Research Article Open Access
Right Versus Left Laparoscopic Donor Nephrectomy: Initial 3 year Experience from a Single Centre Transplant Program
McGregor TB1*, Clare E Gardiner1and Joshua Koulack2
1Section of Urology, University of Manitoba, Canada
2Section of Vascular Surgery, University of Manitoba, Canada
- *Corresponding Author:
- McGregor TB
Section of Urology, University of Manitoba
Canada
Tel: +1 800-432-1960
E-mail: tmcgregor2@sbgh.mb.ca
Received date: December 29, 2015; Accepted date: January 23, 2016; Published date: January 25, 2016
Citation: McGregor TB, Gardiner CE, Koulack J (2016) Right Versus Left Laparoscopic Donor Nephrectomy: Initial 3 year Experience from a Single Centre Transplant Program. Transplant Rep 1:102.
Copyright: © 2016 McGregor TB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Transplant Reports : Open Access
Abstract
Laparoscopic living donor nephrectomy is the standard of care at high volume transplant centers. Despite this there is still reticence to harvest the right kidney laparoscopically because of concerns regarding the shorter renal vein, higher complexity of dissection and potentially higher complication rates and worse renal allograft outcomes. The aim of this single-center study of 72 consecutive laparoscopic donor nephrectomies was to compare left versus right-sided laparoscopic donors in terms of surgical difficulty, complication rates and outcomes.There were 56 left-sided and 16 right-sided donors. There was no significant difference in surgical outcomes or complication rates. Similarly, the recipient surgery complication rates and allograft outcomes were no different between kidneys procured laparoscopically from the left or the right. This single center study shows comparable donor operative parameters and recipient post-operative outcomes in left and right laparoscopic donor nephrectomies. Procuring the right kidney laparoscopically is safe and does not have a negative impact on donor recovery or long term graft function in the recipient.
Keywords
Donor; Kidney transplantation; Laparoscopic nephrectomy
Abbreviations
LDN: Laparoscopic Donor Nephrectomy; ODN: Open Donor Nephrectomy; LLDN: Left-sided Laparoscopic Donor Nephrectomy; RLDN: Right-side Laparoscopic Donor Nephrectomy; AML: Angiomyolipoma; WIT: Warm Ischemic Time; EBL: Estimated Blood Loss; LOS: Length of Stay; LKR: Left Kidney Recipient; RKR: Right Kidney Recipient; STEMI: ST-Elevation Myocardial Infarction; DVT: Deep Venous Thrombosis; DGF: Delayed Graft Function
Introduction
Laparoscopic donor nephrectomy (LDN) has been the preferred method of kidney donation since the technique was first introduced in 1995 [1]. The laparoscopic approach offered many benefits over open donor nephrectomy (ODN) including shorter length of stay, less post-op pain, quicker return to work, and similar donor and allograft outcomes long-term [2,3]. The decreased morbidity and improved cosmetics offered by the laparoscopic approach also attracted more donors and improved live kidney donation rates [4,5].
Left sided laparoscopic kidney donation has always been more preferable compared to right sided donation. The main reason for this has been the significantly greater length offered by the left renal vein compared to the short right renal vein. The longer length of the left vein facilitates an easier venous anastomosis in the recipient potentially decreasing recipient operative time and venous anastomotic complication rates, such as venous thrombosis [6,7]. Due to these concerns and despite many centers continuing to offer right sided LDN, significant reticence still exists regarding its use. For this reason we sought out to review our initial three year experience at laparoscopic donor nephrectomy to compare differences in left versus right sided approaches in terms of technical difficulty, donor outcomes and complications and allograft function.
Methods
We reviewed the clinic and operative reports on 72 consecutive LDN cases performed at our institution between May 2011 and July 2014. Of these 72 cases we identified 56 as left sided laparoscopic donor nephrectomy (LLDN) and 16 as right sided laparoscopic donor nephrectomy (RLDN). All patients underwent similar preoperative workup including assessment by both the surgical and medical transplant teams and abdominal imaging with CT-angiography to assess renal and vascular anatomy. We then compared these two groups regarding several peri-operative parameters, including: pre and postop renal function, intra-operative complications, postoperative complications, hospital stay, recipient operative time and complications and allograft outcome.
Prism Graph Pad Software (v6) was used for all statistical analyses. Unpaired t-tests were performed for continuous variables and Fisher’s exact tests were performed for categorical variables. A p value of <0.05 was considered statistically significant.
All donor procedures were performed by a pure laparoscopic technique with no hand-assist. All left sided donors utilized a threeport approach whereas right-sided donors required an extra 5 mm port for liver retraction Figure 1. Vascular control was performed using an endovascular stapler for both the artery and the vein regardless of the side. Kidneys were removed through a mini-Pfannenstiel incision regardless of the side of the kidney. Post-operative pathways were standardized and consisted of early mobilization and diet progression and pain control by patient controlled analgesia for 24 hours followed by conversion to oral analgesics.
Results
Our analysis included 72 consecutive LDN cases including 56 LLDN and 16 RLDN patients. Patient demographics are summarized in Table 1. There was no statistical difference in donor gender, age or BMI between LLND and RLDN groups. Reasons for selecting the right kidney for donation were: multiple left renal arteries (13 patients), calcification present at the take off of the right renal artery (1 patient) thereby leaving the healthier kidney with the donor, right kidney was smaller (1 patient) more suitable for a pediatric recipient and leaving the larger kidney for the donor, and an AML was present in the right kidney (1 patient) which was resected ex-vivo prior to transplantation. There was no significant difference in donor intraoperative and perioperative parameters including estimated blood loss (EBL), warm ischemic time (WIT) or length of stay in hospital (LOS), as summarized in Table 2. Mean donor EBL was 59.96 ± 11.45 ml for LLDN and 46.13 ± 14.95 ml for RLDN patients. Mean donor WIT was 2 minutes for both LLDN and RLDN patients. Mean donor LOS was 2.21 ± 0.08 days for LLDN and 2.13 ± 0.17 for RLDN patients. Donor postoperative complications included testicular pain (3 LLDN), nausea (1 LLDN), DVT/PE (1 LLDN), wound infection (1 LLDN, 1 RLDN), pneumothorax repaired laparoscopically (1 LLDN) and splenic laceration repaired laparoscopically (2 LLDN). All complications were Clavien-Dindo grade 1 or 2 (Table 3). There was no significant difference in complication rates between LLDN and RRDN patients (p=0.67). Donor creatinine at 6 weeks post-operatively was 111.70 ± 2.95 μmol/L for LLDN and 97.56 ± 4.64 μmol/L for RLDN patients and was significantly different (p=0.02), although clinically insignificant.
| LLDN(n = 56) | RLDN(n = 16) | p values | |
|---|---|---|---|
| Donor | |||
| Sex(M:F) | 18:38 | 3:13 | 0.37 |
| Age(Years) | 45.31 ± 1.84 | 46.25 ± 3.07 | 0.8 |
| BMI(Kg/m2) | 26.45 ± 0.43 | 25.34 ± 0.88 | 0.23 |
| Recipient | |||
| Sex(M:F) | 30:26:00 | 6:10 | 0.4 |
| Age(Years) | 47.50 ± 1.99 | 40.81 ± 4.92 | 0.15 |
| BMI(Kg/m2) | 27.28 ± 0.92 | 24.36 ± 1.19 | 0.14 |
Table 1: Donor and recipient demographic characteristics. Values are mean ± SD.
| LLDN | RLDN | p values | |
|---|---|---|---|
| EBL (ml) | 59.96 ± 11.45 | 46.13 ±14.95 | 0.54 |
| WIT (min) | 2.07 ± 0.06 | 2.00 ± 0.0 | 0.5 |
| LOS (days) | 2.21 ± 0.09 | 2.13 ± 0.17 | 0.66 |
Table 2 : Donor intraoperative and perioperative parameters. Values are mean ± SD.
| LLDN | RLDN | |
|---|---|---|
| Grade 1 | ||
| Testicular pain | 3 | 0 |
| Nausea | 1 | 0 |
| Pneumothorax | 1 | 0 |
| Splenic laceration | 2 | 0 |
| Grade II | ||
| Wound infection | 1 | 1 |
| Total (p=0.67) | 8 | 1 |
Table 3: Laparoscopic donor nephrectomy complications.
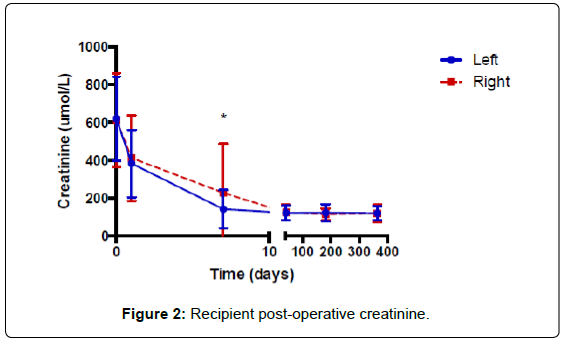
With regard to the renal allograft recipients, there was no significant difference in recipient gender, age or BMI between recipients of left (LKR) or right kidneys (RKR) Table 1. Post-operative creatinine was analyzed in the recovery room and at 1 day, 7 days, 6 weeks, 6 months and 12 months post-operatively Figure 2. Creatinine was significantly different only at 7 days post-operatively (p=0.05) and was not significantly different at any other time point in the dataset. Recipient short-term post-operative complications included blood transfusion (3 LKR), wound dehiscence (1 LKR), STEMI (2 LKR), DVT (1 LKR), lymphocele (1 LKR), peri-renal hematoma (2 RKR), and urosepsis (1 RKR). Clavien-Dindo grades for short-term recipient complications included grade 1 to grade 5 Table 4. There was no significant difference in rate of overall short-term recipient complications (p=0.71). Recipient long-term complications included renal artery stenosis with angioplasty (3 LKR), perinephric abscess (1 LKR), DVT/PE (1 LKR, 2 RKR), incisional hernia (2 LKR), ureteric stricture (2 LKR, 1 RKR), BK virus nephritis (1 LKR), urosepsis (2 LKR), pyelonephritis (1 RKR), primary disease recurrence (1 LKR), post-transplant lympho proliferative disorder (1 RKR) and wound infection (1 RKR). Clavien-Dindo grades for long-term recipient complications included grade 1 to grade 4a Table 5. There was no significant difference in rate of overall long-term recipient complications (p=48). Recipient delayed graft function (DGF) was significantly different (p=0.01) with 3 DGF episodes occurring in LKR and 4 DGF episodes occurring in RKR. There were 3 recipient mortalities. One occurred at 4 days post-transplant from a myocardial infarction, one at 4 months post-transplant from CMV sepsis and one at 2 years post-transplant from a myocardial infarction.
| LLDN | RLDN | |
|---|---|---|
| Grade 1 | ||
| Lymphocele | 1 | 0 |
| Grade II | ||
| Transfusion | 3 | 0 |
| DVT | 1 | 0 |
| Wound dehiscence | 1 | 0 |
| Urosepsis | 0 | 1 |
| Grade III-a | ||
| STEMI | 1 | 0 |
| Grade III-b | ||
| Post-op hematoma | 0 | 2 |
| Grade V | ||
| STEMI | 1 | 0 |
| Total (p=0.71) | 8 | 3 |
Table 4 : Short-term renal allograft recipient post-operative complications.
| LLDN | RLDN | |
|---|---|---|
| Grade I | ||
| RAS + angioplasty | 1 | 0 |
| Incisional hernia | 1 | 0 |
| Grade II | ||
| BK virus nephritis | 1 | 0 |
| DVT/PE | 1 | 2 |
| Pyelonephritis | 0 | 1 |
| Urosepsis | 2 | 0 |
| Wound infection | 0 | 1 |
| Grade III-a | ||
| RAS + angioplasty | 2 | 0 |
| Ureteric stricture | 2 | 1 |
| Perinephric abscess | 1 | 0 |
| Grade III-b | ||
| Incisional hernia | 2 | 0 |
| Grade IV-a | ||
| Dialysis | 1 | 0 |
| PTLD | 0 | 1 |
| Total (p = 0.48) | 14 | 6 |
Table 5: Long-term renal allograft recipient post-operative complications.
Discussion
As the disparity between supply and demand for renal allografts continues to grow, the need to maximize the living donor pool is imperative. This translates into the importance of utilizing right-sided donors when anatomy or conditions contradict left sided donation. However, some centers still have reservations to procurement of rightsided kidneys laparoscopically, thus depriving right-sided donors of the benefits of laparoscopy (if done by open technique) or preventing that donor from contributing to the kidney pool (if the donor is turned down). Despite the perceived technical difficulties of RLDN our results show that RLDN appears to be as safe and efficacious as the historically favored LLDN approach; this is in keeping with reports in the literature that show similar results [4,6-7].
In our review we demonstrate that intra-operative and postoperative outcomes are similar regardless of the side of laparoscopic kidney retrieval. There were no significant differences in donor surgery parameters including similar EBL and WIT.
The post-operative outcomes were also similar, including no difference in the LOS and renal function at 6 weeks post-op for both right and left sided donors. Overall there were no major complications in either donor group and no significant difference in the complication rate between LLDN and RLDN.
Early on in the laparoscopic donor nephrectomy era, several groups reported higher complication rates and worse outcomes for kidneys retrieved from the right side. Specifically, reports of complications regarding the short right renal vein and vascular anastomosis were cited. In more recent series, including our own reported here, we did not notice any difference in complication rates or outcomes for kidneys retrieved from either side. Perhaps this change represents an improvement in the laparoscopic technique with time, and improvements in the laparoscopic instrumentation and technology. For example, improved energy sources and also stapling devices likely allow for easier dissection and management of the short right renal vein as it branches off the vena cava [8].
In our series the RLDN cohort all consist of a pure-laparoscopic technique while other series in the literature utilize a combination of pure-laparoscopic and hand-assisted. Although arguments have been made that hand-assist facilitates an easier right renal and caval dissection [9], we did not notice any hindrances utilizing a purelaparoscopic technique. Also, despite the extra port needed to perform the RLDN we did not notice any difference in peri-operative morbidity between the two groups.
In regards to the recipient outcomes, our series shows no difference in peri-operative parameters for the recipient, complication rate, and renal function outcomes. Specifically, recipients of kidneys harvested from the right side did not see more venous or vascular complications related to the short renal vein. Again, this is similar to other reports in the literature.
This study has inherent limitations, including its retrospective nature and the fact that it represents a single surgeon’s experience from a single center. However, the ability to perform a randomized controlled trial to look at left vs. right sided donors will never happen, and we feel this retrospective case series represents a real-life glance at the use of right sided kidney donors in an era were there still are some centers throughout North America with reluctance to perform right sided donors laparoscopically.
It is now clear that the gold standard for kidney donation utilizes a minimally invasive technique. Despite previous reservations in regards to the laparoscopic approach for right-sided kidneys, our series adds to the growing literature in support of the safety and efficacy of rightsided laparoscopic kidney donation.
References
- Ratner, et al., (1995) Laparoscopic live donor nephrectomy. Transplantation.
- Ratner LE, Montgomery RA, Kavoussi LR (2001) Laparoscopic live donor nephrectomy: a review of the first 5 years .UroloCliin North Am 28:709-19.
- Fonouni H, Mehrabi A, Golriz M, Zeier M, Müller-Stich BP, et al., (2014)Comparison of the laparoscopic versus open live donor nephrectomy: an overview of surgical complications and outcome. Langenbecks Arch Surg 399:543-551.
- Turk IA, Deger S, Davis JW, Giesing M, Fabrizio MD, et al.(2002)Laparoscopic live donor right nephrectomy: a new technique with preservation of vascular length. J Urol.
- Gupta, et al., (2005) Laparoscopic donor nephrectomy. J Minim Access Surg.
- Buell JF,Edye M,Johnson M,Li C, Koffron A,et al. (2001)Are concerns over rightlaparoscopic donor nephrectomy unwarranted? Ann Surg
- Mandal AK, Cohen C, Montgomery RA, Kavoussi LR, Ratner LE (2001) Should the indications for laparoscopic live donor nephrectomy of the right kidney be the same as for the open procedure? Anomalous left renal vasculature is not a contraindication to laparoscopic left donor nephrectomy. Transplantation.
- Bernie JE, Sundaram CP, Guise AI (2006)Laparoscopic Vascular Control Techniques in Donor Nephrectomy: Effects on Vessel Length. JSLS:Journal of the Societyof Laparoendoscopic Surgeons 10:141-144.
- Wang DS, Bird VG, Winfield HN, Rayhill S (2004) Hand-Assisted Laparoscopic Right Donor Nephrectomy: Surgical Technique. J Endourol18:205-09
Relevant Topics
- Allografts Transplant Reports
- Bone Marrow Transplant Reports
- Brain Transplant Reports
- Corneal Transplant Reports
- Eye Transplant Reports
- Eyebrow Transplant Reports
- Hair Transplant Reports
- Head Transplant Reports
- Heart Transplant Reports
- Individual Organ Transplants
- Kidney Transplant Reports
- Liver Transplant Reports
- Lung Transplant Reports
- Pancreatic Transplantation
- Stem Cell Transplant Reports
Recommended Journals
Article Tools
Article Usage
- Total views: 24622
- [From(publication date):
June-2015 - Aug 23, 2025] - Breakdown by view type
- HTML page views : 23605
- PDF downloads : 1017