residents in medicine and surgery.
Limitations and potential bias
Among the 644 residents eligible for inclusion in this study, only 191 fully completed questionnaires were available for analysis, corresponding to a response rate of 29.7%. The response rate may have been affected by residents’ fears that the anonymity of the questionnaire might not be respected. Even among those who answered, some questions were left unanswered, probably to guarantee the anonymity of their responses. A second potential explanation for the response rate is that the distribution of the questionnaire among the residents of each specialty was done through a referent person. Between specialties, the distribution and access to the questionnaire varied. In particular, these two elements may explain the low rate of response among residents in surgery (only 12%). A third potential explanation is the finding that individuals affected by burnout generally tend to respond less frequently to surveys or questionnaires on the subject [14], thus leading to under-estimation of the prevalence of burnout. Our results should therefore be interpreted with caution as regards residents in surgery, whereas the potential for extrapolation of the results is greater among medical residents, with response rates of 43.5% and 25.7% in family medicine and other specialties, respectively.
Residents who were aware of the problems caused by suffering in the workplace and/or burnout, either through information received during their training, or through their personal and/or professional experience, likely responded more frequently to the questionnaire than their counterparts with lower awareness of burnout. This may have introduced potential for a selection bias. Lastly, the number of participants in each category of resident were very low, with the result that some findings could not be analysed (e.g. analysis by individual specialty or by number of semesters of residency already completed).
Emotional exhaustion
Some risk factors were more closely associated with specific dimensions of burnout. In the literature [15], as in our study, the factors associated with emotional exhaustion were mainly related to the workload (number of hours, weekends, night duties, presenteeism). Conversely, the factors associated with depersonalization tended to be more closely related to the actual job content, in particular interpersonal relations with the patients and their families. Indeed, it is through these interpersonal relations that the symptoms of depersonalization, such as cynicism, loss of empathy etc., are expressed.
In our study, the prevalence of high scores on the individual components of burnout was similar to that observed in a French study among residents in oncology [16] in particular as regards emotional exhaustion. In another French study among residents in family medicine [13], the prevalence of emotional exhaustion was lower, likely because 24% of the participants were performing their residency in a private general practitioner (GP) practice, mostly with a lighter workload than residents working in a hospital setting.
We noted a particularly high prevalence of depersonalization among the residents in our study of the Champagne-Ardenne region (41.9%). This component of burnout is associated with substantial morbidity. In one study of residents in the USA, depersonalization was the component that was most strongly related to suicidal thoughts, with an increase in suicidal ideation of 10% for each additional point on the depersonalization score [17]. To prevent depersonalization, changes to the work organisation should be envisaged with a view to reducing the workload on residents, giving them greater autonomy and the capacity to make decisions to develop their skills.
Karasek’s job content questionnaire
Karasek’s Job Content Questionnaire highlights the psychological and organisational constraints that are conducive to burnout, namely increased psychological demands, reduced decision latitude, and isostrain. In our study, we observed that job strain affected 42.4% of residents, which is higher than the rate reported among the general population in France. Indeed, the Sumer study performed in 2010 reported that 22% of employees suffered job strain [18], compared to 23% in 2003, of whom 26.1% worked in the health/social work sector [19].
In terms of the quadrant approach to job strain, the residents of the Champagne-Ardenne region are mainly situated at the borderline between the “active” quadrant and the “job strain” quadrant. A major challenge in this situation is to increase the decision latitude for residents, in order to avoid working conditions that put their health at risk. We show in our study that job strain is associated with an increased risk of emotional exhaustion and depersonalization (thus, of burnout), but other studies have also shown that exposure to job strain is a risk factor for cardiovascular disease and depression [20,21].
Presenteeism
To the best of our knowledge, this is the first study to evaluate the frequency of presenteeism among residents in medicine and surgery. Presenteeism was quite high in this population, with around 40% reporting that they had had some degree of presenteeism during the prior semester. Helping professions and hospital care settings seem to be most affected by the phenomenon of presenteeism [22]. One of the first studies of presenteeism was performed among doctors in Britain, and explained their tendency to go to work when they wer e actually ill by the fact that their tasks could neither be postponed nor delegated to other colleagues, who were likely already overburdened [23]. Yet, presenteeism is reportedly associated with impaired quality of care. Indeed, among nurses in North Carolina, USA, [24] reported that presenteeism was significantly associated with a higher number of patient falls, a higher number of medication errors, and lower qualityof- care scores.
In our study, presenteeism was significantly associated with a risk of emotional exhaustion. This is in line with the findings of Demerouti et al. [25] who reported that depersonalization was an outcome of presenteeism over time, whereas exhaustion and presenteeism were reciprocal. Emotional exhaustion is therefore not solely the consequence of a cumulation of professional risk factors, but can also arise from an at-risk personality and from certain behaviours, of which presenteeism is a symptom.
Recommendations for improving mental health among residents
Collective preventive measures are mandatory to ensure adequate mental health among physician trainees. Indeed, in the USA, Goldman et al. [26], published recommendations for a national response to counteract depression and suicide among trainee doctors. In particular, they proposed that residents should be better informed about stress in the workplace, its social consequences, and its repercussions on the health of both those affected, and the patients they care for. They further recommended that senior physicians should be alerted to the magnitude of the problem in order to help detect residents affected by burnout through the introduction of annual evaluation interviews to screen for addictive behaviours, depression or other psychiatric events. Lastly, the authors called for all residents to have access to local specialized mental health care where confidentiality would be guaranteed, as well as regular group meetings with their peers to discuss their work and the difficulties they encounter.
In France, it also appears necessary to implement a national response to counteract the extent of workplace stress among residents. The US recommendations issued by Goldman et al. could serve as a basis for further reflection in preventive medicine units, which are the cornerstone of prevention and management for residents with burnout. Improved understanding of the psychological and organizational constraints that can engender emotional exhaustion should lead to changes in organizational structures aimed at limiting workload, facilitating rotations between hospitalization wards and consultations, and increasing the level of autonomy accorded to residents. The future reform of the French national residency programme, scheduled to be introduced in September 2017, could represent an ideal opportunity to take these changes into consideration.
Conclusion
We observed that 62.8% of residents in medicine and surgery in the Champagne-Ardenne region presented at least one component of burnout as assessed by the MBI, while 42.4% were exposed to job strain, and 19.9% to iso-strain. The majority of residents in this region would therefore appear to be exposed to situations that pose a risk to their health. Working in a hospitalization unit, not meeting patients’ families, high psychological demands and iso-strain were risk factors for burnout identified by this study, whereas increased decision latitude had a protective effect.
Collective preventive measures are mandatory to ensure adequate mental health among physician trainees.
References
- Freudenberger HJ (1975) The staff burn-out syndrome in alternative institutions. Psychother-Theor Res 12: 73-82.
- Maslach C, Jackson SE (1981) The measurement of experienced burnout. J Organiz Behav 2: 99-113
- Ferreira Ndo N, de Lucca SR (2015) Burnout syndrome in nursing assistants of a public hospital in the state of São Paulo. Rev Bras Epidemiol 18: 68-79.
- Navarro-González D, Ayechu-DÃaz A, Huarte-Labiano I (2015) Prevalence of burnout syndrome and factors associated with this syndrome in primary care health professionals. Semergen-Med Fam 41: 191-198.
- Maite V, Muñoz CC, Pernas FO, Sureda JC, et al. (2015) Burnout and teamwork in primary care teams. Aten Prim 47: 25-31.
- Zanatta AB, de Lucca SR (2015) Prevalence of burnout syndrome in health professionals of an onco-hematological pediatric hospital. Rev Esc Enferm USP 49: 253-258.
- Lissandre S, Abbey-Huguenin H, Bonnin-Scaon S, Arsene O, Colombat P (2008) Factors associated with burnout syndrome in healthcare professionals in oncology and haematology departments. Oncology 10: 116-124.
- Veyssier-Belot C (2015) Burnout syndrome among physicians. Rev Med Interne 36: 233-236.
- Wallace JE, Lemaire JB, Ghali WA (2009) Physician wellness: A missing quality indicator. Lancet 374: 1714-1721.
- Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, et al. (2014) Quality of care and health professional burnout: Narrative literature review. Int J Health Care Qual Assur 27Â : 293-307.
- Prins JT, van der Heijden FMMA, Hoekstra-Weebers JEHM, Bakker AB, van de Wiel HB, et al. (2009) Burnout, engagement and resident physicians’ self-reported errors. Psychol Health Med 14: 654-666.
- Dominique A, Daviet L, Lourdais A (2013) Burnout of internal anesthesia-intensive care in France West region. Ann Fr Anesth 32(S1): A261
- Galam E, Komly V, Le Tourneur A, Jund J (2013) Burnout among French GPs in training: A cross-sectional study. Brit J Gen Pract 63: e217-e224.
- Taris TW, Schreurs PJ (2007) How may nonresponse affect findings in organizational surveys? The tendency-to-the-positive effect. Int J Stress Manage 14: 249-259.
- Lindblom KM, Linton SJ, Fedeli C, Bryngelsson IL (2006) Burnout in the working population: Relations to psychosocial work factors. Int J Behav Med 13: 51-59.
- Blanchard P, Truchot D, Albiges-Sauvin L, Dewas S, Pointreau Y, et al (2010) Prevalence and causes of burnout amongst oncology residents: A comprehensive nationwide cross-sectional study. Eur J Cancer 46: 2708-2715.
- Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, et al. (2008) Burnout and suicidal ideation among U.S. medical students. Ann Intern Med 149: 334-341.
- Amira S, Ast D (2014) Contrasting occupational risks according to the trades: SUMER 2010 survey. DARES Analyses 39: 1-17
- Guignon N, Niedhammer I, Sandret N (2008) SUMER 2003. Psychosocial factors at work. An evaluation by the Karasek questionnaire in the SUMER 2003 survey. Doc Med Trav 115: 389-398
- Belkic K, Landsbergis PA, Schnall PL, Baker D (2004) Is job strain a major source of cardiovascular disease risk? Scand J Work Env Hea 30: 85-128.
- Stansfeld SA, Shipley MJ, Head J, Fuhrer R (2012) Repeated job strain and the risk of depression: Longitudinal analyses from the Whitehall II study. Am J Public Health 102: 2360-2366.
- Aronsson G, Gustafsson K (2005) Sickness presenteeism: Prevalence, attendance-pressure factors, and an outline of a model for research. J Occup Environ Med 47: 958-966
- McKevitt C, Morgan M (1997) Illness doesn’t belong to us. J R Soc Med 90: 491-495.
- Letvak SA, Ruhm CJ, Gupta SN (2012) Nurses’ presenteeism and its effects on self-reported quality of care and costs. Am J Nurs 112: 30-38.
- Demerouti E, Le Blanc PM, Bakker AB, Schaufeli WB, Hox J (2009) Present but sick: A three-wave study on job demands, presenteeism and burnout. Career Development International 14Â : 50-68.
- Goldman ML, Shah RN, Bernstein CA (2015) Depression and suicide among physician trainees: Recommendations for a national response. JAMA Psychiatry 72: 411-412.
Citation: Deschamps F, Castanon J, Laraqui O, Manar N, Laraqui C, et al. (2018) Professional Risk Factors for Burnout among Medical Residents. J Community Med Health Educ 8:596. DOI: 10.4172/2161-0711.1000596
Copyright: © Deschamps F, Castanon J, Laraqui O, Manar N, Laraqui C, et al. (2018) Professional Risk Factors for Burnout among Medical Residents. J Community Med Health Educ 8: 596.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6000
- [From(publication date): 0-2018 - Nov 26, 2025]
- Breakdown by view type
- HTML page views: 5039
- PDF downloads: 961