Research Article
Weight Loss Following Left Gastric Artery Embolization in a Human Population without Malignancy: A Retrospective Review
| Kevin Anton*, Tariq Rahman, Ashok B. Bhanushali, Luis L. Nadal, Gregory Pierce and Aalpen A. Patel | |
| Division of Vascular and Interventional Radiology, Department of Radiology, Geisinger Medical Center, Danville, USA | |
| Corresponding Author : | Kevin Anton Division of Vascular and Interventional Radiology Department of Radiology, Geisinger Medical Center Danville, PA 17822, USA Tel: 570-271-6203 Fax: 570-271-5976 E-mail: kfanton@geisinger.edu |
| Received November 22, 2015; Accepted November 30, 2015; Published December 03, 2015 | |
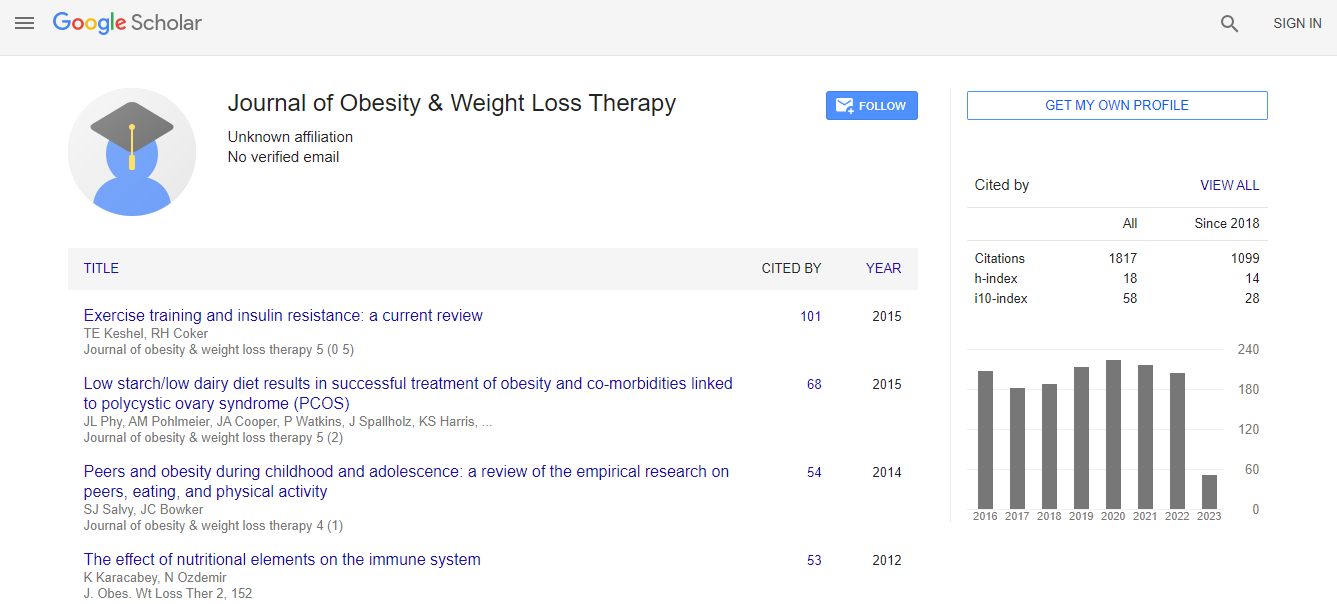
| Citation: Anton K, Rahman T , Bhanushali AB, Nadal LL, Pierce G, et al. (2015) Weight Loss Following Left Gastric Artery Embolization in a Human Population without Malignancy: A Retrospective Review. J Obes Weight Loss Ther 5:285. doi:10.4172/2165-7904.1000285 |
|
| Copyright:© 2015 Anton K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. | |
| Related article at Pubmed, Scholar Google | |
Abstract
Objective: Recent evidence suggests embolization of the left gastric artery, which provides the predominant arterial supply to the gastric fundus, may affect energy homeostasis through alterations in ghrelin production. The purpose of this study is to evaluate post-procedural weight loss following left gastric artery embolization (performed for reasons other than for weight loss) in patients without malignancy. Materials and Methods: A retrospective review of patients who underwent arterial embolization for acute upper gastrointestinal hemorrhage between January 2002 and January 2014 was conducted. A study group of 10 patients who underwent left gastric artery embolization and control group of 22 patients who underwent embolization of a different mesenteric or visceral arterial branch for non-tumoral acute gastrointestinal bleeding were collected. Their electronic medical records were reviewed and data points for height, weight, and body mass index were collected at 1-, 4-, 8-, and 12-month post-procedural time points. Exclusion criteria included age less than 18 years and documented history of malignancy. Results: The left gastric artery embolization group had a significantly greater reduction in body mass index compared with the control group at 1 month (-9.8% vs. -4.0%, p=0.042) and 4 months (-11.7% vs. +0.1%, p=0.033). No significant change was demonstrated at 8 months (-8.6% vs. -1.7%, p=0.32) and 1 year (-5% vs. +2.6%, p=0.42) compared with controls. Conclusion: Left gastric artery embolization provides early post-procedural weight loss that may persist for at least 1 year. Further studies will better elucidate the role of gastric artery embolization in the management of bariatric patients.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi