Research Article Open Access
Are Variations of Paranasal Sinuses and Infundibular Trace Length Responsible for Development of Maxillary Sinusitis?
Paşaoğlu L*, Toprak U, Üstüner E, Temel E, Özer H and Mamedova DAnkara Numune Training and Research Hospital, Altındağ, Ankara, Turkey
- *Corresponding Author:
- Lale Paşaoğlu
Radiologist, Ankara Numune Training and Research Hospital
Talatpaşa Blv No: 44, Altindag, Ankara, Turkey
Tel: 00905357687688
E-mail: ldamgaci@hotmail.com
Received date: August 06, 2017; Accepted date: August 16, 2017; Published date: August 21, 2017
Citation: Paşaoğlu L, Toprak U, Üstüner E, Temel E, Özer H, et al. (2017) Are Variations of Paranasal Sinuses and Infundibular Trace Length Responsible for Development of Maxillary Sinusitis? OMICS J Radiol 6:270. doi: 10.4172/2167-7964.1000270
Copyright: © 2017 Paşaoğlu L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Purpose: To determine whether the lenght and width of ethmoid infundibulum relate to maxillary sinusitis. In addition, evaluation of the relationship of maxillary sinusitis to the type of infundibulum and to anatomical sinonasal variations is also aimed to observe.
Materials and methods: Paranasal sinus computerized tomography images of 491 clinically proven rhinosinusitis cases are analyzed retrospectively by two radiologysts. The length is measured by drawing curve traces and width is measured from the narrowest region for 982 ethmoid infundibula in-total. Maxillary sinusitis of the cases is graded according to the Lund and MacKay score. Type, width and length of ethmoid infundibulum and sinonasal anatomical variations are compared for the cases in terms of having with and without maxillary sinusitis.
Results: Type and length of ethmoid infundibulum are found not to be risk factors for maxillary sinusitis (p>0.05). Length of EI are similar between score 0 and score 1-2 maxillary sinusitis (p>0.05) but width was much more in patients with having score 1 and 2 maxillary sinusitis compared with those not having sinusitis (score 0) (p<0.05). Maxillary ostial closure with according expansion of ethmoid infundibulum is seen in maxillary sinusitis. Sinusitis risk is increased in presence of ethmoid bulla. The other anatomical variations can not be determined as risk factors for sinusitis.
Conclusion: In contrary to general belief, paranasal variations do not constitute risk for maxillary sinusitis apart from ethmoid bulla. Type and trace length of infundibulum are not risk factors for sinusitis. Ethmoid infundibulum is expanded with sinusitis.
Keywords
Ethmoid infundibulum; Maxillary sinusitis; Computed tomography
Introduction
The Ostiomeatal Complex (OMC) is a drainage mechanism for maxillary, frontal, anterior and posterior ethmoid cells. The OMC is composed of ethmoid infundibulum, uncinate process, ethmoid bulla, semilunar hiatus and medial meatus. Normal mucociliary drainage is related to ostium opening. Even with open ostium, a breakdown of mucociliary drainage, accumulating mucus and resulting with infection are claimed to occur in the contact of two opposing mucosal surface. Obstruction with mucociliary drainage dysfunction resulting in repeated inflammatory sinonasal diseases is thought to occur. Ethmoid Infundibulum (EI) which forms the main constitution of OMC was found to be wider and shorter than normal in children with acute complicated sinusitis and the uncinate process which forms the medial wall of the EI was found shorter in another study conducted on adults with chronic sinusitis.
The relation between sinonasal anatomical variations and sinonasal infections is not clear. While some researchers have claimed that anatomical variations increase chronic sinusitis risk, other researchers have not found a relation between sinonasal variations and sinusitis. Showing sinonasal anatomical variations before functional endoscopic sinus surgery blocks the possible complications. Computed Tomography (CT) is the preferred imaging modality for demonstrating sinonasal variations and pathologies. In this study, the anatomical variations of the OMC, in particular the length and width of EI are studied in relation to maxillary sinusitis and ostiomeatal disease to detect whether a correlation exists [1-21].
Material and Methods
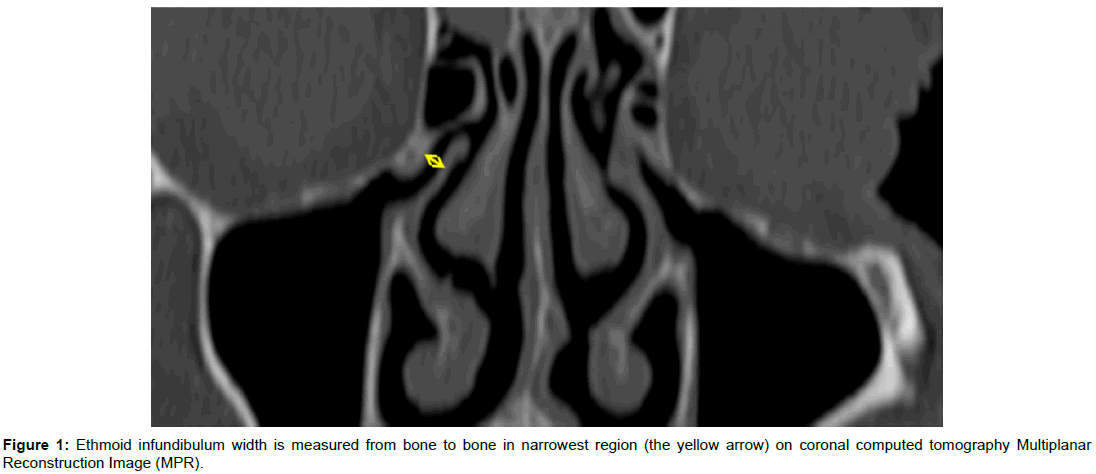
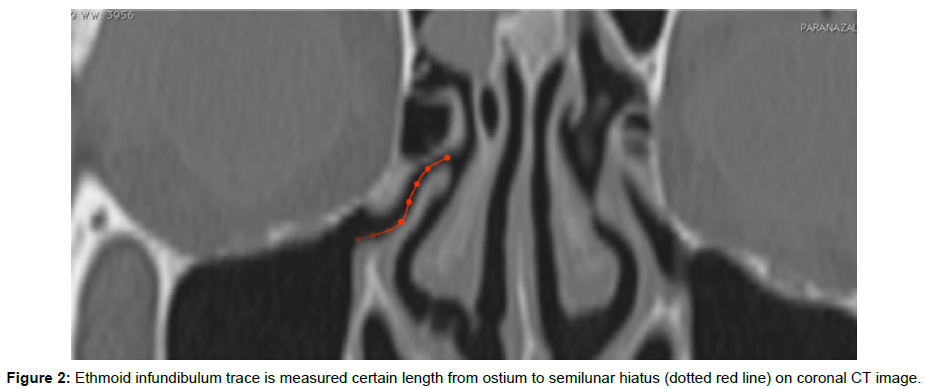
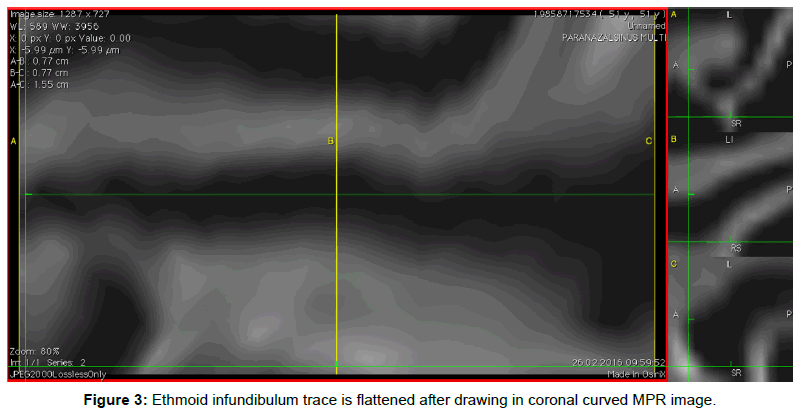
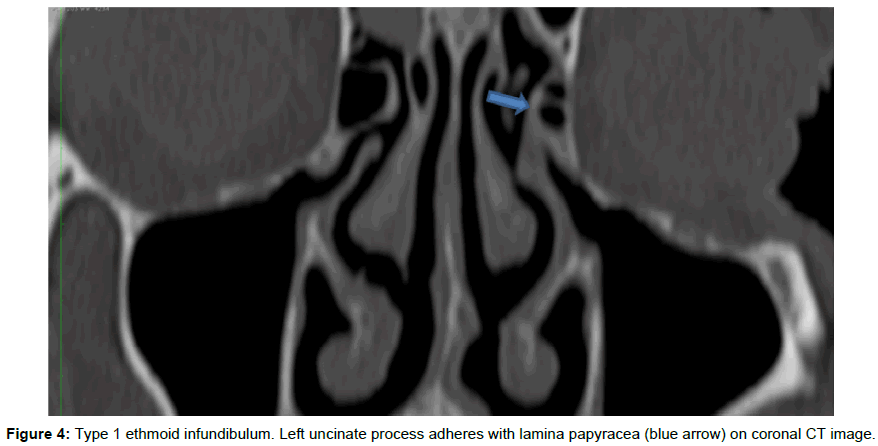
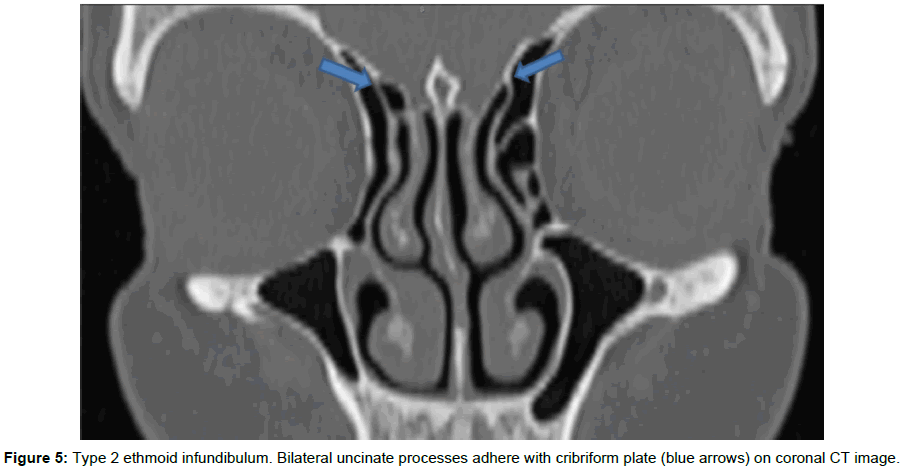
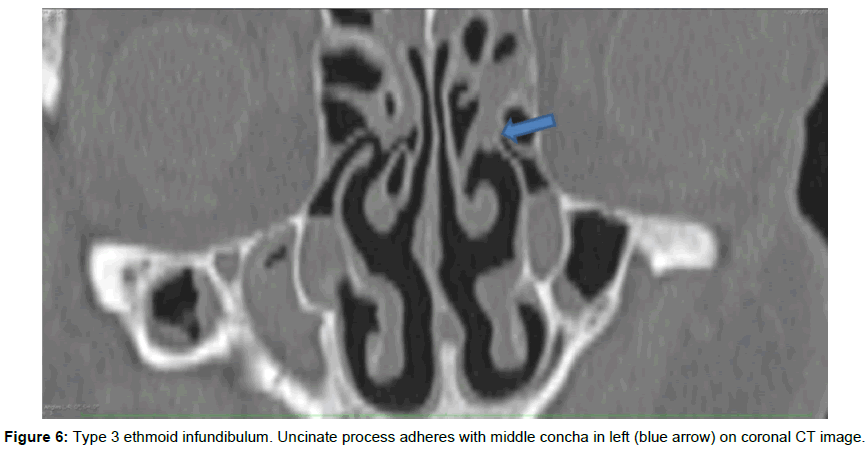
Local ethics committee approval was obtained. Images of 200 (40.7%) females average age 40.36 ± 13.99 and 291 (59.3%) male with average age of 38 (12-85) totaling 491 cases with clinically proven rhinosinusitis are studied by use of scanning paranasal CT without contrast. Postoperative cases, those having sinonasal polyposis or sinonasal malignancy cases are excluded from the study. Paranasal CT images are acquired from the PACS retrospectively. Scans are performed with 64 slice (Aquilion 64, Toshiba Medical Systems, 2011, Japan) CT device. Scanning parameters in 64 detectors CT were as follows: FOV: 16 cm, collimation 64 × 1, gantry rotation time 0.6 s, slice thickness 1 mm, step value 0.64, 120 kV and 250 mA. Anterior and lateral scanogram are performed after patients lying down in supine position. Scanning in axial plan is realized from frontal sinus roof to mandible. The images are evaluated using Osirix soft ware (7.0, 64 bit, Switzerland). CT images of all the cases are evaluated by two exprienced radiologists. Coronal and sagittal Multiplanar Reconstruction (MPR) images are obtained through axial images. Infundibulum widths are calculated coronal plan images with 950% augmentation from uncinate process to outward contour of orbital medial wall (Figure 1). Infundibulum length is measured coronal plan 3-D curved multiplanar reconstruction imaging with 100% augmentation drawing trace from ostium to semilunar hiatus (Figures 2 and 3). Uncinate process adhering with lamina papyracea is classified as type 1, cribriform plate as type 2, middle concha as type 3 EI (Figures 4-6). Anatomical variations such as Haller cell, uncinate aeration, ethmoid bulla, middle turbinate lamella aeration, bullous middle turbinate, paradoxical middle turbinate, septum deformity are recorded. Maxillary sinusitis is graded according to Lund and MacKay score.
Score 0: No abnormality.
Score 1: Partial opacification.
Score 2: Total opacification.
Statistical Analysis
One way variance analysis (One way ANOVA) is used to compare between maxillary sinusitis score and EI length, width. Chi square test is used to compare between sinusitis score and nominal variants (sinus type, variations). Score 0 maxillary sinus is grouped as sinusitis is absent. Score 1 and 2 grouped as “sinusitis is present”. T test is used to evaluate the difference between length and width, chi square test is used to compare with nominal variants and sinusitis status (present-absent) for these two groups. Independent variants (sinus type and variations) that can affect sinusitis existence are analyzed by logistic regression analysis. SPSS 11.5 package program is used in analysis and p<0.05 is accepted as statistically significant level.
Results
Average EI length of 982 subjects were 1.33 ± 0.29 (0.45-2.57) (Min-Max) milimeters. Average EI width were 2.01 ± 0.64 (0.58-6.69)) (Min-Max) milimeters. 662 (67.4%) of 982 ethmoid infundibula were Type 1, 139 (14.2%) were Type 2, 181 (18.4%) were type 3. Of all 982 subjects, 294 (29.9%) have score 0, 614 (62,6%) have score 1, and 74 (7, 5 %) have score 2 maxillary sinusitis. Score 0 maxillary sinus subjects were considered as control group. Haller cell was encountered in 864 (88%), aerated uncinate process in 880 (89.6%), ethmoid bulla in 489 (49.8%), bullous middle turbinate in 556 (75.5%), paradoxical middle turbinate in 820 (83.5%).
There was no relation between sinusitis scores and infundibulum length (p>0.05).
Length of EI are similar between scores 0-2 maxillary sinusitis (p>0.05) but width was much more in patients with having score 1 and 2 maxillary sinusitis compared with those not having sinusitis (score 0) (p<0.05) (Table 1).
| Sinusitis present (N=294) | Sinusitis absent (N=688) | p | |
|---|---|---|---|
| Average ± SD | Average ± SD | ||
| EI Length | 1.31 ± 0.25 | 1.33 ± 0.31 | 0.320 |
| EI Width | 1.93 ± 0.56 | 2.04 ± 0.66 | 0.006* |
Table 1: Relation between sinusitis existence and infundibulum dimensions.
The relation between sinusitis scores, infundibulum type and paranasal variations is summarized in Table 2. A relation between sinusitis scores and infundibulum types is not found (p>0.05). Haller cells are more frequent in score 1 (p<0.05). Sinusitis scores and uncinate aeration are not related to each other (p>0.05).
| Score 0 | Score 1 | Score 2 | p | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Infundibulum Type | |||||||
| 1 | 184 | 27.8 | 428 | 64.6 | 50 | 7.6 | 0.060 |
| 2 | 52 | 37.4 | 78 | 56.1 | 9 | 6.5 | |
| 3 | 58 | 32 | 108 | 49.7 | 15 | 8.3 | |
| Haller Cell | |||||||
| Absent | 254 | 29.4 | 538 | 62.3 | 72 | 8.3 | 0.024* |
| Present | 40 | 33.9 | 76 | 64.4 | 2 | 1.7 | |
| Aerated Uncinate | |||||||
| Absent | 263 | 29.9 | 547 | 62.2 | 70 | 8 | 0.498 |
| Present | 31 | 30.4 | 67 | 65.7 | 4 | 3.9 | |
| Ethmoid Bulla | |||||||
| Absent | 126 | 25.8 | 306 | 62.6 | 57 | 11.7 | 0.001* |
| Present | 168 | 34.1 | 308 | 62.5 | 17 | 3.4 | |
| Lamellar Aeration | |||||||
| Absent | 157 | 28.2 | 348 | 62.6 | 51 | 9.2 | 0.014 |
| Present | 137 | 32.2 | 266 | 62.5 | 23 | 5.4 | |
| Bullous Concha | |||||||
| Absent | 212 | 28.6 | 469 | 63.3 | 60 | 8.1 | 0.077 |
| Present | 82 | 34 | 145 | 60.1 | 14 | 5.8 | |
| Paradoxical Middle Concha | |||||||
| Absent | 243 | 29.6 | 515 | 62.8 | 62 | 7.6 | 0.811 |
| Present | 51 | 31.5 | 99 | 61.1 | 12 | 7.4 | |
| Septum Deformity | |||||||
| Absent | 74 | 35.6 | 111 | 53.4 | 23 | 11.1 | 0.038* |
| Present | 220 | 56.9 | 431 | 129.9 | 51 | 13.1 | |
Table 2: Relation between infundibular type-paranasal variations and sinusitis score.
There is relation between sinusitis score and ethmoidal bulla (p<0.001). Ethmoid bulla is more frequent in score 1 maxillary sinusitis. Middle turbinate lamellar aeration is similar in score 0 and 1-2 patients. Any relation is not detected between sinusitis score and bullous middle concha (p>0.05). There were no significant difference between sinusitis score and paradoxical middle concha frequencies. Score 1 sinusitis is more frequent compared with score 0 and 2 sinusitis in patients with septum deformity (p<0.05). The relation between infundibulum type, paranasal variations and sinusitis scores is shown in Table 3. Ethmoid bulla is more frequent in patients who had score 1-2 sinusitis in comparison with those score 0 maxillary sinuses (p<0.01). Independent variants (infundibulum type, length, variations) that can affect existence of sinusitis are inserted in a logistic regression analysis and risk factors affecting sinusitis existence are analyzed by retrospective elimination method. An end logistic model is generated with statistically significant variants. Ethmoid bulla is found to be an independent risk factor affecting the existance of sinusitis with regard to this model. Sinusitis risk is increased 1.489 fold in patients had ethmoid bulla (Table 4).
| Sinusitis Present (N=294) | Sinusitis Absent (N=688) |
p | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Type of Infundibulum | |||||
| 1 | 184 | 27.8 | 478 | 72.2 | 0.063 |
| 2 | 52 | 37.4 | 87 | 62.6 | |
| 3 | 58 | 32 | 123 | 68 | |
| Haller Cell | |||||
| Absent | 254 | 29.4 | 610 | 70.6 | 0.314 |
| Present | 40 | 33.9 | 78 | 66.1 | |
| Aerated Uncinate | |||||
| Absent | 263 | 29.9 | 617 | 70.1 | 0.916 |
| Present | 31 | 30.4 | 71 | 69.6 | |
| Ethmoidal Bulla | |||||
| Absent | 126 | 25.8 | 363 | 74.2 | 0.004* |
| Present | 168 | 34.1 | 325 | 65.9 | |
| Lamellar Middle Concha | |||||
| Absent | 157 | 28.2 | 399 | 71.8 | 0.184 |
| Present | 137 | 32.2 | 289 | 67.8 | |
| Bullous concha | |||||
| Absent | 212 | 28.6 | 529 | 71.4 | 0.111 |
| Present | 82 | 34 | 159 | 66 | |
| Paradoxical Middle Concha | |||||
| Absent | 243 | 29.6 | 577 | 70.4 | 0.639 |
| Present | 51 | 31.5 | 111 | 68.5 | |
| Septum Deformity | |||||
| Absent | 74 | 35.6 | 134 | 64.4 | 0.135 |
| Present | 220 | 56.5 | 554 | 143.1 | |
Table 3: Relation between existence of sinusitis and type of infundibulum-paranasal variations.
| Odds ratio | 95% CI | p | |
|---|---|---|---|
| Without Ethmoidal Bulla | 1 | - | - |
| With Ethmoidal Bulla | 1. 489 | 1.131 - 1.961 | 0.005 |
Table 4: Relation between sinusitis existence and ethmoid bulla.
Discussion and Conclusion
The OMC is comprised of ostium of the frontal sinus, frontal recess, maxillary sinus ostium, ethmoid infundibulum and middle meatus. Ethmoid infundibulum is the air passage connecting the maxillary sinus ostium to the middle meatus. The uncinate process comprises the medial wall. The lateral wall is formed by the lamina papyracea and frontal process of maxilla and the ethmoid bulla form the posterior wall. EI mainly drains the maxillary sinus [4,10]. It is thought that interference with the drainage process causes sinusitis. Whether bony alterations or mucosal pathologies at the OMC cause the obstruction, is a matter of ongoing debate. Study researching the relation between EI length, width and maxillary sinusitis is limited in literature. Thorp et al. [21] report that the infundibulum is shorter and wider in children with acute sinusitis than in healthy children. Also they report that mucosal changes play a role more than bony changes in the ostiomeatal complex for sinusitis pathogenesis. Pruna [16] made 15 different quantitative measures of structures forming the OMC and report the uncinate process length is shorter in patients with sinusitis. Messerklinger [14] reports the anatomical variations of the middle meatus and infundibulum trigger inflammation by narrowing sinus ostia and the disease extends from there to the other related sinuses.
Treatment modalities are also based upon the bony narrowing concept and therefore aim to widen the drainage routes for example by removing the uncinate process. Our study contradicts this while showing EI length measured drawing trace is not a risk factor for maxillary sinusitis. The ostium is found closed in patients with sinusitis. The infundibulum is widened probably due to the mass effect of inflammatory secretion and decreased mucociliary activity.
A lot of anatomical variations are seen in paranasal sinuses. Certain studies claim some anatomical variations cause inflammation and chronic rhinosinusitis by obstructing sinus drainage ways [6,7,17,20]. On the contrary, Kim et al. [9], Lerdlum et al. [11], Stallman et al. [20] and Katia et al. [17] report there is no relation between anatomical variations and rhinosinusitis as well as that local, systemic, environmental factors and intrinsic mucosal disease are more important in chronic rhinosinusitis pathogenesis. In the study any relation between Haller cell and sinusitis is not detected, on the contrary Haller cell is rarer in patients with sinusitis. A statistical relation between Haller cell existence and maxillary sinusitis is not detected by cone beam CT imaging in Mathew et al. [13]. Also, the relation is not detected in some other studies [9,15,19,20]. On the other hand, there is one study claim that Haller cell existence and narrow infundibulum are related to recurrent acute rhinosinusitis [1]. Nasal septum deformity is seen in 90% of population [1,6,17,22]. Orlandi et al reported that type 3 nasal deformity according to Mladina’s classification has the higher frequency among chronic rhinosinusitis patients [23]. In our study, septal deformities are more frequent in score 1 maxillary sinusitis.
Fadda et al. report ethmoid bulla and ethmoid sinusitis are not related to each other [6]. A study claims there is assosiation between a big ethmoid bulla and maxillary sinusitis [18]. A relation between maxillary sinusitis and bullous concha is not statistically significant in some studies [16,17]. In our study ethmoid bulla is more frequent in patients who had score 1-2 sinusitis in comparison with those score 0 maxillary sinuses so there is correlation of maxillary sinusitis and ethmoid bulla. Ethmoid bulla can narrow the EI and cause maxillary sinusitis.
Bullous concha characterized by bullous part of middle concha pneumatization is reported 9-20%. Maxillary and ethmoid sinusitis can be formed because of bullous and deformed middle concha narrowing middle meatus in some studies [18]. Bullous concha and maxillary sinusitis are not related to each other in Smith et al. study with 883 patients [19]. Bullous middle concha paradoxical middle concha and maxillary sinusitis are not related to each other in our study. Also no significant difference is seen between the sinusitis score, bullous middle concha and paradoxical middle concha rates. However septal deformity is found more frequent in score 1 maxillary sinusitis.
There are some limitations in our study. The concurrence of different anatomical variations has not researched. Medial and lateral deviations of uncinate process are not evaluated. We did’nt calculate the volume of EI. EI volume may be more useful for evaluating the relation with the maxillary sinusitis. Before functional endoscopic sinus surgery reporting anatomical variations is necessary. Because existence of these anatomical variations can affect surgical approaches. These are important for preventing possible complications during surgery [12]. Our study declares the researched variations do not increase sinusitis risk except ethmoid bulla. It is thought that even if a long infundibulum tends to be obstructed and causes sinusitis in general, this condition is not important in the case of sufficient mucociliary activity.
Disclosure of Interest
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Alkire BC, Bhattacharyya N (2010) An assessment of sinonasal anatomic variants potentially associated with recurrent acute rhinosinusitis. Laryngoscope 120: 631-634.
- Al-Qudah M (2008) The relationship between anatomical variations of the sino-nasal region and chronic sinusitis extension in children. Int J Pediatr Otorhinolaryngol 72: 817-821.
- Azila A, Irfan M, Rohaizan Y, Shamim AK (2011) The prevalence of anatomical variations in osteomeatal unit in patients with chronic rhinosinusitis. Med J Malaysia 66: 191-194.
- Babbel RW, Harnsberger HR, Sonkens J, Hunt S (1992) Recurring patterns of inflammatory sinonasal disease demonstrated on screening sinus CT. AJNR 13: 903-912.
- Basu S, Georgalas C, Kumar BN, Desai S (2005) Correlation between symptoms and radiological findings in patients with chronic rhinosinusitis: an evaluation study using the Sinonasal Assessment Questionnaire and Lund-Mackay grading system. Eur Arch Oto-Rhino-Laryngology Head Neck 262: 751-754.
- Fadda GL, Rosso S, Aversa S, Petrelli A, Ondolo C, et al. (2008) Multiparametric statistical correlations between paranasal sinus anatomic variations and chronic rhinosinusitis. Acta Otorhinolaryngol Ital 32: 244-251.
- Gupta AK, Bansal S, Sahini D (2012) Anatomy and its variations for endoscopic sinus surgery. Clin Rhinol An Int J 5: 55-62.
- Jain R, Stow N, Douglas R (2013) Comparison of anatomical abnormalities in patients with limited and diffuse chronic rhinosinusitis. Intl Forum All Rhinol 3: 493-496.
- Jun Kim H, Jung Cho M, Lee JW, Kim Y, Kahng H, et al. (2006) The relationship between anatomic variations of paranasal sinuses and chronic sinusitis in children. Acta Otolaryngol 126: 1067-1072.
- Kennedy DW, Bolger WE, Zinreich SJ (2001) Diseases of the sinuses: diagnosis and management: PMPH-USA.
- Lerdlum S, Vachiranubhap B (2005) Prevalence of anatomic variation demonstrated on screening sinus computed tomography and clinical correlation. J Med Assoc Thai 88: 110-115.
- Maru Y, Gupta V (2001) Anatomic variations of the bone in sinonasal CT. Ind J Otolaryngol Head Neck Surg 53: 123-128.
- Mathew R, Omami G, Hand A, Fellows D, Lurie A (2013) Cone beam CT analysis of Haller cells: prevalence and clinical significance. Dentomaxillofacial Radiol 42: 20130055.
- Messerklinger W (1994) Background and evolution of endoscopic sinus surgery. Ear Nose Throat J 73: 449-450.
- Nouraei S, Elisay A, Dimarco A, Abdi R, Majidi H, et al. (2009) Variations in paranasal sinus anatomy: implications for the pathophysiology of chronic rhinosinusitis and safety of endoscopic sinus surgery. J Otolaryngol Head Neck Surg 38: 32.
- Pruna X (2003) Morpho-functional evaluation of osteomeatal complex in chronic sinusitis by coronal CT. Eur Radiol 13: 1461-1468.
- Shpilberg KA, Daniel SC, Doshi AH, Lawson W, Som PM (2015) CT of anatomic variants of the paranasal sinuses and nasal cavity: poor correlation with radiologically significant rhinosinusitis but importance in surgical planning. AJR 204: 1255-1260.
- Sivasli E, Sirikçi A, Bayazýt YA, Gümüsburun E, Erbagci H, et al. (2003) Anatomic variations of the paranasal sinus area in pediatric patients with chronic sinusitis. Surg Radiol Anat 24: 399-404.
- Smith KD, Edwards PC, Saini TS, Norton NS (2010) The prevalence of concha bullosa and nasal septal deviation and their relationship to maxillary sinusitis by volumetric tomography. Intl J Dentistry.
- Stallman JS, Lobo JN, Som PM (2004) The incidence of concha bullosa and its relationship to nasal septal deviation and paranasal sinus disease. AJNR 25: 1613-1618.
- Thorp MA, Roche P, Nilssen EL, Mortimore S (1999) Complicated acute sinusitis and the computed tomography anatomy of the ostiomeatal unit in childhood. Int J Pediatr Otorhinolaryngol 49: 189-195.
- Mladina R, Skitarelić N, Poje G, Šubarić M (2015) Clinical implications of nasal septal deformities. Balkan Med J 32: 137-146.
- Orlandi RR, Kingdom TT, Hwang PH, Smith TL, Alt JA, et al. (2016) International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int Forum Allergy Rhinol 6: S3-S21.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 5341
- [From(publication date):
August-2017 - Aug 15, 2025] - Breakdown by view type
- HTML page views : 4394
- PDF downloads : 947