The Effect of Effort Test on QT Dispersion in Patients with New Diagnosis of COPD
Received: 05-Nov-2018 / Accepted Date: 23-Nov-2018 / Published Date: 29-Nov-2018
Abstract
Background: Chronic obstructive pulmonary disease (COPD) is associated with increased risk of cardiovascular morbidity and mortality. The aim of this study is to investigate the effect of effort test on corrected QT (QTc) and corrected QT dispersion (QTcd) in patients with newly diagnosed and untreated COPD.
Patients and method: Thirty-three patients who were referred to the chest diseases polyclinic between March- August 2018, who had no previous treatment and had evidence of obstruction in the pulmonary function test were included in the study. As control group, 36 patients who were referred to the cardiology clinic with chest pain, who had no COPD, had an indication for effort test and were negative for effort test, were selected. The study group was initially subjected to pulmonary function test. Patients were then enrolled in the effort test according to the Bruce protocol. QTc and QTcd values were calculated for resting and peak exercise.
Results: The resting QTcd value of the study group was 39.8333 ± 3.6762 ms, value of control group was 38.0244 ± 4.298 ms (p=0.113113, t=1.221961). Peak exercise QTcd values in the study and control groups were 63.356 ± 5.408 ms, 44.475 ± 5.0572 (p<0.00001, t=18.37567), respectively.
Conclusion: There was a statistically significant difference in resting and peak exercise QTcd values in the study group. There was no statistically significant difference between two groups’ resting QTcd values. There was a significant difference between peak exercise QTcd values in the study group and control group.
Keywords: COPD; Corrected QT dispersion; Stress testing
Introduction
Chronic obstructive pulmonary disease (COPD) is associated with increased risk of cardiovascular morbidity and mortality [1-3]. Previous community-based studies have shown that the risk of sudden cardiac death (SCD) in patients with COPD is increased 2-3 times [4]. However, the mechanisms underlying the relationship between COPD and SCD are still unclear, and predictors of malignant cardiac arrhythmias and the predictors of SCD in COPD have not been identified. The change of cardiac repolarization is an important mechanism for the development of malignant arrhythmias and the occurrence of SCD [5-7].
The findings obtained by surface electrocardiography (ECG) represent the distribution of repolarization and electrical homogeneity of the ventricles [8]. Results of previous studies with heart failure [9], patients with long QT syndrome [10] and older individuals [11] have shown that there may be a relationship between malignant arrhythmia and SCD with alteration of cardiac repolarization findings such as QT interval and QT dispersion.
In acute exacerbations of COPD patients and in COPD, QT dispersion and ventricular electrical heterogeneity have been investigated and increased in some studies [12-14]. In addition, COPD patients may have a higher frequency of cardiac arrhythmias and the severity of airway obstruction is thought to be associated with arrhythmia formation [15-17]. It has been shown that QT dispersion can be increased with stress test in hypertensive patients [18]. In addition, it was shown that QT dispersion may be increased by exercise test in healthy individuals [19].
Preliminary evidence from a small case-control study suggests that an increased maximal QT interval is associated with the development of ventricular arrhythmia in patients with COPD [20]. However, the effect of stress test on QT dispersion and ventricular electrical heterogeneity in COPD patients was not investigated. The aim of this study was to investigate the effect of stress test on QT in patients with newly diagnosed and untreated COPD patients and to investigate whether effort is associated with sudden cardiac death and malignant ventricular arrhythmias in COPD patients.
Methodology
Patients
Thirty-tree patients who were admitted to the chest diseases policlinic between March-August 2018, who had not received prior treatment, had obstructive pulmonary function test, were included in the study. The mean age of the study group, consisted of 19 female and 17 male patients, was calculated as 47.88 ± 8.96 (29-71). The control group consisted of 40 patients who presented to the cardiology policlinic with chest pain, had no COPD, had exercise test indication, were found to be negative. The mean age of the control group, consisted of 22 female and 18 male patients, was calculated as 48.64 ± 7.33 (30-72). Patients with a systemic disease such as liver, heart, kidney, systemic hypertension and diabetes mellitus were excluded from the study. There was no statistically significant difference between the two groups' demographic information.
Methods
All participants underwent a standard pulmonary functional test according to the American Thoracic Society [21] to measure forced expiratory volume (FEV1) and forced vital capacity (FVC) within one second. In these patients, FEV1/FVC <70% was considered as a sign of obstruction [22]. Then, patients underwent routine ECG’s [23]. Resting QT values of the patients were measured in routine ECG. The mean of the corrected QT (QTc) interval of the three successive pulses in each lead was taken as the QTc interval of that derivation [24]. Patients whose QTc interval was calculated in at least 9 leads were included in the study. The QTc dispersion (QTcd) was measured by calculating the difference between the longest QTc interval and the shortest QTc interval. All of these evaluations were performed for both the study group and the control group.
Patients were then subjected to stress test according to Bruce protocol [25]. When 88% of the maximal heart rate was reached, the test was terminated. Resting, peak exercise data of the patients were recorded. Thus, resting QTc and QTcd values as well as peak exercise values were calculated.
Statistical analysis
SPSS software for data collection and analysis (Version X; IBM, Armonk, NY) and analysis using t-test. If all tests are p<0.05, the differences are statistically significant.
Results
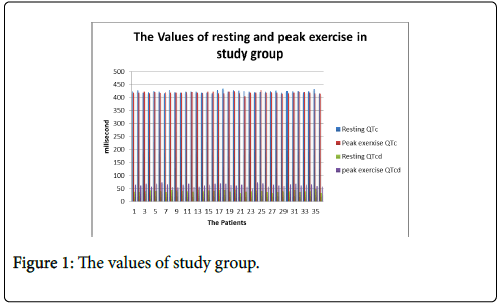
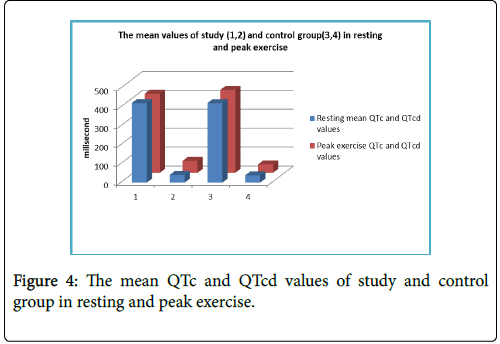
In the study group, the resting QTc value was 421.1389 ± 4.6115 ms, and the peak exercise QTc value was 419.6389 ± 4.0225 ms. There was a statistically significant difference between them (p=0.001229, t=3.264) (Figure 1).
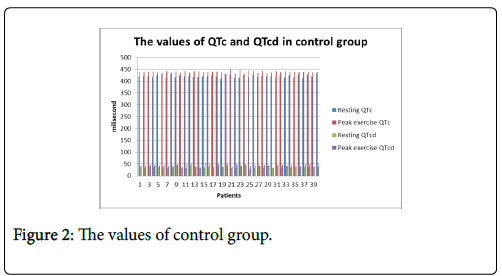
This data showed that QTc duration was shortened by exercise test in the study group. In the control group, the basal QTc value was 420.424 ± 4.9717 ms, in the study group, the resting QTc value was 421.1389 ± 4.6115 ms. No statistically significant difference was found between the control and the study group (p=0.140294, t=1.088214). Resting QTc values were similar in control group and study group. The peak exercise QTc value of the control group was 438.925 ± 4.0582 ms while the study group was 419.6389 ± 4.0225 ms and the difference was statistically significant (p<0.00001, t=21.764) (Figure 2).
It was observed that the QTc value was increased with the stress test in the control group more than the study group. While baseline QTcd was 39.8333 ± 3.6762 ms in the study group, peak exercise QTcd value was 63.356 ± 5.408 ms and the difference between the two values was statistically significant (p<0.00001, t=24.6918).
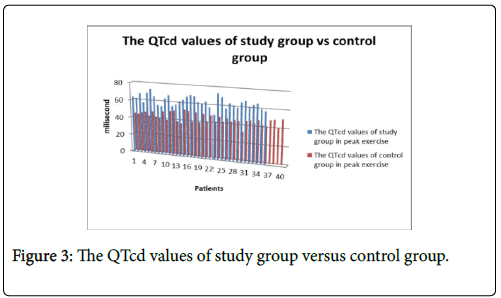
In the study group, it was observed that QTcd duration was significantly increased with exercise test. The baseline and peak exercise QTcd values in the control group were 38.0244 ± 4.298 ms and 44.475 ± 4.0572 ms, respectively. The difference between the two values was statistically significant (p<0.0001, t=6.708204). Although QTcd was significantly prolonged in the control group with the exercise test, QTcd prolongation was in the normal range and the risk of ventricular arrhythmia was low. In the control group, QTcd time was significantly increased with exercise test. The peak exercise QTcd values of the study group and control group were 63.356 ± 5.408 ms and 44.475 ± 4.0572 ms, respectively. The difference between the two groups was statistically significant (p<0.00001, t=18.37567) (Figures 3 and 4).
It was observed that QTcd periods were prolonged with exercise test in both control group and study group. However, the prolongation of QTcd in the control group was within normal limits, while the chances of ventricular arrhythmia were low in control group and in the study group, the risk of ventricular arrhythmias increased abnormally.
Discussion
This study investigated the effect of exercise test according to Bruce protocol on QTc and QTcd in a heterogeneous group of patients who were diagnosed with COPD for the first time and had not received any treatment before. The main finding in this study was that the peak exercise value of the QTcd value of the study group was higher than both the control group and the resting QTcd of the study group and the difference was statistically significant.
A significant difference between the study group and the control group between resting and peak exercise QTcd values measured before and after the effort test was shown to be appropriate for study and control group study purposes. In our prospective study, the increase in QTcd, was statistically significant, a predictor of malignant arrhythmias with exertion in COPD patients diagnosed for the first time, is an important outcome to consider in patients with COPD.
Modified cardiac repolarization may expose these patients to an increased risk for malignant ventricular arrhythmias and SCD. Several pathologies have been reported to increase the risk of SCD, including coronary artery disease, cardiomyopathy, congenital heart disease, and long QT syndrome and electrophysiological abnormalities [26].
A prolonged QT interval and increased QT dispersion are increased markers of malignant cardiac arrhythmias and risk of SCD [9,27]. The prolongation of QTc to >450 ms was defined as a risk factor for malignant ventricular arrhythmias and SCD [28].
QT dispersion (QTd) reflects spatial differences at the time of myocardial recovery. Previous studies have shown that an increase in QTd>60 ms is associated with malignant ventricular arrhythmias [16] and development of SCD [20].
Again in one study, QTcd was found to be as high as our study in the group of patients with hypertensive response compared to healthy people by stress test [29]. Although many studies have previously shown that the hypoxia extends the QTcd to a pronounced extent [30], QTc and QTcd have not been shown to be prolonged by the exercise test.
In another study, salbutamol given as a metered dose in children with acute asthma attack had a statistically non-significant prolongative effect on QT, QTc and QTd and QTcd [31]. In another study, the electrophysiological effects of salbutamol, a beta2-selective agonist, were investigated. Salbutamol had the most effective on atrioventricular node in the heart. Impaired effects of decelerating ventricular conduction were observed and the refractory duration of myocardium was shortened. QT dispersion was found to be prolonged [32].
In our study, a significant difference was found between the study and control groups in values of QTcd. In other words, the chances of ventricular arrhythmia in the study group were higher than the control group. In other words, the risk of ventricular arrhythmia induced by effort was higher in the study group than in the control group.
As a result, in patients with newly diagnosed COPD, it is thought that there may be a greater risk of ventricular arrhythmias with exertion.
Conclusion
Study limitations: In our study, the number of cases is small, healthier data can be made with larger case studies. In addition, longterm studies should be made in order to observe the effect of medical therapy on the prolonged QTcd times and ventricular arrhythmias induced by the exercise test. More comprehensive and long-term follow-up studies should be performed to obtain healthier data.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Anthonisen NR, Connett JE, Enright PL, Manfreda J (2002)Â Hospitalizations and mortality in the Lung Health Study. Am J Respir Crit Care Med.166: 333-339.
- McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA (2007)Â Ascertainment of cause-specificmortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax 62: 411-415.
- Clarenbach CF, Senn O, Sievi NA, Camen G, van Gestel AJ, et al. (2013)Determinants of endothelial function in patients with COPD. Eur Respir J 42: 1194-1204.
- Sin DD, Man SF (2005) Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc.2: 8-11.
- Elming H, Brendorp B, Kober L, Sahebzadah N, Torp-Petersen C (2002)Â QTcinterval in theassessment of cardiac risk. Card Electrophysiol Rev 6: 289-294.
- Straus SM, Kors JA, De Bruin ML, van der Hooft CS, Hofman A, et al. (2006) ProlongedQTcintervaland risk of suddencardiacdeath in a population of olderadults. J Am Coll Cardiol 47: 362-367.
- Bednar MM, Harrigan EP, Anziano RJ, Camm AJ, Ruskin JN (2001) The QT interval. Prog Cardiovasc Dis 43: 1-45.
- Antzelevitch C, Shimizu W, Yan GX, Sicouri S (1998) Cellular basis for QT dispersion. J Electrocardiol 30: 168-175.
- Barr CS, Naas A, Freeman M, Lang CC, Struthers AD (1994) QTÂ dispersion and sudden unexpected death in chronic heart failure. Lancet 343: 327-329.
- Yamaguchi M, Shimizu M, Ino H, Terai H, Uchiyama K, et al. (2003) T wave peak-to-endi ntervaland QT dispersion in acquired long QT syndrome:a new index for arrhythmogenicity. ClinSci(Lond) 105: 671– 676.
- Robbins J, Nelson JC, Rautaharju PM, Gottdiener JS (2003) The association between the length of the QT interval and mortality in the Cardiovascular Health Study. Am J Med115: 689–694.
- Akramova ÉG (2012) Dispersion of QT interval during holter monitoring in patients with chronic obstructive pulmonary disease and bronchial asthma. Klin Med (Mosk) 90: 25-28.
- Lai Y, DeNardo A, Niranjan S, Sriram KB (2017) Increased QT dispersion is associated with reduced overall survival in patients with acute exacerbations of chronic obstructive pulmonary disease. Hosp Pract 45: 253-257.
- Zulli R, Donati P, Nicosia F, De Vecchi M, Tantucci C, et al. (2006)Â Increased QT dispersion: a negative prognostic finding in chronic obstructive pulmonary disease. Intern Emerg Med 1: 279-286.
- Buch P, Friberg J, Scharling H, Lange P, Prescott E (2003) Reduced lung function and risk of atrial fibrillation in the Copenhagen City HeartStudy. Eur Respir J. 21: 1012-1016.
- Kleiger RE, Senior RM (1974) Long term electrocardiographic monitoring of ambulatory patients with chronic airway obstruction. Chest 65: 483–487.
- Sievi NA, Clarenbach CF, Camen G, Rossi VA, van Gestel AJ, et al. (1995)Â High prevalence of altered cardiac repolarization in patients with COPD. Cardiologia. 40: 247-251.
- Ertaş F, Yavuz C, Kaya H, Karahan O, Demirtaş S (2013) The relationship between QT dispersion and exaggerated blood pressure response to exercise stress stesting. Clin Exp Hypertens.35: 470-474.
- Chauhan VS, Krahn AD, Walker BD, Klein GJ, Skanes AC (2002) Sex differences in QTc interval and QT dispersion: Dynamics during exercise and recovery in healthy subjects. Am Heart J. 144: 858-864.
- Yildiz P, Tukek T, Akkaya V, Sozen AB, Yildiz A, et al. (2002) Ventricular arrhythmias in patients with COPD are associated with QT dispersion. Chest. 122: 2055-2061.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. (2005)Â Standardisation of spirometry. EurRespirJ 26: 319-338.
- Global Initiative for Chronic Obstructive Lung Disease (2017) Global Strategy for the Diagnosis, Management and Prevention of COPD.
- Eldridge MJ, Richley D, Ross C, Cox C, Breen C (2014) Clinical Guidelines by Consensus: Recording a standard 12-lead electrocardiogram. An approved methodology by the Society for Cardiological Science and Technology (SCST).
- Bert V, Eline V, Tomas R, Joris V, Christophe G, et al. (2016) Which QTÂ Correction Formulae to Usefor QT Monitoring? J Am Heart Assoc 5:e003264.
- Luong MW, Ignaszewski M, Taylor CM (2016) Stresstesting: AÂ contribution from Dr Robert A. Bruce, father of exercise cardiology. Bc medical journal 58: 70-76.
- Zipes DP, Wellens HJ (1998) Sudden cardiac death. Circulation 98:Â 2334-2351.
- De Bruyne MC, Hoes AW, Kors JA, Hofman A, vanBemmel JH (1999)Â Prolonged QT interval predicts cardiac and all-cause mortality in the elderly. The Rotterdam Study. Eur Heart J. 20: 278-284.
- Viskin S (1999) Long QT syndromes and torsade de pointes. Lancet. 354:Â 1625-1633.
- Barr CS, Naas A, Freeman M, Lang CC, Struthers AD (1994) QTÂ dispersion and sudden unexpected death in chronic heart failure. Lancet. 343: 327-329.
- Tirlapur VG, Mir MA (1982) Nocturnal hypoxemia and associated electrocardiographic changes in patients with chronic obstructive airways disease. N Engl J Med 306: 125-130.
- Polat TB, Saz EU, Nursoy MA (2012) Effects of salbutamol given by metered-dose inhaler on dispersion of ventricular repolarization. Anadolu Kardiyol Derg. 11: 232-236.
- Insulander P, Juhlin-Dannfelt A, Freyschuss U, Vallin H (2004)Â Electrophysiologic effects of salbutamol, a beta2-selective agonist. J Cardiovasc Electrophysiol. 15: 316-322.
Citation: Cosgun A (2018) The Effect of Effort Test on QT Dispersion in Patients with New Diagnosis of COPD. J Card Pulm Rehabil 2:123.
Copyright: © 2018 Cosgun A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 3490
- [From(publication date): 0-2018 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 2595
- PDF downloads: 895