Research Article Open Access
Codification of Islamic Republic of Iran's Emergency Medical Services (EMS) Native Reaction Protocol to Suspected Ebola Patients based on World Protocols
Behrooz Iran Nejhad1*, Ali Jadidi2 and Mehdi Safar Abadi31Emergency Medical Services and Crisis Management of Markazi Province, Arak University of Medical Sciences, Arak, Iran
2School of Nursing and Midwifery, Arak University of Medical Sciences, Arak, Iran
3School of Paramedical Sciences, Arak University of Medical Sciences, Iran
- *Corresponding Author:
- Behrooz Iran Nejhad
MSc in Bioterrorism Counter Management
Emergency Medical Services & Crisis Management of Markazi province
Arak University of Medical Sciences, Arak, Iran
Tel: +989128637936
E-mail: irannejad.b@arakmu.ac.ir
Received Date: June 30, 2016; Accepted Date: September 24, 2016; Published Date: September 30, 2016
Citation: Nejhad BI, Jadidi A, Abadi MS (2016) Codification of Islamic Republic of Iran's Emergency Medical Services (EMS) Native Reaction Protocol to Suspected Ebola Patients based on World Protocols . J Bioterror Biodef 7:151. doi:10.4172/2157-2526.1000151
Copyright: © 2016 Nejhad BI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
Introduction: Biological threats are one of the greatest dangers that threaten national security of different countries. Ebola haemorrhagic fever is one of these threats and there is no guideline that helps us to deal with suspected cases in Emergency Medical Services (EMS) in Iran. Objective: This study has been conducted to develop native guidelines reaction, based on world protocols, in Emergency Medical Services of the Islamic Republic of Iran in facing Ebola. Method: This study is considered literature review and was conducted by library studies. At first we started by identifying the domestic and international organizations and centres then visiting the sites and information resources available, we searched for proper keywords then we collected and localized all guidelines and instructions about dealing with Ebola. In the end a comprehensive chart was provided to determine the way of facing and transporting patients suspected with Ebola by care and pre-hospital emergency personnel. Discussion: Based on general facts, overview guidelines should be useful to establish native compilation that includes planning and preparation, screening (telephone triage) patients, special assessment and transmit team via telephone calls, making necessary coordination with other organizations and units within and outside the organization, preparation for patient transport, preparation and carrying out some activities after transporting and the process of evaluation after transferring patients. Conclusion: To succeed in facing similar diseases, considering the need to write native guidelines for each country according to the generalities mentioned, all organizations and institutions involved, should start working in concert with each other and the instructions and practice manoeuvres should be performed again and again to review and fix bugs.
Keywords
Infectious haemorrhagic fever; Ebola; Bioterrorism; Guidelines, Emergency medical services
Introduction
Bioterrorism and its potential capacity for destruction and genocide is an issue that has increasingly drawn the attention of the world Because it endangers national security and public health communities simultaneously [1]. One of the modified viruses that threatens global security nowadays is Ebola haemorrhagic fever [2]. Ebola was called haemorrhagic fever Ebola in the past. Ebola virus is contagious and lethal. Ebola was identified in the second half of the twentieth century (1976) in Central Africa for the first time. This virus is named after a river that is called Ebola in Congo). From 1976 to 2014, more than 20 outbreaks of Ebola have been reported [3]. Ebola virus is a serious disease that kills more than 90% of patients [2]. Due to the nature of biological threats, the first group of people who encounter the consequences of a biological attack are managers and healthcare centres’ personnel [4]. Among the health centres and their personnel, emergency medical services’ personnel (EMS) are one of the first units that interfere in all natural and man-made disasters and help sick and injured. More precisely Emergency Medical Services’ personnel are usually the only medical staff personnel, present at the scene and they face the primary risk of exposure to biological agents, toxins and radiation [5]. Emergency Medical Services’ personnel should be aware of guidelines, specific disease patterns and diagnostic clues that may help them to detect an act of bioterrorism or a disease outbreak [6]. In dealing with the patients at the scene, Emergency Medical Services’ personnel must take a series of measures in accordance with international standards guidelines [5]. By considering the fact that detecting the presence and distinguishing the type of biological threats is very difficult, developing and having access to standardized guidelines for dealing with threats and reducing injuries and damage caused by them are difficult as well [7]. So far, several medical care guidelines are suggested. Advantages, strengths and weaknesses of these guidelines have been examined [8]. However, there are not any comprehensive guidelines for dealing with biological events then the result is lack of preparation in such circumstances. a study was conducted to evaluate the readiness of Emergency Medical Services’ personnel in Tehran in facing biological events in 1391. All The staff are considered weak in the aspects of teaching, practical training and having regulations and guidelines and necessary equipment [9].
This study has been conducted with the aim of developing operational guidelines In order to respond to suspected cases of haemorrhagic infections fevers’ help request by considering the maximum safety for personnel in Emergency Medical Services.
Materials and Methods
This study is a review and was conducted with the method of library research in which the instructions developed by Emergency Medical Services centres (EMS) and the World Health Organizations developed in European and American countries-, are used as a basic model. These guidelines are modified and developed according to the social and cultural conditions, facilities and equipment’s in the ministry of health and emergency medical services centres, Iran’s strategic geographical location.
At first by identifying the domestic and international organizations and centres, visiting sites and information resources available such as pub med, SID, science direct, Pro Quest, Google Scholar, Scopus, CDC, WHO as well as examining magazines and e-books, we searched for appropriate keywords, such as: guidelines + emergency Medical Services + Ebola haemorrhagic fever + EMS Response Planning to a Suspected Biological / Infectious Disease Incident and then all instructions and guides that might help technicians and emergency centres and ambulances to deal with Ebola were collected.
The criterion of using articles and guidelines in this study was based on the relevance of them to the aims of study. These articles are in English and Persian and were in the form of research or review. According to the procedure and regarding the capacity, the situation in the country and also the application of the guidelines, a model was designed and presented with the title of (Emergency Medical Services Reaction guidelines to patients with suspected Ebola haemorrhagic fever).
These guidelines were analysed and localized according to instructions and regulations of health and treatment ministry and also the common parts were harmonized by professors and experts who studied this field. In the end some headings were considered to develop a practical guideline, including all the necessary tips in Emergency Medical Services from the moment of contacting with the patient And telephone triage till taking the patient to the hospital, normal treatment principle, respiratory-cardio arrest and burying the corpses if it’s necessary and sterilize the ambulance and equipment’s then getting ready to deploy on another mission.
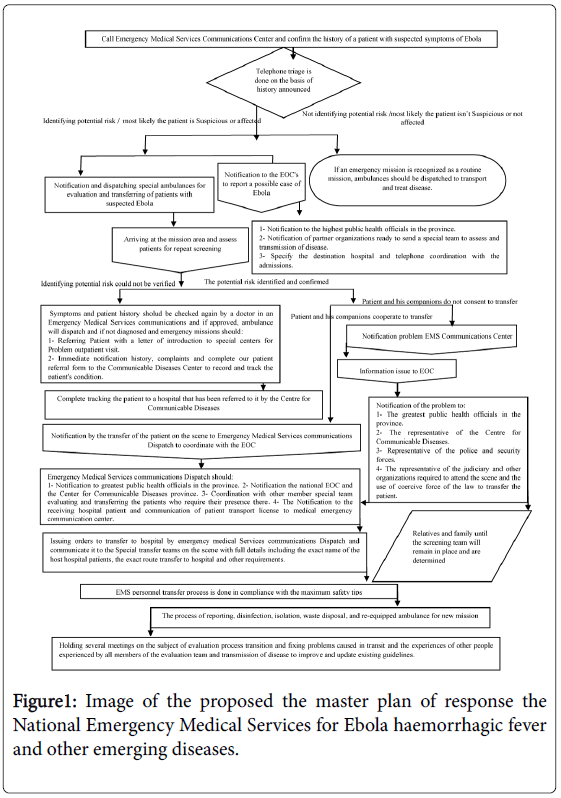
In the end according to gathered information, a comprehensive chart was presented to determine the way of dealing with, protecting and transporting people suspected with Ebola by pre-hospital emergency medical services’ personnel.
Results
Common general guidelines
Planning and preparation: In this part people will be educated about using the policies; all the guidelines and standards will be taught and practiced repeatedly.
How to donning and doffing individual safety equipment, the way of dealing with suspected cases, dealing with bodies and special missions, driving, car repair, ambulance request backup and stuff like this will be practiced and localized completely in this section.
Also choosing special assessment team members, transporting equipment’s and reducing equipment and additional people depending on the type and extent of the disease is considered in this section (Figure 1).
Transmission of equipment consists one ambulance, preferably type A, personal protective equipment’s, medicines and medical equipment that will be used depending on the patients' illness and no equipment and extra drugs should not be carried to the mission [10].
Screening (telephone triage) patients and coordination
If the caller has flu symptoms, he should be asked about a trip to African countries in the past month and the history of contacting suspect cases of Ebola.
In addition, the patients should be asked if they have symptoms like fever higher than 38 degrees Celsius, diarrhoea, nausea, vomiting, abdominal pain, shivering and intense weakness, muscle and joint pain, headache and difficulty in swallowing and if the answer is affirmative, we need to proceed with appropriate caution and informing the conduct Emergency Operations Centre (EOC) and the competent health managers and we should give peace of mind and essential advice to patients and their relatives, then we must dispatch the special transportation infectious patient team.
Emergency Medical Services Communications Unit is responsible for making contacts and coordination between units inside Emergency Medical Services and the and lead Emergency Operations Centre (EOC) is responsible for communicating and coordinating with organizations outside the Emergency Medical Services [11].
Patient transport
Full personal protective equipment for every 3 emergency medical services’ personnel who are in the car escort should be provided and for 2 Paramedic that have direct contact with the patient, two alternative sets and for driver-rescuer 1alternative set should be considered.
Ambulance rear cabin should be isolated completely with a durable plastic layer with a diameter of 6 mm and the connection between the back cabinet and forth cabin must cut off.
All used tools and medicines and serums, if possible, should be put in plastic cover separately in case of not using them, they can be disinfected and re-used in the next mission. All unnecessary equipment’s should be discharged from the rear cabin and the only needed equipment’s are kept in this area. Equipment’s that are not required must be removed before dispatching the ambulance.
If the stretcher has a mattress, it must be covered with a plastic cover with a diameter of 6 mm and also patient should be covered with a plastic cover but that cover must not limit access to the patient's body when he is on a stretcher. Driver required equipment’s such as personal protective equipment, exact map of the transmission path, reliable wireless phone, alternative personal equipment and any other items that he needs should be provided.
Coordination in Internal Emergency Medical Services Units is done by Medical emergency communication Unit (Dispatch) and coordination with organizations outside of Emergency Medical Services is performed by Emergency operations Centre (EOC). Emergency Medical Services personnel must cover the patient with plastic protective cover when they want to put him on the stretcher in addition to covering stretcher mattress [12,13].
Inhibiting the secretion of patients
Inhibition of patients' body fluids is carried out through wound dressing, using surgical mask if the patient can tolerate, using a waterproof cover to cover the patient, collecting the spilled fluid around by placing an absorbent cloth on it, using 10% sodium hypochlorite solution for 10 minutes, collecting the secretion and putting it in the bag Category A for infectious waste [10].
The safety of personnel during patient transport
To protect personnel’s safety paying attention to some points such as trying to limit contact with the patients, giving only necessary health care services to patients, avoidance of cardiopulmonary resuscitation operation, not using the invasive procedures if possible, and using a little resource and a few personnel in transporting patients. A patient who has infectious disease symptoms, but doesn’t have a history of traveling to contaminated areas or contacting with a person who suffers from Ebola and also there is no bleeding or diarrhoea, should be treated like a normal patient.
If the patient has symptoms of infectious disease but no history of traveling to West Africa in past 30 days or any other traveling history, also there is no sign of diarrhoea, vomiting or bleeding, emergency medical services’ personnel should use their usual method of infection control for the patient and they must use appropriate personal protection equipment’s including: two pairs of gloves, masks N95 or N100, gowns, goggles and a face Shield [12].
Clinical care while in transit
For people with the suspected Ebola virus disease pre-hospital care, primary care should be limited. Factors related to advanced life support measures (ALS) include: loss of consciousness, respiratory rate more than 30 breathes per minute, symptoms of shock including ( for example: systolic blood pressure less than 90 mmHg and heart rate above 120 beats per minute). The important thing is that advanced life support measures in these patients are only limited to oral and sublingual administration (For example, anti-vomiting drugs). Creating intravenous open line is done only for those who have signs of shock, or transfer them to the hospital for more than 20 minutes [10].
In facing Patients with acute severe symptoms who are known as people with restraining orders end tracheal intubation (DNI) and the prohibition of carrying out CPR (DNR) we have the permission not to do end tracheal intubation and carrying out CPR in case of cardio respiratory arrest [12].
Calling the centre that accepts and hosts patients and confirming the departure time and also calling the centre some moments before the arriving of the ambulance at the centre should be made by Emergency Medical Services communication (Dispatch) and only by phone. Make sure you enter the hospital in coordination with senior officials at the hospital and using the previous determined route. Regional route between the places that ambulance, carrying the patient, is parked must be controlled and monitored with the building control department and hospital communications and the path intended, for transporting patients should be so wide and flat to allow correct transmission and safety of patients, staff and equipment. The recipient patient's medical personnel are required to wear full personal protective equipment [14].
If the patient is able to move using only one staff is enough. Emergency Medical Services’ personnel and patients must stay inside the ambulance the hospital crew comes. Try to bring a clean stretcher with necessary equipment’s for transmission the patient, close EMS ambulance and also in transferring the patients from ambulance to hospital we should use special track is covered with waterproof sheet. It is better emergency medical services’ personnel don’t interfere in the transferring the patient to his hospital room because the possibility of contamination due to the contamination of clothes and hands, but if they do, after getting off the ambulance the stretcher's wheels and the soles of shoes of procedures staff must be disinfected with sodium hypochlorite 10% [4,11,15,16].
Disinfection equipment and ambulance
Personal protective equipment used in transmission of the patient should be discarded for safe and respected organizations such as CDC guidelines.
In order to discard high-risk personal protective equipment in the area, use a plastic sheet. Doff Personal protective equipment and put them away from your body. Sterilize the Plastic sheet or dispose it safely. Don new personal protective equipment. At first clean the Ambulance then disinfect it. Doff Personal protective equipment.
Throw away used Personal protective equipment used safely. Sterilize the Ambulance inner surface with bleach solution 10% or other approved disinfectants. Sterilize the outer surface of the ambulance with a 10% bleach solution or other approved disinfectants [12-16].
Infectious waste disposal management
The Person who wants to dispose infectious waste should be wearing full personal protective equipment.
All infectious waste should be placed in red bags (Autoclave able) Category A by rolling out each piece of clothes or bed sheets inward slowly in a way that does not produce aerosols of infectious waste. Bags should not be filled more than half. 200 to 300 ml of water should be added to the bag. All the bags should be cleaned with a tissue soaked in 10% sodium hypochlorite. Put the Bags into another garbage bags.
Clean Around the bag again after scotch-taping the rim of the bag and struck it with a cloth soaked in sodium hypochlorite (10%). This bag should be put into an autoclave bag and we purged the bag by soaking it in sodium hypochlorite 10%. After autoclave bags are placed in cardboard boxes for disposal in accordance with the standards [17-21].
Disposing or burying bodies safely
Dead must be prepared and transferred to landfill (burial site) as soon as possible.
The patient's family should be informed about the reasons of cancelling some ceremonies and the importance of special measures that must be done. One of the family members of patients who other family members trust more should be determined to justify and guide family members in the prevention of dangerous actions such as washing and touch the body to be. It is recommended that similar necessary precautions measures especially when we want to isolate patients such as using thick gloves with second pair of rubber gloves (top layer) be considered. Solution of bleach (sodium hypochlorite) 10% must be sprinkled in 2-meter radius around the body. The body of the deceased must be transported in special bags and 10% bleach solution must be sprinkled on waterproof bag containing the body [17-21].
The report of the emergency medical services personnel patient transfer
Oral and written reports about performed measures and the patient's condition during transporting patient should be given to hospital staff by personnel. Emergency Medical Services’ personnel after removing personal protective equipment and disinfect their hands should deliver the mission tab and report to set records.
The overall assessment of the patient transfer process
This section is one of the most important parts of the process of transferring a patient with Ebola haemorrhagic fever and it is divided into two intra-organizational and inter-organizational.
If there is a problem like Finding lack of coordination within an organization or between the responsible agencies in transmission the patient, some joint meetings will be held to discuss and resolve potential failures and correct action guidelines and the results of these meetings will be communicated as a decision to all organizations [12,13,15,16].
Discussion
The ultimate goal of formulating a guideline is making the most of individuals, organizations, troops and equipment in order to do different things better and safer with the lowest financial and human cost trends. By examining the compilations as guidelines, sent to emergency medical services in the country we detected generalization and disruptive content in information at hand, now by considering types of missions in facing and transporting patients suspected of having Ebola by Emergency Medical Services’ personnel there are not available guidelines to help them.
On the other hand, breaking out some emerging diseases such as SARS, bird flu, mad cow disease and now the world's gatherings such as the Hajj and fortieth Hussein (Arbain), such as the FIFA World Cup and Olympics...codification a comprehensive, native, functional and complete guidelines, as the first and most important requirement of any country in response to Ebola and emerging diseases is not considered in ministry of health and treatment.
In reviewing listed foreign guidelines, these guidelines being matched in international organizations in dealing with infectious diseases attract attention, in a way that the base of instructions is the same and only determined according to the cause of epidemic, its transmission power, the isolation level of personnel and equipment’s, following some procedures while transferring the patient, the of level of exposure to the patient and factors like that
In these guidelines we can see a kind of exercised harmonization between organizations responsible for these diseases, such as medical universities, police and security forces, forensics, municipalities, governments, research institutes medical and pharmaceutical, veterinary, fire department and safety measures that represent the unique leadership of these organizations in situations of crisis and outbreak of diseases that it leads to better and safer different actions and also costs will be reduced too.
Conclusion
Based on general facts, Overview guidelines should be useful to established native compilation that includes planning and preparation, screening (telephone triage) patients, special assessment and transmit team via telephone calls, making necessary coordination with other organizations and units within and outside the organization, preparation for patient transport, preparation and carrying out some activities after transporting and the process of evaluation after transferring patients
To succeed in facing these diseases and similar diseases, considering the need to write native guidelines for each country according to the generalities mentioned, all organizations and institutions involved, should start working in concert with each other and the instructions and practice manoeuvres should be performed again and again to review and fix bugs.
General Matters that are Included in these Guidelines
1. Planning and preparation.
2. Screening (telephone triage) patients by making phone calls to special team of evaluating and transferring and also ensuring necessary coordination with other organizations and units within and outside the organization.
3. Preparations for patient transport.
4. Transferring the patient.
5. Preparedness and post-transfer activities.
6. Evaluation after transferring the patient.
Items that Require Adjustment in Accordance with International Guidelines and Objects Country is as Follows
Shortage of technical facilities and equipment
According to prestigious Guidelines institutions specific requirements are considered for personal protective equipment and other equipment, While in most of countries, used equipment for emergency medical technicians are very limited and with low quality.
So firstly authorities should act to increase the quality and quantity of the equipment and secondly, emergency medical technicians should be convinced, if necessary, use the same restrictive means (such as gowns, masks, gloves, face shields, etc) optimally.
Separating pre-hospital emergency levels in many countries
In the review of global studies in some countries pre-hospital emergency is graded into different level to act in different stages in case of having an accident. This allows to the emergency system to give specialized response, while in most countries such a possibility is not provided.
Instead, certain Emergency Medical Services stations can be established for this purpose or in every city an Emergency Medical Services station should be established in order to deal with these events by giving timely and expert response to prevent the situation from getting complicated.
Some recommendations do not fit with the culture, religion and customs of some countries
In some guidelines, some recommendations for handling dead patients, died because of Ebola, in a quite isolated way and in covers that minimize the risk of spreading the infection or some items such as quarantine people and relatives, not giving the permission of holding normal funeral and not to permit the transfer and treatment, etc. can be seen.
While these recommendations in some countries do not fit the culture and religion and customs and this issue is a serious barrier in the way of adoption and implementation of these guidelines.
Therefore it is necessary to provide people trainings on the disease and use help of characters like Clergymen and people who have the ability to influence public opinion in times of need that such recommendations could be implemented.
In review studies and guidelines provided by international organizations, keen attention to manoeuvre and practical exercises and holding several meetings to review the implementation of guidelines is considered at the time of dealing with the disease.
The importance of this issue is very high that, on the basis of existing studies and research, money spent for manoeuvre in most countries is several times higher than the cost to provide ambulance and equipment needed to deal with the epidemic or bioterrorist threats.
This reflects that awareness, preparedness, training, manoeuvres, guidelines, all is considered as key factors to make an appropriate response by medical emergency centres’ Personnel, and other public health organizations in facing patients with haemorrhagic fevers and out breaking emerging diseases and emerging infectious
This can act as a guide for responsible organizations to plan using the resources and manpower effectively and efficiently to respond to the crisis and the diseases.
The history and experiences of other countries such as America, Britain, Ireland and organizations such as the World Health Organization in the field of public health shows Emergency Medical Services and all organizations in these countries use these guidelines as a way to facilitate dealing with infectious haemorrhagic, and by modifying and practicing developed guidelines they could deal with out braking such diseases with minimal additional cost and less worries and they show satisfaction and peace of mind in case of an accident.
To succeed in dealing with this disease and similar disorders all authorities, especially officials and all components must act comprehensively and all mentioned parts in the process should be considered in developing guidelines by all organizations.
Team work and repetition of the discussion in conducted manoeuvres between experts in charge of an organization or between organizations is necessary and major joint exercises for reasons such as the impact on the learning process, creating appropriate procedures, simulating possible scenarios, operational team training and identifying potential problems are of crucial value.
References
- Sundström JF, Albihn A, Boqvist S, Ljungvall K, Marstorp H, et al. (2014) Future threats to agricultural food production posed by environmental degradation, climate change, and animal and plant diseases–a risk analysis in three economic and climate settings. Food Security 6: 201-215.
- Flint M, Goodman CH, Bearden S, Blau DM, Amman BR, et al. (2015) Ebola Virus Diagnostics: The US Centres for Disease Control and Prevention Laboratory in Sierra Leone, August 2014 to March 2015. J Infect Dis 361.
- Kinloch-de LS, Brown CS (2015) International Congress on Targeting Ebola: 28-29 May 2015, Pasteur Institute, Paris. Journal of Virus Eradication 1: 282.
- Fardhosseini MS, Esmaeili B, Wood R (2015) A strategic safety-risk management plan for recovery after disaster operations 106: 1-10.
- Hsia RY, Thind A, Zakariah A, Hicks ER, Mock C (2015) Prehospital and emergency care: updates from the disease control priorities. World journal of surgery 39: 2161-2167.
- Levy M, Royne MB, Koch RW (2016) Civilian-military interface in catastrophes requiring aeromedical evacuation. International Journal of Emergency Management 12: 136-151.
- Wagar E (2016) Bioterrorism and the role of the clinical microbiology laboratory. Clinical microbiology reviews 29: 175-189.
- Üstün AK, Barbarosoğlu G (2015) Performance evaluation of Turkish disaster relief management system in 1999 earthquakes using data envelopment analysis. Natural Hazards 75: 1977-1996.
- Djalali A, Della CF, Segond F, Metzger MH, Gabilly L, et al. (2016) TIER competency-based training course for the first receivers of CBRN casualties: a European perspective. European journal of emergency medicine.
- Adams A, Boualam L, Diorditsa S, Gregory C, Jee Y, et al. (2014) Maintaining Polio-Free Certification in the World Health Organization Western Pacific Region for Over a Decade. Journal of Infectious Diseases 210: S259-S267.
- (2015) Control CfD, Prevention. Guidance on personal protective equipment (PPE) to be used by healthcare workers during management of patients with confirmed Ebola or persons under investigation (PUIs) for Ebola who are clinically unstable or have bleeding, vomiting, or diarrhoea in US Hospitals, including procedures for donning and doffing PPE. Vomiting, or Diarrhoea in US Consult ado a 30.
- Fitzpatrick G, Vogt F, Moi GO, Black B, Santantonio M, et al. (2014) Describing readmissions to an Ebola case management centre (CMC) Sierra Leone 2014. Eurosurveillance 19: 20924
- (2014) How to conduct safe and dignified burial of a patient who has died from suspected or confirmed Ebola virus disease. WHO.
- Isakov A, Jamison A, Miles W, Ribner B (2014) Safe management of patients with serious communicable diseases: recent experience with Ebola virus. Ann Intern Med 161: 829-830.
- Jelden KC, Gibbs SG, Smith PW, Schwedhelm MM, Iwen PC, et al. (2015) Nebraska Biocontainment Unit patient discharge and environmental decontamination after Ebola care. American Journal of Infection Control 43: 203-205.
- Lowe JJ, Jelden KC, Schenarts PJ, Rupp LE, Hawes KJ, et al. (2015) Considerations for safe EMS transport of patients infected with Ebola virus. Prehospital Emergency Care 19: 179-183.
- Hewlett AL, Varkey JB, Smith PW, Ribner BS (2015) Ebola virus disease: preparedness and infection control lessons learned from two biocontainment units. Current Opinion in Infectious Diseases 28: 343.
- Heymann DL (2015) Ebola: burying the bodies. The Lancet 386: 1729-1730.
- Nielsen CF, Kidd S, Sillah A, Davis E, Mermin J et al.(2015) Improving burial practices and cemetery management during an Ebola virus disease epidemic-Sierra Leone, 2014. MMWR Morb Mortal Wkly Rep 64: 20-27.
- (2014) Ebola virus Disease-Fact SheetWHO.
- (2015) Rapid guidance on the decommissioning of Ebola care facilities WHO.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 11374
- [From(publication date):
September-2017 - Sep 01, 2025] - Breakdown by view type
- HTML page views : 10429
- PDF downloads : 945