Case Report Open Access
CT Assisted Diagnosis, Management of Soft Tissue Cervicofacial Emphysema and Pneumomediastinum during Root Canal Treatment of an Upper Premolar: A Case Report
Navin Mishra* and Isha Narang
Senior Resident, Department of Conservative Dentistry and Endodontics, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India
- *Corresponding Author:
- Navin Mishra
Senior Resident
Department of Conservative Dentistry and Endodontics
Centre for Dental Education and Research
All India Institute of Medical Sciences New Delhi, India
Tel: 11 2658 8500
E-mail: navinpdch@gmail.com
Received Date: November 25, 2014; Accepted Date: January 27, 2015; Published Date: February 02, 2015
Citation: Navin Mishra, Isha Narang (2015) CT Assisted Diagnosis, Management of Soft Tissue Cervicofacial Emphysema and Pneumomediastinum during Root Canal Treatment of an Upper Premolar: A Case Report. J Oral Hyg Health 5:1000169. doi: 10.4172/2332-0702.1000169
Copyright: © 2015 Navin Mishra. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Aim: To discuss the iatrogenic cervicofacial emphysema and pneumomediastinum after endodontic treatment of maxillary premolar.
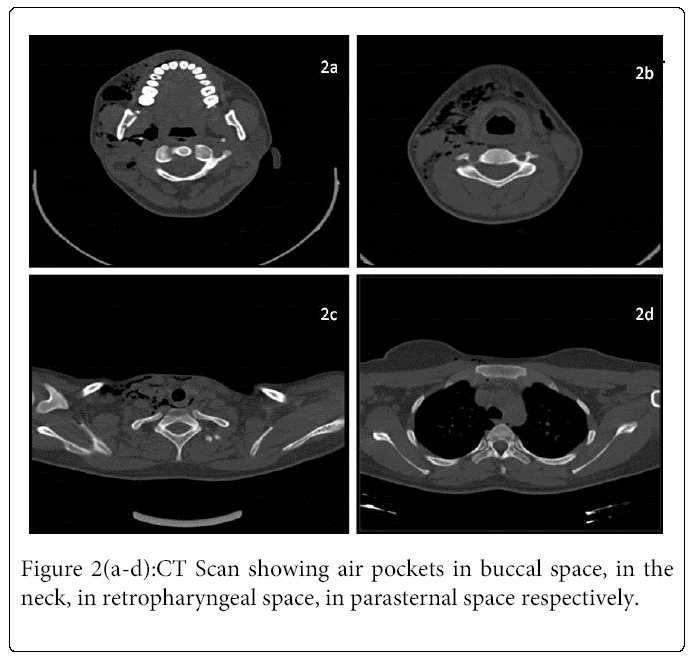
Summary: A 25-year-old female was referred to the department with considerable swelling on the right side of face. She gave a history of progressive swelling with mild difficulty in breathing and swallowing 15 minutes after endodontic treatment of an upper right first premolar. The tooth was accessed by a private practitioner using high speed air driven handpiece without the use of rubber dam and compressed air was used to dry the canals. On examination, swelling extended from right peri-orbital region to the neck bilaterally. It was soft, non-erythematous and showed crepitations without pain. The microbiological tests showed no evidence of infection. A Computed tomogram of the thoracocervicofacial region confirmed the diagnosis of cervicofacial emphysema with pneumomediastinum. She was kept on antibiotics and analgesics for 7 and 3 days respectively. Patient showed regression of swelling, dyspnoea and dysphagia on follow up visit after 48 hours.
Key learning point: Early diagnosis and management of such cases is of extreme importance to prevent possible cardiopulmonary complications and infections. Computed tomography scans are very useful in diagnosis and to determine the extension of air into the tissue spaces.
Keywords
Computed tomography; Emphysema; Pneumomediastinum
Introduction
Cervicofacial emphysema is a clinical condition caused by inadvertent introduction of compressed air in the subcutaneous tissue of the head and neck. It is mainly caused by trauma, head and neck surgery, general anaesthesia [1], and rarely by dental treatment [2]. A comprehensive search of the medical and dental literature from 1993 to 2008 yielded 32 case reports of subcutaneous emphysema due to dental operations [3]. Shovelton in 1957 reported 13 such cases after endodontic treatment [4]. Pneumomediastinum occurs when air leaks from any part of the lung or airways into the mediastinum [5]. It is caused either by a traumatic injury to the chest or increased pressure within the lungs or airways. In 70-90% of the cases of pneumomediastinum, the air rises up to communicating cervical spaces producing subcutaneous cervical emphysema [6] while pneumomediastinum following cervicofacial emphysema is extremely rare and has been reported in the literature after surgical removal of impacted third molar [7,8]. Seventy-four reports of emphysematous complications in ambulatory dental patients were published between the years 1960 and 1993, and were reviewed by Heyman and Babayof in 1995 [9].
We present here a case of iatrogenic subcutaneous emphysema with pneumomediastinum which occurred after endodontic treatment of an upper premolar.
Case Report
A 25-year old woman was referred to the department of Conservative dentistry and endodontics, by a general dental practitioner with considerable swelling on the right side of face. Patient gave a history of progressive swelling with difficulty in swallowing fifteen minutes after an endodontic treatment of the right upper premolar. A high speed air driven handpiece was used by the practitioner for the access cavity preparation and a three way syringe was used to dry the canals. No rubber dam was placed during the procedure.
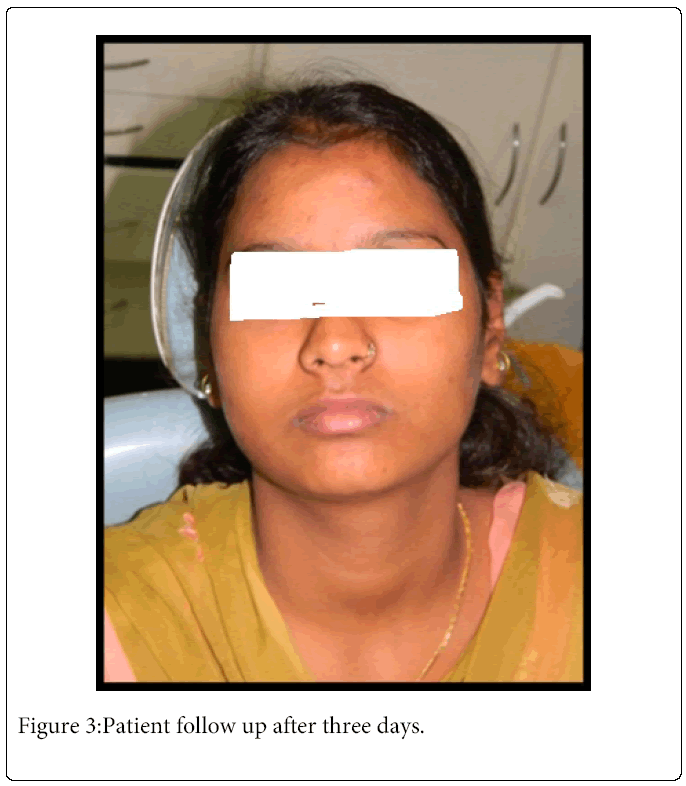
Physical and clinical examination showed significant soft tissue swelling extending from right periorbital region to the neck bilaterally (Figure 1 a-b). On palpation the area was non-erythematous and showed crepitus without pain. Her vital signs were: blood pressure 128/82 mmHg, heart rate 96 beats per minute, respiratory rate 21 breaths per minute and body temperature was 37.1°C orally. Her medical history was noncontributory and had no known allergy to any drugs or local anesthetics. Microbiological tests showed no evidence of infection. Patient was reassured and an immediate computer tomography scan (CT scan) of the head, neck and the thorax region was advised Figure 2 (a-d) which revealed air in the right periorbital region, retropharyngeal area, mediastinum and subcutaneous tissue of the neck. The diagnosis of cervicofacial subcutaneous emphysema with pneumomediastinum was confirmed and patient was put on amoxicillin 500mg and metronidazole 400mg thrice a day, for 7 days and non-steroidal anti-inflammatory ibuprofen 400 mg thrice a day for three days. She was kept on follow up visits after 48 hours and one week. She had an uneventful recovery with resolution of swelling, dyspnoea and dysphagia and normal symmetry of the face was regained (Figure 3).
Discussion
The etiology of cervicofacial emphysema is divided into three categories: Spontaneous which is induced by the patient while coughing [10], secondary after trauma to facial skeleton [11] and iatrogenic after a surgical procedure when air is introduced into the soft tissues [3]. The clinical diagnosis of cervicofacial emphysema is based upon the sudden onset of swelling with crepitation in the absence of erythema, edema, significant tenderness or lymphadenopathy. Pneumomediastinum implies free air within the mediastinum resulting from the rupture of peripheral pulmonary alveoli due to sudden increase of intraalveolar pressure after exaggerated Valsalva maneuver [10]. It was first reported by Turnbull and is usually seen in healthy young men or parturient women. The features suggestive of pneumomediastinum are dyspnea with a brassy voice, chest pain and hamman sign, which is a crunching and bubbling sound caused by movement of air. Pneumomediastinum following cervicofacial emphysema is extremely rare and has been reported after dental surgical procedures [11]. Very few cases have been reported in literature during endodontic treatment. Air may also penetrate into the communicating spaces like parapharyngeal and retropharyngeal spaces through sublingual and submandibular space leading to development of complications like asphyxia. The retropharyngeal space also called as “danger space” is the main route of communication from the mouth to the mediastinum from where the air can reach the pleural, the pericardial and even the retroperitoneal cavity causing pneumothorax, pneumopericardium and death of the patient [13]. This case report discusses the subcutaneous cervicofacial emphysema with pneumomediastinum after endodontic treatment in an otherwise healthy adult. The compressed air from high speed handpieces or three way syringes can enter the subcutaneous tissues of the face and neck and mediastinum during routine dental procedures like extractions [12], restorations, endodontic treatment [14] and extensive oral surgical procedures [11]. These handpieces are air turbine driven and expel high pressure air downwards towards the cutting surface of the bur. In the present case, pain and progressive swelling developed soon after access cavity preparation using an air turbine handpiece and drying the root canal with three way syringe. The gingival sulcus may also be a route for air because the teeth were not isolated with a rubber dam. Most cases of pneumomediastinum and emphysema after endodontic treatment have been related to the use of hydrogen peroxide for irrigating the canals. Sometimes dental burs also lacerate the adjacent mucosa and cause a breach which acts as pathway for air to tract down subcutaneously leading to emphysema. These complications can be prevented by using a rubber dam, electric motor driven handpieces, avoiding the use of the compressed air for drying the root canal after biomechanical preparation, avoiding the use of hydrogen peroxide while irrigating canals [15]. The diagnosis of cervicofacial emphysema and pneumomediastinum depends upon radiologic imaging. Standard posteroanterior and lateral radiographs are usually sufficient for diagnosis as posteroanterior chest radiographs typically demonstrate a radiolucent line between the left heart border and the mediastinal pleura [16]. Other findings may include “highlighting” of the aortic knob and the “contiguous diaphragm” sign. However a CT scan is of utmost importance to know the exact extent of air in soft tissues [17].
The rationale behind antibiotic coverage in these conditions is that the breach in the mucosa almost certainly causes ingress of oral flora which has the potential to infect the subcutaneous tissues.
Conclusion
Although dental procedures seem routine in clinical practice today, they are not without their systemic complications. Air-powered drills or other pressurized appliances used during dental procedures can introduce air into the potential spaces of the face, neck and thorax. The occurrence of sudden swelling during a dental procedure, marked crepitus within the soft tissue, should raise suspicion of subcutaneous emphysema. Assessment for possible infection should be undertaken, and empiric antibiotic therapy for typical oral pathogens can decrease risk of life-threatening complications associated with infectious spread in the facial planes.
References
- Durukan P, Salt O, Ozkan S, Durukan B, Kavalci C (2012) Cervicofacial emphysema and pneumomediastinum after a high-speed air drill endodontic treatment procedure. Am J Emerg Med 30: 2095.
- Smatt Y, Browaeys H, Genay A, Raoul G, Ferri J (2004) Iatrogenic pneumomediastinum and facial emphysema after endodontic treatment. Br J Oral MaxillofacSurg 42: 160-162.
- McKenzie WS, Rosenberg M (2009) Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral MaxillofacSurg 67: 1265-1268.
- Shovelton DS (1957) Surgical emphysema as a complication of dental operation. British Dental Journal 102: 125-129.
- Maunder RJ, Pierson DJ, Hudson LD (1984) Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med 144: 1447-1453.
- Vidal Marsal F, González Olivella J, NualartBerbel L, Torre Alonso L, SauriConejero A, et al. (1984) [Spontaneous pneumomediastinum in the adult. Presentation of 13 cases and review of the literature]. Med Clin (Barc) 82: 797-802.
- Horowitz I, Hirshberg A, Freedman A (1987) Pneumomediastinum and subcutaneous emphysema following surgical extraction of mandibular third molars: three case reports. Oral Surg Oral Med Oral Pathol 63: 25-28.
- Torres-Melero J, Arias-Diaz J, Balibrea JL (1996) Pneumomediastinum secondary to use of a high speed air turbine drill during a dental extraction. Thorax 51: 339-340.
- Heyman SN, Babayof I (1995) Emphysematous complications in dentistry, 1960-1993: an illustrative case and review of the literature. Quintessence Int 26: 535-543.
- Hamman L (1961) Spontaneous mediastinal emphysema. Bulletin of Johns Hopkins Hospital 54: 46-56.
- Oliver AJ, Diaz EM Jr, Helfrick JF (1993) Air emphysema secondary to mandibular fracture: case report. J Oral MaxillofacSurg 51: 1143-1145.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 16198
- [From(publication date):
March-2015 - Aug 22, 2025] - Breakdown by view type
- HTML page views : 11554
- PDF downloads : 4644