Lichen Scrofulosorum in a Patient with Tuberculous Cervical Lymphadenopathy: A case report
Received: 19-Jul-2017 / Accepted Date: 31-Jul-2017 / Published Date: 10-Aug-2017
Abstract
Introduction: Cutaneous tuberculosis (CTB) is a rare presentation of extrapulmonary tuberculosis (TB) with various clinical manifestations. Tuberculids, a type of CTB, are probably the result of hyperergic immune reaction induced by Mycobacterium tuberculosis. Lichen scrofulosorum (LS) is a rare tuberculid mostly seen in children and young adults with or without other manifestations of tuberculosis.
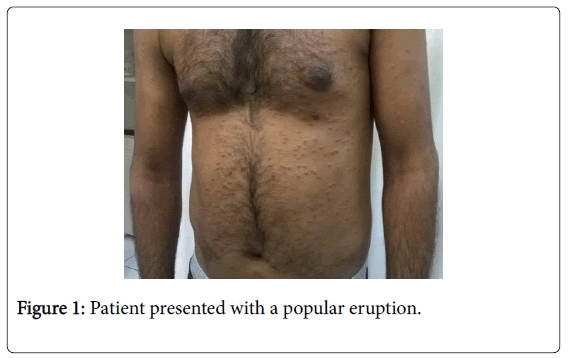
Case report: We present a 30 year old patient presented with a papular eruption on his trunk and upper extremities. The patient had recently started on a 4 drug-regimen treatment for a diagnosed tuberculous cervical lymphadenitis and he was under investigation for pulmonary TB. Histopathology of the papular lesions showed epithelioid granulomas strongly indicating lichen scrofulosorum. The eruption responded to antitubercular therapy with complete clearance of the lesions.
Discussion: The tuberculids are a form of CTB caused by hypersensitivity reactions to Mycobacterium tuberculosis. The diagnosis of LS is problematic and frequently delayed because of its rarity and clinical similarity to many other more common skin conditions.
Abbreviations
TB: Tuberculosis; CTB: Cutaneous tuberculosis; LS: Lichen scrofulosorum; FBC: Full blood count; CXR: Chest X-ray; HIV: Human immunodeficiency virus; PPD: Purified protein derivative; FNA: Fine-needle aspiration
Introduction
Cutaneous tuberculosis (CTB) is a relatively uncommon form of extrapulmonary tuberculosis (TB). Even in countries such as India and China where TB still commonly occurs, cutaneous outbreaks are rare. However the rates of TB are expected to rise due to immigration from TB endemic countries, emergence of human immunodeficiency virus infection (HIV) and the increase in use of immunosuppressive treatments. This can be seen in a study by Varshney et al., which reports that the overall incidence of cutaneous manifestations of TB was found to be 0.7% (131 of 18,720 patients), slightly higher than the incidence demonstrated in other studies from India [1]. The incidence of lichen scrofulosorum (LS), a tuberculid and therefore a form of CTB, varies between 2% and 11.4% in different studies among the cases of CTB but it has been reported as high as 23.5% to 33% in children [1,2].
Tuberculids are exanthems possibly induced by a hyperergic response to mycobacteria and/or their fragments released from a different focus of concomitant or past infection [3,4]. LS is presenting as a lichenoid eruption of small papules most commonly seen in children and adolescents with TB. The lesions are usually asymptomatic, closely grouped, skin-colored to reddish-brown papules, often perifollicular and are mainly found on the abdomen, chest, back, and proximal parts of the limbs. The eruption is usually associated with a strongly positive tuberculin reaction.
Case Report
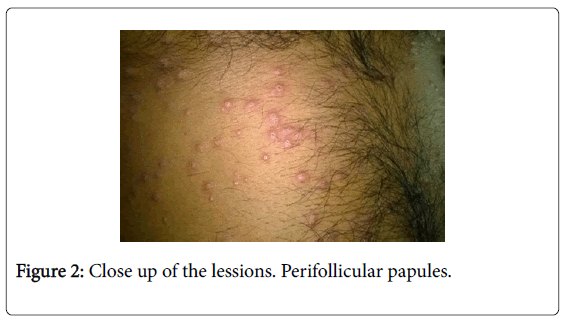
A 30-year-old Pakistani man was referred to our clinic because of an eruption consisting of multiple small erythematous to skin-colored, mostly perifollicular papules over his trunk and humeral areas of his upper limps since 8 days (Figure 1 and 2).
The eruption was described as asymptomatic. Examination of hair, nails and mucosal surfaces was normal.
The patient was under the care of the TB unit of a hospital for chest diseases in Athens and he was receiving a 4-drug regimen including isoniazid, rifampin, pyrazinamide and ethambutol for less than a month.
The patient resorted to the TB unit due to a febrile syndrome cough and right sided painless cervical lymphadenopathy. Workup in the TB unit disclosed a raised erythrocyte sedimentation rate (~60 mm), while full blood count (FBC), chest X-ray (CXR), blood biochemistry and urinalysis were normal or insignificant. Serologic tests for HIV, hepatitis B and C viruses and for syphilis were negative.
The Mantoux skin test was strongly positive with an induration of 25 mm. The patient also underwent a fine needle aspiration (FNA) biopsy on one cervical lymph node, which demonstrated granular eosinophilic material (caseation), multinucleated giant cells, epithelioid cells, neutrophils and lymphocytes.
Staining for acid-fast bacilli was positive. The patient was also under further investigation for possible occult pulmonary TB because the initial workup had not established the definite involvement of the lungs.
Our initial impression of the rash was that it could be a possible lichenoid drug eruption but the combination of medical history and clinical presentation was highly suggestive of a possible tuberculid and therefore a skin biopsy from a lesion was carried out.
In the meantime his physicians in the TB unit have been informed for the possible diagnoses and they had switched his regiment to moxifloxacin 400 mg/day in order to exclude the lichenoid drug reaction while they were waiting for the histology report of the skin lesion and the complete dermatological review.
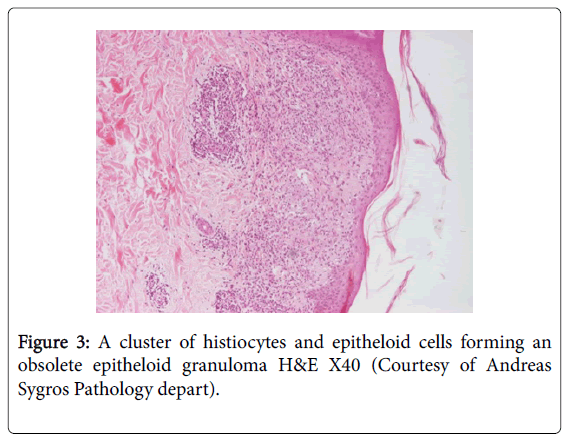
The histology revealed inflammatory lymphoid and epithelioid histiocytic infiltration of upper dermis and fibroblastic activity attributed to epithelioid granulomas (Figure 3). The correlation of histology with the clinical image led to the diagnosis of LS. The patient was already receiving an anti-TB regimen, which in this case is the treatment for LS as well. With the consolidation of the LS diagnosis and in liaison with his TB unit physicians, the patient continued his initial treatment regimen. Complete clearance of LS lesions was achieved gradually over a period of 60 days from the histopathological diagnosis.
Discussion
Tuberculids consist one type of CTB and they include conditions such as papulonecrotic tuberculid, LS, erythema induratum of Bazin, and erythema nodosum [5]. Tuberculids are thought to be due to hematogenous spread of bacilli in a person with a moderate or high degree of immunity against Mycobacterium tuberculosis [7,8]. Although the pathogenesis of LS is yet to be elucidated, most authors believe that the condition occurs in patients with medium to strong tuberculin sensitivity, who have undergone hematogenous spread of mycobacteria from an active internal tuberculous locus. This is followed by a type III hypersensitivity response from the host. The continuous formation of antigen-antibody complexes may lead a type IV hypersensitivity reaction, resulting in granuloma formation [6-9].
LS, also known as TB cutis lichenoides, most commonly affects children and adolescents with TB. LS appears to be the second most common form of CTB, according to recent reports, possibly because of increased incidence of all types of TB in general. Seven per cent of CTB patients were found to have LS in a prospective study in India [4]. Furthermore 11.4% of concurrent TB and HIV infection presented with LS in another Indian study [1]. LS could be a cutaneous sign for an underlying TB anywhere in the body. The most frequent extracutaneous involvement of TB in association with LS is lymphadenophathy (cervical, hilar, axillary, or mediastinal) but pulmonary TB is also reported. LS can also be associated with other types of CTB such as scrofuloderma, lupus vulgaris, and erythema induratum [4,6].
The lesions in LS usually present over the abdomen, chest, back and proximal parts of the limbs, as asymptomatic clusters of firm, typically perifollicular, skin-colored, erythematous or brown papules of 0.5-3 mm topped by a scale. Lesions may coalesce to form rough and discoid plaques [10,12].
Histopathology is diagnostic and demonstrates superficial granulomas around hair follicles and sweat ducts, with little or no caseation necrosis. Normally giant cells are absent and acid-fast bacilli are not found [3,4,6]. Tubercle bacilli are almost never seen in the biopsy specimen and they cannot be cultured [4,6,11]. A possible explanation is that they are present in a fragmented form or have been destroyed by immunological mechanisms [13]. The eruption is frequently associated with a strongly positive tuberculin reaction.
Diagnosis of LS is frequently delayed because of its rarity and resemblance to many other dermatological conditions [5]. The differential diagnosis may include lichen spinulosus, lichen nitidus, keratosis pilaris, pityriasis rubra pilaris, and lichenoid sarcoidosis [14]. Dermatologists should maintain heightened awareness of the clinical spectrum of CTB to halt this destructive and contagious disease early in its course [10].
The treatment of LS should follow the established guidelines for TB treatment as those of any other part of the body affected with TB. Following anti-TB treatment, the lesions usually clear within 4 to 12 weeks without scarring [6,10,11,15,16].
A cutaneous eruption as the first presentation of TB or as an accompanying condition of TB focus at other site of the body could be challenging for the primary care physician or the dermatologist. High index of suspicion is required in order to diagnose and treat quickly this condition, avoid complications and to stop disease spread. This case aims to raise awareness for the consideration of LS in the differential diagnosis of a widespread exanthem consisting of persistent, papular lesions, especially when the history of the patient suggests an evident or a possible TB infection. Patients with a suspected cutaneous eruption possibly associated with TB should be referred to a dermatologist for further diagnostic evaluation.
References
- Varshney A, Goyal T (2011) Incidence of various clinico-morphological variants of cutaneous tuberculosis and HIV concurrence: A study from the Indian subcontinent. Ann Saudi Med 31: 134-139.
- Singal A, Sonthalia S (2010) Cutaneous tuberculosis in children: The Indian perspective. Indian J Dermatol Venereol Leprol 76: 494-503.
- Joshi HS, Zacharia A, Warrier A (2014) Lichen scrofulosorum. BMJ Case Rep.
- Yates VM (2010) Mycobacterial Infections. In: Burns T, Breathnach S, Cox N, Griffith C, Rook's Textbook of Dermatology (8thedn) Massachusettes: Wiley-Blackwell.
- Santos JB, Figueiredo AR, Ferraz CE, Oliveira MH, Silva PG, et al. (2014) Cutaneous tuberculosis: epidemiologic, etiopathogenic and clinical aspects - part I. An Bras Dermatol 89: 219-228.
- Camacho D, Pielasinski U, Revelles JM, Górgolas M, Manzarbeitia F, et al. (2011) Lichen scrofulosorum mimicking lichen planus. Am J Dermatopathol 33: 186-191.
- Dogra N, Shah S, Dogra D (2008) Lichen scrofulosorum: an important marker of occult tuberculosis. Indian J Dermatol 53: 91-92.
- Dandale A, Gupta N, Dhurat R, Ghate S (2013) Unusual presentation of lichen scrofulosorum. Indian J Dermatol Venereol Leprol 79: 436-438.
- Beena KR, Ramesh V, Mukherjee A (2000) Lichen scrofulosorum - a series of eight cases. Dermatology 201: 272-274.
- Frankel A, Penrose C, Emer J (2009) Cutaneous tuberculosis: a practical case report and review for the dermatologist. J Clin Aesthet Dermatol 2: 19-27.
- Santos JB, Figueiredo AR, Ferraz CE, Oliveira MH, Silva PG, et al. (2014) Cutaneous tuberculosis: diagnosis, histopathology and treatment - Part II. An Bras Dermatol 89: 545-555.
- Kumar P, Jha OP, Mondal A (2014) Lichen scrofulosorum. Indian Pediatr 51: 335.
- Das JK, Sengupta S, Mitra S, Gangopadhyay AK (2010) Coexistence of papulonecrotic tuberculide with lichen scrofulosorum. Indian J Dermatol 55: 109-112.
- Dias MF, Bernardes Filho F, Quaresma MV, Nascimento LV, Nery JA, et al. (2014) Update on cutaneous tuberculosis. An Bras Dermatol 89: 925-938.
- Yadav P, Mendiratta V, Nikita, Chander R (2014) Concurrent lichen scrofulosorum and papulonecrotic tuberculid in a patient with tubercular lymphadenitis. Indian J Dermatol Venereol Leprol 80: 483.
- Puri N (2011) A clinical and histopathological profile of patients with cutaneous tuberculosis. Indian J Dermatol 56: 550-552.
Citation: Kostopoulos N, Tzanetakou V, Platsidaki E, Theologi V, Christofidou E, et. al (2017) Lichen Scrofulosorum in a Patient with Tuberculous Cervical Lymphadenopathy: A case report. Epidemiology (Sunnyvale) 7:316.
Copyright: © 2017 Kostopoulos N, et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4860
- [From(publication date): 0-2017 - Aug 16, 2025]
- Breakdown by view type
- HTML page views: 3938
- PDF downloads: 922