Research Article Open Access
Serum Creatinine and Weaning in Patients with Chronic Obstructive Pulmonary Disease: Multicenter Pilot Study
Özlem Yazicioglu Moçin1*, Zuhal Karakurt1, Elif Sen2, Gökay Güngör1, Hilal Altinöz1, Begüm Ergan Ersava3, Murat Yalçinsoy1, Ayse Yalçin2, Nalan Adigüzel1, Akin Kaya4 and Arzu Topeli3
1Respiratory intensive care unit Sureyyapasa Chest Diseases and Thoracic Surgery Training and Research Hospital, Istanbul-Turkey
2Medical Intensive Care Unit of Ankara University Faculty of Medicine, Ankara- Turkey
3Medical Intensive Care Unit of Hacettepe University, Faculty of Medicine, Ankara-Turkey
4Pulmonary Department of Ankara University Faculty of Medicine, Ankara-Turkey
- *Corresponding Author:
- Özlem Yazicioglu Moçin, MD
Respiratory intensive care unit Sureyyapasa Chest Diseases
and Thoracic Surgery Training and Research Hospital, Istanbul-Turkey
Tel: 00905326466590
Fax: 0090 216 4214031
E-mail: drozyaz@yahoo.com
Received date March 02, 2013; Accepted date March 20, 2013; Published date March 23, 2013
Citation: Moçin ÖY, Karakurt Z, Sen E, Güngör G, Altinöz H, et al. (2013) Serum Creatinine and Weaning in Patients with Chronic Obstructive Pulmonary Disease: Multicenter Pilot Study. J Palliative Care Med 3:143. doi:10.4172/2165-7386.1000143
Copyright: © 2013 Moçin ÖY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Keywords
Creatinine; Weaning; Mechanical Ventilation; Chronic Obstructive Pulmonary Disease
Introduction
Non-invasive mechanical ventilation (NIV) is a gold standard for acute respiratory failure (ARF) in patients with chronic obstructive pulmonary disease (COPD) [1]. When NIV fails, invasive mechanical ventilation (IMV) is required in COPD.
During the International Consensus Conference Brochard proposed a new weaning classification of patients into three groups according to the difficulty and length of the weaning process [2]. Although the NIV success rate is very high in COPD, when NIV fails or is contra-indicated, weaning from mechanical ventilation can be a problem [3]. Therefore, taking potentially prolonged ventilation and weaning difficulties into account, intensivists hesitate to intubate COPD patients. Successful weaning has been attributed to a number of factors, as stated in guidelines, including nutritional status and muscle strength [2-5]. The role of respiratory muscle is very important in COPD patients during the weaning process [3].
Serum creatinine can provide indirect information on body muscle mass. Oterdoom et al. report that low creatinine excretion in the urine is an indirect measure of low muscle mass (with normal renal function) and is associated with major adverse cardiovascular events [6].
An acute increase in serum creatinine originates from muscle destruction due to drug-induced muscle atrophy [7]. Serum creatinine is low in patients with whole body muscle wasting or atrophies [8]. Thus, we can speculate that invasively ventilated patients with low serum creatinine, especially during the weaning period, may have muscle wasting and atrophy. In addition, blood urea nitrogen (BUN) levels are elevated by the catabolism of lean body mass [5], and lower levels of BUN may be a marker of the cessation of catabolism, which is necessary for respiratory muscle recovery and a good predictor of weaning [9].
We hypothesized that COPD patients with low serum creatinine levels on the first day of weaning would most likely not be successfully weaned because of inadequate muscle strength.
Methods
Design and settings
This multicenter, retrospective cohort pilot study was conducted in three centers. One center, a 14-bed respiratory intensive care unit (ICU) in a big government respiratory training and research hospital, was in Istanbul, while the others were medical faculties in Ankara; one was a six-bed ICU for patients with respiratory failure, the other was a ten-bed medical ICU. The study was conducted from June 1st, 2007 to June 30th, 2008.
The study was approved by our local ethical committee.
Patient recruitment
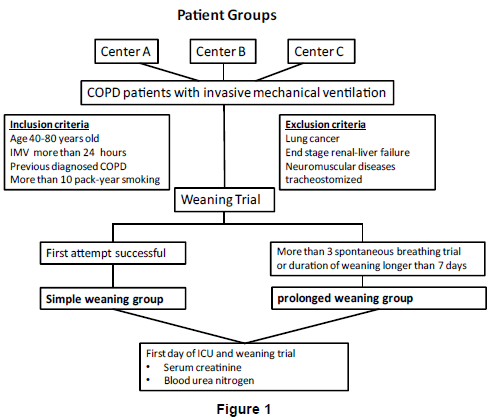
All consecutive, previously diagnosed, COPD [1] patients with ARF who, either failed a first attempt of NIV, or who had contraindications for NIV [10], and were intubated for IMV for more than 24 h, were enrolled into the study. We excluded patients with chronic renal disease or acute renal failure requiring hemodialysis, or those who had a tracheostomy (Figure 1).
Weaning process
The following criteria had to be met before weaning was attempted: 1) An improvement in the precipitating factors of ARF, 2) hemodynamic stability (heart rate [HR] less than 140 beats-min-1, systolic blood pressure [BP] between 90-160 mmHg, no or minimal vasopressors), 3) stable metabolic status, 4) adequate oxygenation (oxygen saturation rate [SatO2%] more than 90% on ≤ fractionated inspirated oxygen [FiO2] of 0.40 or PaO2/FiO2 more than 150), 5) positive expiratory end pressure (PEEP) ≤ 8 cm H2O, 6) adequate pulmonary function (breath per minute [fR] less than 35, tidal volume [VT] 0.5 mL-kg-1, rapid shallow breathing index [fR/VT] less and equal to 105 breaths-min-1-L-1), 7) no significant respiratory acidosis, and 8) adequate mentation without sedation or adequate mentation on sedation (i.e., stable neurological patient). All three institutions followed the same weaning protocol. All weaning was conducted by experienced ICU physicians and initiated in the morning. When patients met the criteria for weaning the pressure support ventilation (PSV) was gradually decreased (1-2 cm H2O every 1-2 hours). When the PS reached 8-10 cm H2O and PEEP was 0 or less than 5 cm H2O, the patient progressed to spontaneous breathing trials (SBT) by T-piece with oxygen support [4]. Duration of the T-piece trial was 30 minutes. During this period the patient was observed directly by the ICU physicians and nurses.
The failure criteria for the T-piece trials were as follows: 1) Clinical assessment and subjective indices, i.e., agitation and anxiety, depressed mental status, diaphoresis, cyanosis, evidence of increasing effort, increased accessory muscle activity, facial signs of distress, and dyspnea. 2) Measurements such as arterial blood gases (ABGs); PaO2 ≤ 50–60 mmHg on FiO2 ≥ 0.5 or SaO2 less than 90%, PaCO2>50 mmHg or an increase in PaCO2 more than 8 mmHg, fR/VT>105 breaths min-1 L-1, fR>35 breaths min-1 or increased by ≥ 50%, HR>140 beats min-1 or increased by ≥ 20%, systolic BP>180 mmHg or increased by ≥ 20%, systolic BP<90 mmHg, and cardiac arrhythmias. Patients were extubated after 30 min of a successful T-piece trial. After extubation, NIMV was applied in cases of moderate respiratory distress if no contra-indication existed [4].
Definitions of weaning
Pre-weaning period: the time (hours) from intubation to the beginning of weaning.
Successful weaning (simple weaning): successful extubation after the first T-piece trial.
Unsuccessful weaning: failed extubation after more than one T-piece trial.
Prolonged ventilation: mechanical ventilation for more than seven days, or three or more T-piece trials.
Patients were divided into two groups based on their weaning success.
Simple weaning group (SWG): weaning was successful at the first weaning attempt.
Prolonged weaning group (PWG): weaning failed at the first attempt of the weaning trial, or death under IMV. We further divided patients according to their serum creatinine levels on the first day in ICU and the first day of the weaning trial. These were classified as low serum creatinine and normal to high creatinine according to the normal limits for females and males.
Data records
All records were collected retrospectively. Age, gender, smoking habits, co-morbidities (e.g. diabetes, cardiac disease), body mass index (BMI, kg/m2), arterial blood gas analysis on admission to the ICU, recent/current medications including bronchodilators, steroids (systemic/inhaler), and sedatives, were recorded. The cause of ARF was defined as hypercapnic respiratory failure (PaCO2 more than 45 mmHg) without hypoxemia; hypoxemic and hypercapnic respiratory failure were defined as PaCO2>45 mmHg and PaO2/FiO2<300. As an ICU severity score, the acute physiological and chronic health evaluation (APACHE) II was recorded on admission to the ICU [11]. Serum creatinine and BUN were recorded on the first day of ICU, and the first and seventh day of the weaning trial. The BUN/creatinine ratio was calculated to compare weaning groups with respect to hypercatobolic state, as described previously [9]. Blood glucose, sodium, potassium, hematocrit, and C-reactive protein levels on admission to the ICU were recorded from the patient’s file. The duration of mechanical ventilation, ICU length of stay, and ICU outcome (mortality), were also recorded from the data.
Statistical analyses
Data for continuous variables (i.e., age, body mass index, BUN, creatinine, BUN/creatinine, arterial blood gas values, APACHE II scores, and length of ICU stay) are presented as the mean ± standard deviation (SD) for normal distrubution, and the median (inter quartile ratio, 25%-75%) for non-normal distrubution. We used the student t-test to compare groups if the values were well distrubuted, and if not the Mann-Whitney-U test was performed. To compare data of categorical variables (i.e., gender, presence of tracheostomy), the chisquare test was used. A p value < 0.05 was accepted as significant.
Results
In the study period 85 of 96 COPD patients (19 female) were enrolled from three centers. Patients were divided into two groups according to the weaning trials, as described in the Methods. Patient demographics and ICU data are summarized in table 1.
| SWG | PWG | p values | |
|---|---|---|---|
| Patient demographics | |||
| Gender, Female/male | 7/29 | 12/37 | 0.58 |
| Age, years, mean (SD) | 67 (11) | 68 (9) | 0.76 |
| Body mass index* kg/m2, mean (SD) | 25.1 (5.5) | 24.6 (7.6) | 0.76 |
| Reasons of acute respiratory failure | |||
| Hypercapnia and hypoxemia, n(%) | 28 (77.8) | 40 (81.6) | 0.66 |
| Hypercapnia, n(%) | 8 (22.2) | 9 (18.4) | |
| Co-morbid diseases, | |||
| Diabetes mellitus, n(%) | 6 (16.7) | 11 (22.4) | 0.51 |
| Heart diseases, n(%) | 27 (75.0) | 34 (69.4) | 0.57 |
| Bronchiectasis, n(%) | 5 (13.9) | 7 (14.3) | 0.95 |
| Arterial blood gases on admission) | |||
| pH, median (IQR) | 7.28 (7.20-7.32) | 7.28 (7.19-7.34) | 0.95 |
| PaCO2, mmHg, mean (SD) | 77.0 (22.5) | 85.0 (28.3) | 0.16 |
| PaO2/FiO2 mmHg, median (IQR) | 218 (167-284) | 221 (161-268) | 0.87 |
| Biochemistry | |||
| Hematocrit %, mean (SD) | 42.9 (7.0) | 42.8 (7.1) | 0.96 |
| Glucose mg/dL, mean (SD) | 136 (39) | 139 (64) | 0.84 |
| Sodium mmol/L, mean (SD) | 138 (6) | 139 (6) | 0.37 |
| Potassium mmol/L, mean (SD) | 4.4 (0.6) | 4.5 (0.9) | 0.84 |
| C-reactive protein# mg/dL, median (IQR) | 42.3 (10.2-100.0) | 35.4 (18.4-99.0) | 0.81 |
| APACHE II mean (SD) | 22.6 (5.7) | 23.0 (7.1) | 0.79 |
Non-parametric continuous values are shown as median (interquartile ratio= IQR). The Mann Whitney U test was used and parametric continuous values are shown as mean (SD). The student-t test was also used. P<0.05 was accepted as statistically significant. SWG: simple weaning group, PWG: prolonged weaning group, PaCO2: arterial partial carbon dioxide pressure, PaO2/FiO2: arterial partial oxygen pressure over inspired fractionated oxygen, *body mass index available for 27 patients in the SWG, 34 in the PWG, #C-reactive protein available for 31 patients in the SWG, and 37 in the PWG. APACHE II: Acute physiologic and chronic health evaluation (11).
Table 1: Patient demographics and arterial blood gases and biochemistry on admission to the intensive care unit.
Table 2 shows the relationship between the patient groups and ICU data (IMV, sedation, tracheostomy, need for home MV, length of ICU stay, and mortality). The pre-weaning period and length of ICU stay were longer in the PWG group compared with the SWG group (p<0.004 and p<0.001, respectively). Mortality rate was similar but there were more patients discharged to home with a tracheostomy and home ventilators in the PWG than the SWG group (p<0.004 and p<0.020, respectively).
| Variables | SWG, n=36 | PWG, n=49 | p values |
|---|---|---|---|
| Mechanical ventilation, median (IQR) | |||
| Pre-weaning MV duration, hours | 71 (33-99) | 103 (49-175) | 0.004 |
| Duration of midazolam, hours | 29 (22-72) | 51 (20-84) | 0.40 |
| Total midazolam doses, mg | 60 (23-115) | 57 (18-160) | 0.75 |
| ICU length of stay, day median (IQR) | 9 (5-14) | 15 (11-24) | 0.001 |
| Discharge from ICU | |||
| Ward, n (%) | 33 (91.7) | 16 (32.7) | 0.001 |
| Home via non-invasive ventilators, n (%) | 2 (5.6) | 12 (24.5) | 0.020 |
| Tracheostomy, n (%) | 0 | 10 (20.4) | 0.004 |
| Mortality % | 2.8 (n=1) | 12.2 (n=6) | 0.23 |
Non-parametric continuous values are shown as median (IQR: interquartile ratio). The Mann Whitney U test was also used. P<0.05 was accepted as statistically significant. SWG: simple weaning group, PWG: prolonged weaning group, ICU: intensive care unit.
Table 2: Patient ICU data and outcomes.
The relationship between the patient groups and BUN, creatinine, and BUN/creatinine ratio on first day of ICU, and the first and seventh day of the weaning trial are summarized in table 3. Serum creatinine on the first and seventh day of the weaning trial was significantly lower in the PWG group compared with the SWG group (p<0.003 and p<0.012, respectively).
| Variables | SWG, n=36 | PWG, n=49 | p values |
|---|---|---|---|
| Serum Creatinine | |||
| First day of ICU, mean (SD) | 1.08(0.36) | 0.99 (0.51) | 0.36 |
| First day of weaning trial, mean (SD) | 0.94 (0.29) | 0.78 (0.0.37) | 0.035 |
| Seventh day of weaning trial* median (IQR) | 0.80 (0.70-1.07) | 0.58 (0.48-080) | 0.012 |
| Serum blood urea nitrogen (BUN) | |||
| First day of ICU, median (IQR) | 30 (21-37) | 26 (18-42) | 0.73 |
| First day of weaning trial, median (IQR) | 25 (19-35) | 18 (11-31) | 0.034 |
| Seventh day of weaning trial*, median (IQR) | 14 (11-23) | 13 (10-21) | 0.52 |
| BUN/serum creatinine | |||
| First day of ICU, median (IQR) | 28 (19-38) | 32 (20-48) | 0.21 |
| First day of weaning trial, mean (SD) | 30.3 (12.7) | 31.4 (17.2) | 0.74 |
| Seventh day of weaning trial*, mean (SD) | 19.9 (7.9) | 26.6 (15.7) | 0.07 |
Non-parametric continuous values are shown as median (interquartile ratio=IQR) The Mann Whitney U test was used and parametric continuous values are shown as mean (SD). The student-t test was also used. P<0.05 was accepted as statistically significant. SWG: simple weaning group, PWG: prolonged weaning group, *n: 11 for SWG, n: 36 for PWG.
Table 3: Patient serum creatinine and blood urea nitrogen levels.
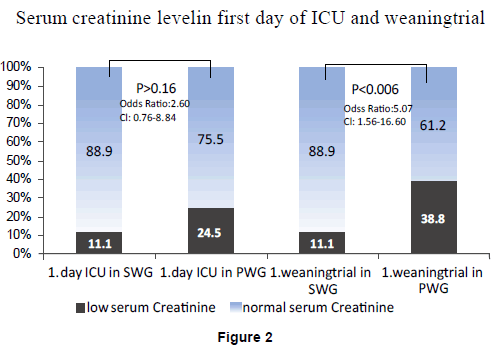
Table 4 shows patient’s BMI, ICU severity score, C-reactive protein on admission to the ICU, BUN/creatinine, pre-weaning duration, and length of ICU stay in the two patient groups relative to serum creatinine on the first day of ICU and the first day of the weaning trial. The percentage of patients in the low and normal creatinine groups on the first day of ICU and the first day of weaning are shown in figure 2. There were significantly more patients with lower creatinine levels in the PWG compared with the SWG (p<0.006).
| Variables | On the admission day to ICU | On the first day of the weaning trial | ||||
|---|---|---|---|---|---|---|
| Serum creatinine level | Serum creatinine level | |||||
| Low | Normal to higher | p | Low | Normal to higher | p | |
| Body mass index, kg/m2* | 19.2 (3.9) | 26.1 (6.6) | 0.002 | 24.2 (9.0) | 25.2 (5.4) | 0.66 |
| APACHE II on admission* | 19 (4) | 24 (7) | 0.011 | 20 (18-24) | 23 (19-28) | 0.025 |
| APACHE II at discharge* | 13 (5) | 14 (4) | 0.92 | 13 (4) | 14 (5) | 0.51 |
| C-reactive protein on admission to ICU, mg/dL* | 36 (9-80) | 43 (14-106) | 0.50 | 47 (26-99) | 35 (10-100) | 0.24 |
| PaO2/FiO2 on admission to the ICU* | 248 (119) | 230 (97) | 0.50 | 238 (101) | 231 (101) | 0.78 |
| BUN, mg/dL* | 22 (12) | 35 (22) | 0.023 | 22 (10) | 37 (23) | 0.001 |
| Serum creatinine mg/dl * | 0.52 (0.08) | 1.15 (0.43) | 0.001 | 0.66 (0.02) | 1.17 (0.45) | 0.001 |
| BUN/serum creatinine* | 37.2 (14.2) | 33.6 (14.4) | 0.53 | 33.8 (17-33) | 34.5 (21.5) | 0.88 |
| Assist/Control mod, preweaning hour# | 77 (49-134) | 82 (40-120) | 0.88 | 98 (63-138) | 72 (35-108) | 0.07 |
| Length of ICU stay, day# | 15 (11-23) | 12 (6-19) | 0.18 | 15 (12-21) | 11 (5-20) | 0.031 |
*Parametric continuous values are shown as mean (SD). Analyses were done with the Mann Whitney U test and # nonparametric continuous values are shown as median (interquartile ratio). The student-t test was also used. P<0.05 was accepted as statistically significant. ICU: intensive care unit, APACHE II: Acute physiologic and chronic health evaluation (11), PaO2/FiO2: arterial partial oxygen pressure over inspired fractionated oxygen, BUN: blood urea nitrogen.
Table 4: Patient characteristics, blood urea nitrogen (BUN), BUN/creatinine and ICU data in serum creatinine groups.
Discussion
In the present study our hypothesis that low serum creatinine may indicate a longer duration of ventilation weaning in COPD patients as a result of muscle wasting/atrophy, was supported. There were significantly more patients with low serum creatinine in the PWG compared with the SWG, even though they had similar APACHE II scores, and other factors (sedation doses and duration, co-morbidities, BMI), that might affect the success of a weaning trial.
COPD and weaning
The present study was performed in COPD patients to assess serum creatinine as an easy, quick, cheap, and reproducible test to predict weaning outcome. Non-invasive and invasive mechanical ventilation, and the weaning process are nearly standardized all over the world with consensus and guidelines [4,10]. Weaning from mechanical ventilation is complicated in intubated patients particularly those with COPD due to ARF [10]. In the present study, the majority of patients had both hypercapnic and hypoxemic respiratory failure. A previous study showed weaning success to be highest in post-operative patients (58%), and those with acute lung injury (57%), and lowest in patients with COPD or neuromuscular disease (22%) [2]. However the weaning success of our COPD patients was 42.4% in the first weaning trial. A longer duration of mechanical ventilation is an important risk factor for morbidity and mortality and the long-term survival rate after successful weaning is worse in patients with severe COPD compared with non-COPD patients [12]. Similarly, we found a longer duration of pre-weaning mechanical ventilation, and a five times higher mortality in the PWG compared with the SWG.
Creatinine, BUN, BUN/creatinine
In the present study COPD patients with a low creatinine level on admission to the ICU had a significantly lower body mass index. We showed a further decrease in the creatinine levels of patients with COPD as time passed in the ICU. This can be explained by the continuous catabolism and lesser amounts of muscle tissue to increase serum creatinine levels. We showed that on the day of the weaning trial, COPD patients with lower serum creatinine had higher levels of C-reactive protein than patients with normal serum creatinine. The group with lower serum creatinine spent longer in the ICU, although the ICU severity scores were similar in both groups. This can be attributed to muscle wasting/atrophy and muscle weakness in the patients with COPD due to the severity of inflammation. Muscle cells can be affected by C-reactive protein and other cytokines (IL-1, IL6, TNF) generated in response to systemic inflammation/infection, especially during COPD exacerbation [13-17]. In the present study, BUN levels gradually decreased during the ICU stay in both the SWG and the PWG, and a lower BUN level may be a marker of the cessation of catabolism. We showed that on the first day of weaning the BUN level in the SWG was significantly higher than in the PWG.
Wu et al. found that BUN levels were higher in successfully weaned patients versus those that were unsuccessful (34 versus 50 mg/dL). Their values are a lot higher than presented in this study. In their study the length of ICU stay was longer and their underlying diagnoses were different to COPD [18]. A higher BUN level indicates a continuous catabolic state [5]. In the Wu et al. study, due to the longer respiratory care stay, the patients’ catabolic state was not ceased. Contrary to our results, they also found higher serum creatinine levels in the unsuccessfully weaned patients [18]. Some studies have shown that patients undergoing prolonged mechanical ventilation and with lower BUN and serum creatinine levels were well correlated with successful weaning [9,18]. In the present study, after the acute necessity for intubation was diminished or nearly controlled, we checked serum creatinine and BUN levels at the initiation of the weaning process. The BUN/Creatinine ratio is generally used as a conventional means to determine pre-renal azotemia, and a higher ratio correlates with a failure to wean due to fluid deficiency, after excluding other causes (upper gastrointestinal bleeding and overloaded protein). Scheinhorn et al. found that a BUN/serum creatinine of 35 was the crucial level for unsuccessful weaning [9]. However, we should consider that the ratio could be greater when the serum creatinine is lower or BUN is increased. In our study, COPD patients with a lower serum creatinine on admission to the ICU had a higher BUN/serum creatinine ratio than patients with a normal to high serum creatinine level.
One study showed a delta serum creatinine greater than 0.31 increased mortality in mechanically ventilated patients [19], however, this may reflect co-incidental renal injury. Separating the effect of renal failure from endogenous creatinine generation in an ICU cohort is a very difficult task.
Although mortality was not a primary measurement in the present study, we did observe that mortality was mainly seen in the PWG. Interestingly, APACHE II scores on admission to the ICU were similar in the group with low serum creatinine and the normal to high creatinine groups. Besides a higher APACHE II score, prolonged mechanical ventilation increases mortality in the ICU [20]. We found that the serum creatinine decreased further during the ICU stay in the PWG and their mortality was higher than the SWG. A recent study showed that patients with normal creatinine levels on admission to hospital, and who suffered acute renal failure during their hospital stay, had higher mortality than patients who were admitted to hospital with acute renal failure [21]. However, in the present study we excluded patients with acute renal failure. Another new study concerning fluid overload and acute kidney injury in the ICU [22] defined an acute increase of serum creatinine > 0.5 mg/dL from baseline as acute kidney injury, and they defined volume related weight gain as the difference between initial weight and weight initiation of continuous renal replacement treatment [22]. They assessed statistically significant associations with mortality in multivariate models that included sepsis and Apache II score, and they concluded that fluid overload is an important prognostic factor for survival in critically ill, acute kidney injury patients undergoing renal replacement treatment [22]. In the present study our patients did not have acute kidney injury and we did not measure the weight of patients.
There are some limitations to our study. Due to its retrospective design we did not check inflammatory markers such as IL1, IL6, and TNF (apart from C-reactive protein and urine creatinine levels) [6,13-17]. We also did not perform any measurements of muscle force or activity.
In conclusion, this study was performed in three training centers that followed their guidelines for weaning. We showed that low levels of serum creatinine on the first day of weaning indicated an unfavorable result for COPD patients during the weaning process, contrary to other studies. According to our data, a low serum creatinine on the first day of weaning had a 2.5 times higher risk for prolonged weaning. Although our study was done retrospectively in an homogenous group of COPD patients, the results may be significant in the weaning trials of other patient populations.
Key messages
1. Low serum creatinine and high a BUN/creatinine ratio indicates a hyper-catabolic state and muscle wasting/atrophy.
2. A hyper-catabolic state and muscle weakness/atrophy in COPD patients with low serum creatinine can indicate problems for the weaning process.
Acknowledgements
The manuscript hypothesis and design were improved by the American Thoracic Society Methods in Epidemiologic, Clinical and Operations Research (MECOR) and Turkish Thoracic Society 2008-Turkey. We would like to thank Steve McCurdy, A Sonia Buist, and Phil Hopewell.
Competing Interests
There was no financial research support and no conflict of interest for this study. All authors have no disclosure.
References
- Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, et al. (2007) Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176: 532-555.
- Brochard L (2005) Pressure support is the preferred weaning method. As presented at the 5th International Consensus Conference in Intensive Care Medicine: Weaning from Mechanical Ventilation.
- Tobin MJ, Laghi F, Brochard L (2009) Role of the respiratory muscles in acute respiratory failure of COPD: lessons from weaning failure. J Appl Physiol 107: 962-970.
- Boles JM, Bion J, Connors A, Herridge M, Marsh B, et al. (2007) Weaning from mechanical ventilation. Eur Respir J 29: 1033-1056.
- Mirtallo JM (1990) Assessing the nutritional needs of the critically ill patients. DICP 24: S20-23.
- Oterdoom LH, Gansevoort RT, Schouten JP, de Jong PE, Gans RO, et al. (2009) Urinary creatinine excretion, an indirect measure of muscle mass, is an independent predictor of cardiovascular disease and mortality in the general population. Atherosclerosis 207: 534-540.
- Kitahara Y, Maki T, Torii K (1997) Development of degenerative muscle weakness by chronic administration of beta,beta'-iminodipropionitrile in the drinking water to rats: a model for motorneuropathy. Physiol Behav 62: 443-451.
- Boroujerdi M, Mattocks AM (1983) Metabolism of creatinine in vivo. Clin Chem 29: 1363-1366.
- Scheinhorn DJ, Hassenpflug M, Artinian BM, LaBree L, Catlin JL (1995) Predictors of weaning after 6 weeks of mechanical ventilation. Chest 107: 500-505.
- Consensus Conference IV (1997) Noninvasive positive pressure ventilation. Respir Care 42: 362-449.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13: 818-829.
- Schönhofer B, Euteneuer S, Nava S, Suchi S, Köhler D (2002) Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensive Care Med 28: 908-916.
- Wouters EF, Groenewegen KH, Dentener MA, Vernooy JH (2007) Systemic inflammation in chronic obstructive pulmonary disease: the role of exacerbations. Proc Am Thorac Soc 4: 626-634.
- Broekhuizen R, Wouters EF, Creutzberg EC, Schols AM (2006) Raised CRP levels mark metabolic and functional impairment in advanced COPD. Thorax 61: 17-22.
- Broekhuizen R, Grimble RF, Howell WM, Shale DJ, Creutzberg EC, et al. (2005) Pulmonary cachexia, systemic inflammatory profile, and the interleukin 1beta -511 single nucleotide polymorphism. Am J Clin Nutr 82: 1059-1064.
- Janssen SP, Gayan-Ramirez G, Van den Bergh A, Herijgers P, Maes K, et al. (2005) Interleukin-6 causes myocardial failure and skeletal muscle atrophy in rats. Circulation 111: 996-1005.
- Takabatake N, Nakamura H, Abe S, Inoue S, Hino T, et al. (2000) The relationship between chronic hypoxemia and activation of the tumor necrosis factor-alpha system in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 161: 1179-1184.
- Wu YK, Kao KC, Hsu KH, Hsieh MJ, Tsai YH (2009) Predictors of successful weaning from prolonged mechanical ventilation in Taiwan. Respir Med 103: 1189-1195.
- Nin N, Lombardi R, Frutos-Vivar F, Esteban A, Lorente JA, et al. (2010) Early and small changes in serum creatinine concentrations are associated with mortality in mechanically ventilated patients. Shock 34: 109-116.
- Esteban A, Alía I, Ibañez J, Benito S, Tobin MJ (1994) Modes of mechanical ventilation and weaning. A national survey of Spanish hospitals. The Spanish Lung Failure Collaborative Group. Chest 106: 1188-1193.
- Brar H, Olivier J, Lebrun C, Gabbard W, Fulop T, et al. (2008) Predictors of mortality in a cohort of intensive care unit patients with acute renal failure receiving continuous renal replacement therapy. Am J Med Sci 335: 342-347.
- Fülöp T, Pathak MB, Schmidt DW, Lengvárszky Z, Juncos JP, et al. (2010) Volume-related weight gain and subsequent mortality in acute renal failure patients treated with continuous renal replacement therapy. ASAIO J 56: 333-337.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 15591
- [From(publication date):
April-2013 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10969
- PDF downloads : 4622