Whom to Blame For Infertility: Semen Analysis of Men from 70 Infertile Couples
Received: 08-Nov-2018 / Accepted Date: 12-Nov-2018 / Published Date: 20-Nov-2018 DOI: 10.4172/2161-1165.1000361
Abstract
Background: Fertility has been one of men admire commendation since the beginning of recorded history and remains a driving need for young couples now days. Infertility is important cause of frustration, despair, and helplessness with debilitating consequences. As per the WHO estimates 60–80 million couples worldwide currently suffer from infertility. In developing countries frequently women are accused of infertility.
Purpose: Aim of this study is to describe semen analysis of men from infertile couples to highlight the male factor as important cause of infertility.
Methods and Material: This is a retrospective observational study. We analysed semen samples from men among infertile couple’s male patients with in 2015 at a hospital in Northern India.
Results: Mean age was 28.9 year. Age range was from 20 year to 45 year of study group. Among 70 infertile couples, primary infertility was more prevalent (59.1%) than secondary infertility (30.1%). Out of 70 patients 50 (71.5%) male were having abnormal semen quality on semen analysis suggesting male factor for infertility. In remaining 20 (28.5%) infertile couples female might have responsible for infertility.
Conclusions: Male infertility is major reason, 71.5% in current study, among infertile couples; therefore, women should not be accused for infertility.
Keywords: Infertility; Semen; Analysis
Introduction
Fertility has been one of men’s desired accreditation since the beginning of recorded history and remains a driving need for young couples now days. Most of people have life plans that include children. When they fail to get children, they find their efforts unsuccessful. Frustration, despair, and helplessness are common with infertility with debilitating consequences [1]. Infertility surveys conducted by the National Center for Health Statistics have shown that in the United States in 1988, 8.4% of the women of 15-44 years of age, or 4.9 million women had an impaired ability to have children; of these, 2.2 million had primary infertility and 2.7 million had secondary infertility [2]. As per the World Health Organization (WHO) estimates 60–80 million couples worldwide currently suffer from infertility [3]. According to WHO, infertility is defined as a disease of reproductive system failure to achieve the clinical pregnancy after 12 months or more of regular unprotected sexual intercourse [4]. There is two type of infertility primary and secondary infertility. In primary infertility, couples never conceived, whereas secondary infertility refers to inability to conceive following a previous pregnancy. Primary infertility is most prevalent worldwide [5]. Sexually transmitted infections (STIs) are common leading preventable cause of infertility worldwide, especially in developing countries [6].
The overall prevalence of primary infertility in our country is between 3.9 and 16.8 percent as estimated by the WHO [7]. Few studies reported that 40% of infertility cases were related to men, 40% of women and 20% of both sexes [8]. According to World Health Organisation (WHO) study reported that male factor contributes to infertility as much as 51.2% [9]. There are several factor associated with male infertility included impotence, testicular atrophy and loss of sexual interest are associated with alcoholism and reduced FSH, LH and testosterone levels have been found as a result of excessive drinking [10].
The infertility rate in various states of our country is different and ranges from 3.7% to 15% [9-11]. Nearly 50% of infertility is related to the reproductive anomalies or disorders of male [12]. The same study also reported that in over 25% of infertility cases, no detectable cause could be traced after routine tests, which leaves the case as unexplained infertility [12]. Research question of this study is: what proportion of infertility in couples can be attributed to men based on abnormal semen analysis? Aim of this study is to describe semen analysis of men from infertile couples to highlight the male factor as important cause of infertility.
Subjects and Methods
The index study was done from January to December 2015 at a hospital in Northern India. This study was a retrospective chart review. Inclusion criteria included men of infertile couple patients who attended hospital with history of infertility and gave semen sample for analysis. Patients who had vasectomy, tubectomy and congenital anomaly of genital tract were excluded. Women were also evaluated for history, radiological and biochemical reports. We collected all the data related to history, systemic disease, family history, and drug history. We reported semen analysis in the form of physical and morphological characters by neubaur chamber. We were charged this chamber with 1:19 ratio of semen and semen diluting fluid. We also examined the direct smear prepared from semen. Sperms morphology was described in Giemsa stain and viability of sperms was described by eosin stain. Semen analysis was done according to WHO guidelines [1]. Percentage of men with abnormal semen analysis was calculated. The study was retrospective not need ethical clearance as per our institute norms.
Results
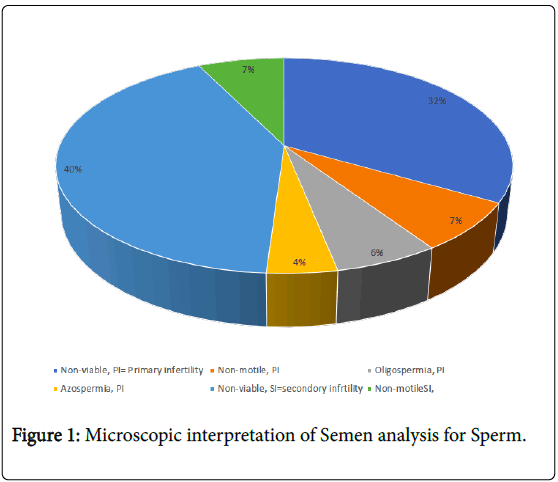
We enrolled 70 male patients from infertile couples with semen analysis in this study. Mean age 28.9 year. Age range was from 20 year to 45 year of study group. Out of 70 patients 50 (71.5%) male were having abnormal semen quality on semen analysis suggesting male factor for infertility. In remaining 20 (28.5%) infertile couples female might have responsible for infertility. The volume of semen we received ranged from 1.5 to 4ml, with gray –white in colour, and average pH was 7.9. The liquefaction time was 20 to 40 minutes. Primary infertility was reported in 30 (60%) patients. Secondary infertility was noted in 20 (40%) cases. The microscopic interpretation of semen analysis for sperm had shown in Figure 1. In primary infertility patients group included 4% patients were having abnormal morphological abnormality in the form of biheaded, big headed, absence of acrosomes, neck abnormality(folded from neck) and tail abnormality(absence of tail). Majority of included males had history of smoking, alcohol consumption and tobacco chewing. Five patients with primary infertility were having history of drug (aryurved medicine) intake. Secondary infertility was noted in factory workers and malnourished patients. Thus, these factors were directly and indirectly associated with infertility.
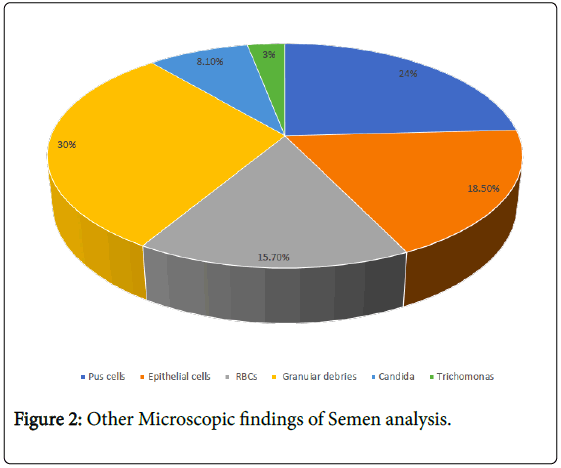
Other morphological findings of semen analysis had shown in Figure 2. Patients those were infected by trichomonas and candidacies had low sperm counts, high non- motile sperm, more granular debris, increased pus cells and increased RBCs. We were noted trichomonas more severely affected semen quality than candidiasis. Out 70 women, 60 women were had no any abnormalities in their history, radiology and biochemical reports. We did not find data of 10 women.
Discussion
In present study we had shown that male infertility is a major factor in infertility and semen analysis plays an important role in diagnosis of male infertility. Sadock et al. reported that 40% of infertility cases were related to men, 40% of women and 20% of both sexes; male infertility accounted for 60 % overall [8]. In our study male infertility was present in 70%; we don’t have data on women infertility.
Zargar et al. reported that primary infertility is common and distressing problem in developing countries, which is corroborating with our findings [13]. Zargar et al. reported semen abnormalities (22.4%), anovulation (17.2%), ovarian failure (8.8%), hyperprolactinemia (8.4%), and tubal disease (7.2%) as common causes of infertility. But in our study, we found semen abnormality in 71.5% of males among infertile couples. Geoffroy-Siraudin et al. demonstrated declining trends in sperm concentration (1.5%/year), total sperm count (1.6%/year), total motility (0.4%/year), rapid motility (5.5%/year), and normal morphology (2.2%/year) [14]. According to a study conducted in developing countries, the decline in sperm count was 30.31% whereas, sperm motility and morphology was reduced by 22.92% and 51.25%, respectively [15]. These findings were much higher than our findings and indicated qualitative impairment of spermatogenesis and perhaps of the sertoli cells [16]. One study from a developing country reported that over 12–18 million couples are diagnosed with infertility every year, with normal sperm counts [17]. Similarly, in our study most of patients had normal sperm counts but they were infertile. The exact reason for the decline in semen quality is not clear, but many studies were suggested it may be due to environmental, nutritional, socioeconomic or other unknown causes [18].
Few studies had reported that sperm motility decreases with advancing age [19]. Studies indicate a decline in normal sperm morphology of 0.2–0.9% per year of age [19]. Kalokhe et al. reported that infertility is important factors for domestic violence against women [20]. Few studies reported that male infertility impacts a substantial proportion of men and has serious implication for a man’s quality of life [21,22]. Present study has not any case of onco-infertility.
Whereas we found major part of infertility was contributed by men. Therefore, its messages to the society that frequently women are accused for infertility, but in reality, men are responsible for large number of infertilities.
Conclusion
In 70 infertile couples, male were responsible for infertility in 71.5%. The male infertility was mostly due to reduced semen quality in the form of non-viable sperms, and non-motile sperms. The index study is addressing an important issue of male factor of infertility. Unfortunately, it is not a norm in a clinical practice to look for a male factor of infertility although it is easy to diagnose with simple semen analysis. Accusing women for infertility in the society should be stopped.
References
- Jones HW Jr, Toner JP (1993) The infertile couple. N Engl J Med 329: 1710-1715.
- Mosher WD, Pratt WF (1990) Fecundity and infertility in the United States, 1965-88. Advance data from vital health statistics. No. 192. Hyattsville, MD: Public Health Service.
- Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, et al. (2009) International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril 92: 1520–1524.
- Inhorn MC (2003) Global infertility and the globalization of new reproductive technologies: illustrations from Egypt. Soc Sci Med 56: 1837-1851.
- Ombelet W, Cooke I, Dyer S, Serour G, Devroey P (2008) Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update 14: 605-621.
- World Health Organization (2004) Infecundity, infertility, and childlessness in developing countries. DHS Comparative Reports No 9. Calverton, Maryland, USA: ORC Macro and the World Health Organization.
- Sadock BJ, Sadock VA (2003) 9th ed. Philadelphia: Lippincott Williams and Wilkins; 2003. Kaplans and Sadocks Symptoms of Psychiatry Behavioral Sciences. Indian J Psychiatry 51; 331.
- Velu A, Prasad G (2017) Epidemiologic aspects of male infertility. Int J Reprod Contracept Obstet Gynecol 6: 3362-3365.
-  Inhorn MC, Patrizio P (2015) Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update 21: 411–426.
- Talwar PP, Go OP, Murali IN (1986) Prevalence of infertility in different population groups in India and its determinants. Statistics and Demography. New Delhi: National Institute of Health and Family Welfare and Indian Council of Medical Research.
- Unisa S (1999) Childlessness in Andhra Pradesh, India: Treatment-seeking and consequences. Reprod Health Matters 7: 54-64.
- Zargar AH, Wani AI, Masoodi SR, Laway BA, Salahuddin M (1997) Epidemiologic and etiologic aspects of primary infertility in the Kashmir region of India. Fertil Steril 68: 637-643.
- Kumar TCA (2004) Fertility and in-vitro fertilization in India. Curr Sci 86: 254-256.
- Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, et al. (2010) World Health Organization reference values for human semen characteristics. Hum Reprod Update 16: 231-245.
- Geoffroy-Siraudin C, Loundou AD, Romain F, Achard V, Courbière B, et al. (2012) Decline of semen quality among 10 932 males consulting for couple infertility over a 20-year period in Marseille, France. Asian J Androl 14: 584-590.
- Adiga SK, Jayaraman V, Kalthur G, Upadhya D, Kumar P (2008) Declining semen quality among South Indian infertile men: A retrospective study. J Hum Reprod Sci 1: 15-18.
- Sharpe RM (1993) Declining sperm counts in men – Is there an endocrine cause? J Endocrinol 136: 357-360.
- Express News Service (2014) Male and Female Infertility Just Keeps on 'Rising'. The Indian Express.
- Jørgensen N, Andersen AG, Eustache F, Irvine DS, Suominen J, et al. (2001) Regional differences in semen quality in Europe. Hum Reprod 16: 1012–1019.
- Harris ID, Fronczak C, Roth L, Meacham RB (2011) Fertility and the aging male. Rev Urol 13: e184-190.
- Kalokhe AS, Potdar RR, Dunkle KL, Paranjape A, del Rio C, et al. (2015) How Well Does the World Health Organization Definition of Domestic Violence Work for India? PLoS One 10: e0120909.
- Walsh TJ (2011) Male Reproductive Health and Prostate Cancer Risk. Curr Opin Urol 21: 506-513.
Citation: Khairwa A, Kumar D (2018) Whom to Blame For Infertility: Semen Analysis of Men from 70 Infertile Couples. Epidemiology (Sunnyvale) 8: 361 DOI: 10.4172/2161-1165.1000361
Copyright: © 2018 Khairwa A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5148
- [From(publication date): 0-2018 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 4236
- PDF downloads: 912