Research Article Open Access
Short- and Long-Term Effects of Workshop-Style Educational Program on Long-Term Care Leaders ’ Attitudes toward Facility End-of-Life Care
Yoshihisa Hirakawa1*, Takaya Kimata2 and Kazumasa Uemura1
1Center for Postgraduate Clinical Training and Career Development, Nagoya University Hospital, 65 Tsuruma-cho, Showa-ku, Nagoya, Aichi, 466-8560, Japan
2Aoi Home Clinic, 1-15 Hinokuchi-cho, Nishi-ku, Nagoya, Aichi, 451-0034, Japan
- *Corresponding Author:
- Yoshihisa Hirakawa
Center for Postgraduate Clinical Training and Career Development
Nagoya University Hospital, 65 Tsuruma-cho
Showa-ku, Nagoya, Aichi, 466-8560, Japan
Tel: +81-52-744-2644
Fax: +81-52-744-2999
E-mail: y.hirakawa@med.nagoya-u.ac.jp
Received date: August 22, 2013; Accepted date: November 06, 2013; Published date: November 08, 2013
Citation: Hirakawa Y, Kimata T, Uemura K (2013) Short- and Long-Term Effects of Workshop-Style Educational Program on Long-Term Care Leaders’ Attitudes toward Facility End-of-Life Care. J Community Med Health Educ 3:234. doi:10.4172/2161-0711.1000234
Copyright: © 2013 Hirakawa Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Although the proper training of caring staff is required, very few studies have actually focused on the effects of caring staff educational programs on end-of-life care at long-term care facilities. The aim of the present study was to test a pilot caring staff education program emphasizing quality end-of-life care for elderly residents at long-term care facilities. Method: The workshop program was designed by an expert panel made up of long-term care educational leaders from 8 selected long-term care facilities. The topics of the program were: (1) definition of end of life of the elderly, (2) signs and symptoms of imminent death, (3) advanced care planning, (4) issues related to tube feeding, (5) communication with family members of end-of-life residents, (6) communication with bed-ridden elderly, and (7) staff education concerning key elements in the provision of end-of-life care for elderly residents. Study questionnaires were administered to participants both before and after the educational intervention. The questionnaires included two major sets of questions: the Frommelt Attitude toward Care of the Dying scale, Form B, Japanese version and the Death Attitude Inventory. Six months after the intervention, the same questionnaire was mailed to the participants. Result: A total of two hundred and forty seven care leaders participated in the program. Two hundred and forty care leaders completed pre- and post-questionnaires. Out of these, 226 completed a follow-up questionnaire six months after the program. Our six month follow-up data confirms improvements in the participants’ attitudes toward end-of-life care provision at long-term care facilities. Our data also indicates an improved outlook on caring for the dying patient and the maintenance of a positive perception of patient- and family-centered care. Conclusion: Our workshop-style educational program had positive short- and long-term effects on long-term care leaders’ attitudes toward facility end-of-life care.
Keywords
Palliative care; Workshop; Education; Attitudes toward death; Caring staff; Older people
Introductionwww.omicsonline.org/scholarly/end-of-life-care-journals-articles-ppts-list.php
In 2001, the Japan Geriatric Society released its Position Statement regarding palliative care for the elderly, formulating the following observation on end-of-life care for the elderly: the majority of health care professionals receive insufficient specialized training in the care of terminally-ill patients [1]. There is a particular need for comprehensive and practical instruction in the care of dying patients, including symptom management and communication skills [2,3]. Over the past decade, there has been a growing national awareness in the deficiencies in end-of-life care education for health care professionals. A national study on undergraduate end-of-life care education programs for medical and nursing schools conducted in 2005 revealed that most medical and nursing schools offered palliative care education programs, but that the mean number of teaching hours was too low (7.6 hours in medical schools vs 35.5 hours in nursing schools) to allow for the acquisition of proper skills. In addition, most of such end-of-life care education programs included only a course on end-of-life care for cancer patients, indicating a serious education deficiency in the area of elderly care at end-of-life [2].
One of the most important goals of end-of-life education is to ensure the proper training of caring staff [4-7]. As a result of new policies promoting home care, as well as recent changes in preferences of elderly patients and their families, greater numbers of frail elderly are now opting to spend the last years of their life at home or at a long-term care facility rather than at a hospital [7,8]. Therefore, staff involvement in supplying end-of-life care has increased [8-10]. A 2006 survey on nursing and caring staff education revealed that 97.8% of staff recognized a need for end-of-life care education [11].
The deficiencies in end-of-life care education are seriously affecting the performance of caring staff. As well, the lack of medical professionals who receive quality end-of-life care education is having a negative impact on the quality and quantity of end-of-life care education for caring staff because medical professionals act as role models for caring staff. A large 2003 study on end-of-life care education at long-term care facilities in Japan revealed that only 47.9% of long-term care facilities provided staff education on end-of-life care; this was found to have a negative influence on the facilities’ policies on end-of-life care provision [6]. Thus, improving the quality and quantity of caring staff end-of-life care education at long-term care facilities has become an urgent priority in Japan.
End-of-life care educational programs and guidelines for caring staff have been developed in several countries. In the United States, Henderson et al. prepared an end-of-life care training manual for long-term care staff [9]. In Canada, the National Advisory Committee developed the “Guide to end-of-life care for seniors”, a useful and informative document for caring staff working at long-term care facilities and community care settings [12]. Again in Canada, Kortes- Miller et al. designed a 15-hour inter-professional curriculum tailored to meet the needs of caring staff [13]. Arcand et al. performed a pilot study to assess the impact, in terms of family satisfaction with end-oflife care, of a nursing home pilot educational program for nursing staff and physicians on comfort care and advanced dementia, and reported that the program improved family satisfaction with end-of-life care [4]. Also, Parks et al. conducted a pilot end-of-life care education program which ultimately contributed to improve caring staff’s attitude toward end-of-life care [5].
However, very few studies have actually focused on the effects of caring staff educational programs on end-of-life care at longterm care facilities in Japan and other countries. Furthermore, introducing end-of-life care education programs from other countries in Japan represents quite a challenge. For example, there are several difficulties associated with the use of advance directives in Japan [14]. Particularly, the will of elderly patients might change after considering the feelings of others [15], or the patient might be reluctant to make a decision [1,8]. Moreover, the Japan Association of Geriatric Care Services Facilities [16] and Tsuruwaka and Semba [17] reported that discussing end-of-life care or life-sustaining treatment options upon admission is psychologically difficult for caring staff; discussions on advance care planning with newly admitted residents are nevertheless strongly recommended. It is now important to devote studies to and accumulate data on end-of-life care education for caring staff in Japan. It is especially crucial for non-western countries such as Japan, a superaging society, to develop educational programs for end-of-life care for the elderly [8,18].
The aim of the present study was to test a pilot caring staff education program emphasizing quality end-of-life care for elderly residents at long-term care facilities. This nationwide pilot study assessed the attitudes and knowledge of long-term care leaders about issues related to end-of-life care for elderly residents before and after this educational intervention. The study also assessed whether the observed changes were maintained over a 6-month follow-up period.
Methods
Participant recruitment
To provide equal access to this educational intervention throughout Japan, we mailed an invitation letter to all long-term care facilities in the following five prefectures: Akita (Tohoku area) 369 facilities, Ibaraki (Kanto area) 611 facilities, Aichi (Tokai area) 897 facilities, Hyogo (Kansai area) 893 facilities, Fukuoka (Kyushu area) 1399 facilities. Two long-term care leaders per facility were selected to take part in the study, to ensure participant diversity. Further, we refrained from recruiting inexperienced long-term care staff because we felt that they would not be sufficiently knowledgeable to discuss end-of-life care.
Educational intervention
The educational program was designed by an expert panel made up of long-term care educational leaders from 8 selected long-term care facilities in and around Nagoya City. The eight-member panel included: two geriatric physicians, a nurse practitioner, a long-term care facility administrator, a social worker, and three caring staff. The educational program was developed as a 7-hour workshop-style course by the panel and focused on important end-of-life care themes identified in previous trials, studies, literature, and the members’ educational experience [3,5,6,9,18-20].
The workshop programs were held separately in the five prefectures in 2012. Workshop participants were divided into groups of 7 to 8 people. The topics of the workshop program were: (1) definition of end of life of the elderly (60 min), (2) signs and symptoms of imminent death (50 min), (3) advanced care planning (60 min), (4) issues related to tube feeding (60 min), (5) communication with family members of end-of-life residents (80 min), (6) communication with bed-ridden elderly (50 min), and (7) staff education concerning key elements in the provision of end-of-life care for elderly residents (60 min). Each session was facilitated by a panel composed of a physician (the first author) and a nursing practitioner. Prior to each session, the participants were given a 10-minute micro lecture, after which they took part in group work and presented their discussion results. During the session “definition of end of life of the elderly”, the participants discussed and defined the onset of the end-of-life stage for the elderly. During the session “signs and symptoms of imminent death”, the participants discussed and listed the frequently observed signs and symptoms of imminent death among end-of-life elderly. During the session “advance care planning”, the participants discussed a hypothetical case where a caring staff provides emergency cardiopulmonary resuscitation to a resident with a do-not-resuscitate order. During the session “issues related to tube feeding”, the participants took part in a debate on the pros and cons of tube feeding for end-of-life care elderly residents. During the session “communication with family members of end-of-life elderly patients”, we used role-play as a way to get the participants to share their experiences of dealing with families of endof- life residents. During the session “communication with bed-ridden elderly”, the participants watched a 2-minute trigger video script where a bed-ridden elderly was being treated roughly, and discussed proper attitudes toward elderly residents. During the session “staff education concerning key elements in the provision of end-of-life care for elderly residents”, the participants discussed the items they felt should be prioritized in the provision of end-of-life care for elderly residents and designed micro teaching program for inexperienced caring staff based on the discussion results.
Assessment
Study questionnaires were administered to participants both before and after the educational intervention. The questionnaires included a study question as well as two major sets of questions: the Frommelt Attitude toward Care of the Dying scale, Form B, Japanese version (FATCOD-Form B-J) [21,22] and the Death Attitude Inventory (DAI) created by Hirai et al. [23]. The expert panel created a study question on positive attitudes toward end-of-life care provision at the participants’ long-term care facilities. The question was graded on a 5-point Likert scale where a score of 1 signifies that the respondent is “not at all in agreement” and a score of 5 signifies that the respondent is “in complete agreement”. The FATCOD Scale-Form B is a 30-item scale designed to measure the participants’ attitudes toward providing care to dying patients and their families. It includes two subscales: positive attitude toward caring for the dying patient and perception of patient- and family-centered care. The worded items of the FATCOD Scale-Form B are rated on a 5-point Likert scale. Possible scores range from 30 to 150, with higher scores indicating more positive attitudes. The FATCODForm B-J Scale, the Japanese version of the FATCOD Scale-Form B, has a high reliability and validity rating. The DAI is designed to analyze attitudes toward death in context of Japanese cultural characteristics, and is composed of seven factors: Afterlife belief, Death anxiety, Death relief, Death avoidance, Life purpose, Death concern, and Supernatural belief. The worded items of the DAI are rated on a 5-point Likert scale where a score of 1 signifies that the respondent is “not in agreement” and a score of 5 signifies that the respondent is “in agreement”; higher scores therefore indicate a stronger tendency to agree.
A pretest was performed just before starting the workshop program, and a posttest was carried out right after the program. The posttest featured the same questions as the pretest questionnaire. Six months after the intervention, the same questionnaire was mailed to the participants. The participants did not receive any take-home educational materials on end-of-life care but they were given the products they had created during the workshop.
Analysis
The data was statistically analyzed comparing pre- and post-test scores, as well as post and follow-up test scores. We analyzed the data using SPSS and compared inter group changes over time using the paired-T test. P<0.05 scores were considered to be significant.
Results
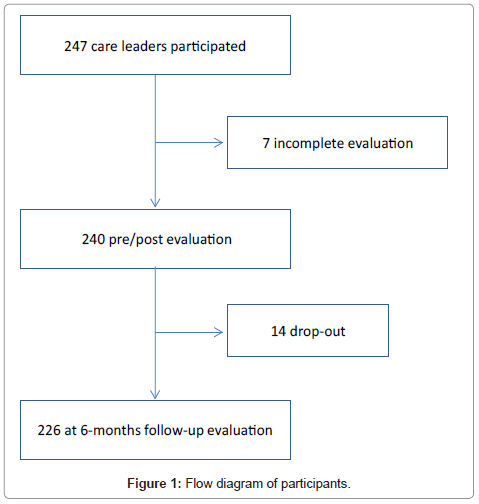
A total of two hundred and forty seven care leaders participated in the workshop program. Two hundred and forty care leaders completed pre-and post- questionnaires (97.2%). Out of these, 226 completed a follow-up questionnaire six months after the program (94.2%).
Immediate post-intervention
As shown in Table 1, the participants scored a pre-intervention mean of 3.97 and a post-intervention mean of 4.05 in the study question on positive attitude toward end-of-life care provision at each of the participants’ long-term care facility, signaling a significant change between pre- and post-intervention (P=0.042).
| pre | post | p-value | ||
|---|---|---|---|---|
| Positive attitude towards end-of-life care provision at facilities | 3.97 | 4.05 | 0.042 | |
| FATCOD-Form B-J* | Positive attitude toward caring for the dying patient | 3.85 | 3.94 | 0.000 |
| Perception of patient-and-family-centered care | 3.81 | 3.89 | 0.004 | |
| DAI** | After life belief | 3.37 | 3.33 | 0.261 |
| Death anxiety | 3.19 | 2.83 | 0.000 | |
| Death relief | 2.58 | 2.64 | 0.154 | |
| Death avoidance | 2.14 | 2.16 | 0.531 | |
| Life purpose | 2.95 | 3.11 | 0.000 | |
| Death concern | 2.84 | 2.88 | 0.278 | |
| Super natural belief | 3.19 | 3.17 | 0.597 |
**Death Attitude Inventory
Table 1: Short-term effect of workshop-style educational program on long-term care leaders’ attitudes toward facility end-of-life care (n=240).
As for the FATCOD-Form B-J Scale, there was a significant change in positive attitude toward both caring for the dying patient (P=0.000) and perception of patient- and family-centered care (P=0.004).
As for the DAI, there was a significant decrease in tendency to agree about Death anxiety (P=0.000), and a significant increase in tendency to agree about Life purpose (P=0.000).
Six-month follow-up
The original cohort of 240 participants was studied six months after the completion of the educational intervention. Two hundred and twenty six of the original 240 participants completed the follow-up questionnaire. Ten of the original participants were lost to follow-up because the staff no longer worked at the facility, and 4 participants were lost due to unknown reasons (Figure 1).
As shown in Table 2, with respect to the study question on positive attitude toward end-of-life care provision at each of the participants’ long-term care facility, no significant change between post and followup was recorded (P=0.770).
| pre | post | p-value | ||
|---|---|---|---|---|
| Positive attitude towards end-of-life care provision at facilities | 4.08 | 4.07 | 0.770 | |
| FATCOD-Form B-J* | Positive attitude toward caring for the dying patient | 3.93 | 3.89 | 0.081 |
| Perception of patient-and-family-centered care | 3.87 | 3.89 | 0.526 | |
| DAI** | After life belief | 3.30 | 3.32 | 0.700 |
| Death anxiety | 2.83 | 3.00 | 0.001 | |
| Death relief | 2.63 | 2.59 | 0.540 | |
| Death avoidance | 2.16 | 2.09 | 0.168 | |
| Life purpose | 3.10 | 3.08 | 0.486 | |
| Death concern | 2.86 | 2.84 | 0.688 | |
| Super natural belief | 3.14 | 3.25 | 0.038 |
**Death Attitude Inventory
Table 2: Long-term effect of workshop-style educational program on long-term care leaders’ attitudes toward facility end-of-life care (n=226).
As for the FATCOD-Form B-J Scale, the positive attitude toward caring for the dying patient (P=0.081) and the perception of patientand family-centered care (P=0.526) was maintained by the participants six months following the program.
As for the DAI, there was a significant increase in tendency to agree about Death anxiety (P=0.001) and Supernatural belief (P=0.038). There was no significant change in tendency to agree about Life purpose (P=0.486).
Discussion
This nationwide pilot project represents a preliminary step toward developing a standardized end-of-life care educational program for long-term care leaders looking after end-of-life elderly residents. The large number of participants who took part in this pilot trial highlights the unmet educational needs of long-term care leaders engaged in endof- life care. Presumably, the lack of exchange on views and information on end-of-life care for elderly among long-term care facilities leads to misconceptions [20] and contributes to a certain feeling of guilt among care leaders. Our program aims at promoting greater exchange among the country’s various long-term care facilities and encouraging the improvement of skills and attitudes of end-of-life care leaders. This community-based end-of-life care education program may ultimately help care leaders’ modify their views about their role in dealing with the death of elderly end-of-life residents, which they often regard as being the responsibility of medical professionals. The program may also help improve the quality of the end-of-life period of long-term care facility residents.
Our six month follow-up data confirms improvements in longterm care leaders’ attitudes toward end-of-life care provision at all of the participants’ long-term care facilities. Our data also indicates an improved outlook on caring for the dying patient and the maintenance of a positive perception of patient- and family-centered care. Matsui and Braun previously examined nurses’ and care workers’ attitudes toward caring for dying older people, and revealed that better attitudes toward caring for them were positively associated with end-of-life care seminar attendance [7]. Because care leaders become involved in training inexperience staff, improving their attitude about end-of-life issues is an important way to enhance the quality of end-of-life care in the community. Also, it is important for long-term care facility administrators to demonstrate that short-time educational programs such as ours can produce positive attitude changes among long-term care leaders for at least up to six months. Parks et al. determined if shorttime five educational seminars can improve knowledge and attitude among long-term care staff on end-of-life care issues in long-term care facility, and demonstrated that such program can improve end-of-life knowledge and attitudes among them [5]. Our results may confirm the results of Parks et al.’s study. Thus, we believe that the educational seminars should be short-time in order to increase participation. However, the success of this work-shop style program lies in great part on the skills of competent facilitators; therefore, in order to expand our program to other areas, we need to train facilitators and evaluate the effects of the program.
The results of our study reveal a short-term relief of death anxiety; however, this effect was not maintained for a long time. Caring staff’s death anxiety may have an impact on the quality of end-of-life care for elderly residents [7]. In addition, death anxiety may increase the psychological distress of long-term care leaders. Our results suggest that we need to develop an educational program focusing on attitudes toward death designed for facilities or individuals. Our six month follow-up data indicates that the initial improvement in long-term care leaders’ attitudes toward life purpose was maintained following the workshop program. This outcome may be closely related to the improved attitudes toward end-of-life issues and provision among long-term care leaders. In addition, our results show a significant increase in tendency to agree with supernatural beliefs, although no change was observed between pre- and post-intervention. However, we currently lack sufficient qualitative data to interpret our results of DAI. Additional qualitative studies on the effects of the present educational program on participants’ attitudes toward death therefore need to be carried out.
Our program has several limitations. Because this educational program has not been authorized or standardized, the details of the program should be verified. For example, it is not clear what effect each individual session had on the participants, although we know that the overall program had a positive impact on their attitude towards end-oflife care. Also, since we did not develop a complete facilitator’s manual, the effects of the program may have been influenced by the ability of the facilitator to guide the discussions. Furthermore, it is possible that the experience of discussing end-of-life care with other participants from other facilities may have triggered a peer support effect, and it is therefore unclear whether the program itself had an educational impact or not. We need to carry out additional studies to confirm our results.
Acknowledgement
This study was supported by the Ministry of education, culture, sports, science and technology-Japan. We extend all participants from long-term care facilities who took part in our study. We also thank the following research assistants: Ms. Noriko Sano and Ms. Junko Shinoda.
References
- Japan Geriatric Society (2001) Announcement from The Japan Geriatrics Society Ethics Committee: The Terminal Care of the Elderly- position statement from the Japan Geriatrics Society. 01.08
- Hirakawa Y, Masuda Y, Uemura K, Kuzuya M, Noguchi M, et al. (2005) [National survey on the current status of programs to teach end-of-life care to undergraduates of medical and nursing schools in Japan]. Nihon Ronen Igakkai Zasshi 42: 540-545.
- Meekin SA, Klein JE, Fleischman AR, Fins JJ (2000) Development of a palliative education assessment tool for medical student education. Acad Med 75: 986-992.
- Arcand M, Monette J, Monette M, Sourial N, Fournier L, et al. (2009) Educating nursing home staff about the progression of dementia and the comfort care option: impact on family satisfaction with end-of-life care. J Am Med Dir Assoc 10: 50-55.
- Parks SM, Haines C, Foreman D, McKinstry E, Maxwell TL (2005) Evaluation of an educational program for long-term care nursing assistants. J Am Med Dir Assoc 6: 61-65.
- Hirakawa Y, Masuda Y, Kuzuya M, Iguchi A, Uemura K (2007) Non-medical palliative care and education to improve end-of-life care at geriatric health services facilities: a nationwide questionnaire survey of chief nurses. Geriatrics and Gerontology International 7: 266-270.
- Matsui M, Braun K (2010) Nurses' and care workers' attitudes toward death and caring for dying older adults in Japan. Int J Palliat Nurs 16: 593-598.
- Hirakawa Y (2012) Palliative Care for the Elderly: A Japanese Perspective, InTech 978-953-307-986-8.
- Henderson ML, Hanson L, Reynolds K (2000) Improving nursing home care of the dying: a training manual for nursing home staff. NY: Springer Publishing Company.
- Zimmerman S, Sloane PD, Hanson L, Mitchell CM, Shy A (2003) Staff perceptions of end-of-life care in long-term care. J Am Med Dir Assoc 4: 23-26.
- Hirakawa Y, Kuzuya M, Uemura K (2009) Opinion survey of nursing or caring staff at long-term care facilities about end-of-life care provision and staff education. Arch Gerontol Geriatr 49: 43-48.
- National Advisory Committee (2000) A Guide to End-of-Life Care for Seniors. University of Toronto and University of Ottawa
- Kortes-Miller K, Habjan S, Kelley ML, Fortier M (2007) Development of a palliative care education program in rural long-term care facilities. J Palliat Care 23: 154-162.
- Masuda Y, Fetters MD, Hattori A, Mogi N, Naito M, et al. (2003) Physicians's reports on the impact of living wills at the end of life in Japan. J Med Ethics 29: 248-252.
- Hattori A, Masuda Y, Fetters MD, Uemura K, Mogi N, et al. (2005) A qualitative exploration of elderly patients’ preferences for end-of-life care. Japan Medical Association Journal 48: 388-397.
- Japan Association of Geriatric Care Services Facilities (2007) Report of the study on development of guidelines on end-of-life care at geriatric care services facilities.
- Tsuruwaka M, Semba Y (2010) Study on confirmation of intention concerning end-of-life care upon moving into welfare facilities for elderly requiring care. Journal of the Japan Association for Bioethics 20: 158-164.
- Hirakawa Y, Kuzuya M, Uemura K (2009) Topics of medical education concerning end-of-life care for the elderly. Medical Education Japan 40: 61-64.
- Hirakawa Y, Uemura K (2013) Community-based education concerning palliative care for the elderly in Japan. Caregivers: Challenges, Practices and Cultural influences, Adrianna Thurgood and Kasha Schuldt Nova Science Publishers, NY 207-216.
- Hockley J, Froggatt K (2006) The development of palliative care knowledge in care homes for older people: the place of action research. Palliat Med 20: 835-843.
- Nakai Y, Miyashita M, Sasahara T, Koyama Y, Shimizu Y (2006) Factor structure and reliability of the Japanese version of the Frommelt attitudes towards care of the dying scale (FATCOD-B-J). Jpn J Cancer Nurs 11: 723-729.
- Frommelt KH (1991) The effects of death education on nurses' attitudes toward caring for terminally ill persons and their families. Am J Hosp Palliat Care 8: 37-43.
- Hirai K, Sakaguchi Y, Abe K, Morikawa Y, Kashiwagi T (2000) The study of death attitude: construction and validation of the Death Attitude Inventory. Jpn J Clin Res Death Dying 23: 71-76.
--
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 15631
- [From(publication date):
November-2013 - Dec 10, 2025] - Breakdown by view type
- HTML page views : 10886
- PDF downloads : 4745