Case Report Open Access
Paraspinal and Foraminal Plexiform Neurofibromas: A Case Report from Radiological Standpoint
1Department of Radiology, Maharajha's Institute of Medical Sciences, Visakhapatnam, Andhra Pradesh, India
2Department of Radio-diagnosis, King George hospital, NTR University, Visakhapatnam, Andhra Pradesh, India
- *Corresponding Author:
- Padala RN
Department of Radiology, Maharajha's Institute of Medical Sciences
Visakhapatnam, Andhra Pradesh, India
Tel: 0091 8978005496
E-mail: nanda.padala@gmail.com
Received date: September 06, 2016; Accepted date: October 10, 2016; Published date: October 17, 2016
Citation: Padala RN, Malla UMR (2016) Paraspinal and Foraminal Plexiform Neurofibromas: A Case Report from Radiological Standpoint. OMICS J Radiol 5:235. doi:10.4172/2167-7964.1000235
Copyright: © 2016 Padala RN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
There are two types of Neurofibromatosis (NF), NF type 1 and NF type 2. NF 1 is an inherited autosomal dominant disease involving skin and peripheral nerves. NF 2 is a rare autosomal dominant neurocutaneous disorder manifesting as the development of multiple CNS tumours. The disease predominantly affects men, with M:F ratio of 3:1. The clinical manifestations do vary according to the region of involvement. All cases of NF 1 should undergo further investigation, due to possible development of complications as the nerves supply the vital organs. Surgical resection and biopsy should be avoided and such patients should undergo clinical and radiological follow-up at subsequent intervals. This case reveals the radiological perspective of imaging, preliminary diagnosis, follow-up and palliative care of symptomatic patients, with plexiform neurofibromas.
Keywords
Neurofibromatosis (NF); Neurofibromatosis type 1(NF1); Neurofibromatosis type 2 (NF2); Von Recklinghausen disease; Plexiform neurofibromas (PNF)
Introduction
Neurofibromatosis 1 (NF1) is described by Friedrich Daniel VonRecklinghausen in the year 1882, is an inherited autosomal dominant disease involving skin and peripheral nerves. The incidence of NF 1 is approximately 1 in 4,000 people [1,2]. Aberration in long arm of chromosome 17 is the cause of NF1.The genetic disorder is identified by a combination of clinical features like Café au lait spots, lisch nodules, neurofibromas, gliomas of the optic pathway and bone dysplasia. Spinal involvement of PNF was classified for simplicity into types depending on their anatomical location as paraspinal, intramedullary, foraminal [3]. PNF are benign masses of peripheral nerve sheath and may sometimes undergo malignant transformation, which needs to be distinguished from malignant peripheral nerve sheath tumor.
At least two of the following criteria should be fulfilled to make the diagnosis of NF-1 clinically [4].
1. Prepubescent patients: Five or more cafe-au-lait spots (or) macules each measuring greater than 5 mm in long axis; postpubescent patients: six (or) more cafe-au-lait spots each measuring greater than 15 mm in long axis.
2. Two or more than two neurofibromas, (or) one plexiform neurofibroma.
3. Inguinal (or) axillary freckling
4. Glioma of optic tract.
5. Two (or) more Lisch’s nodules
6. A distinguishing osseous lesion (pseudoarthrosis of the tibia or dysplasia of sphenoid wing)
7. A person (parent, sibling) diagnosed with NF-1.
This case reveals the radiological significance of imaging, preliminary diagnosis, follow-up and palliative care of symptomatic patients with plexiform neurofibromas in NF1.
Case report
A 33-year young male patient presented with a complaint of lumps in the right lower abdomen and lower back since one month. There were no constitutional symptoms.
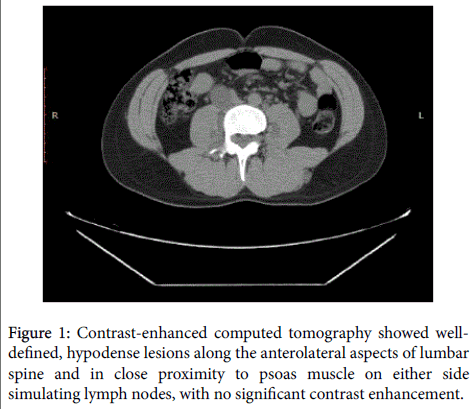
Physical examination of patients revealed cafe-au-lait spots, skin, subcutaneous neurofibromas and lisch nodules. Ultrasonography revealed a hypoechoic paraspinal mass lesion measuring 9.6 cm in the right iliac region. Contrast-enhanced computed tomography showed well-defined, hypodense lesions along the anterolateral aspects of lumbar spine and in close proximity to psoas muscle on either side simulating lymph nodes, with no significant contrast enhancement (Figure 1).
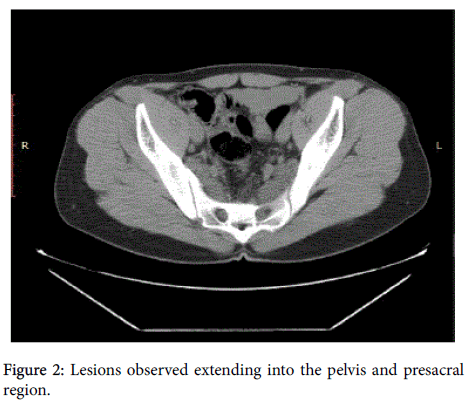
Paraspinal masses tended to be long and cylindrical with a measurement of 10.0×3.0 cm. In addition to the paraspinal lesions, few more similar type lesions were also observed extending into the pelvis and presacral region (Figure 2).
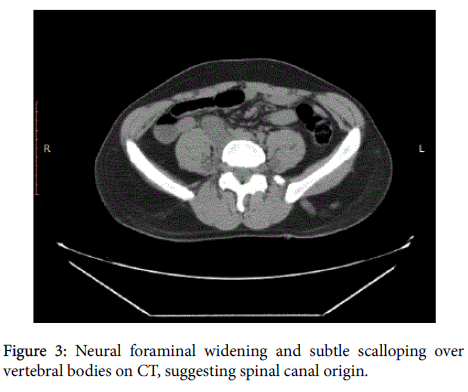
There is evidence of neural foraminal widening and subtle scalloping over vertebral bodies on CT, suggesting spinal canal origin (Figure 3).
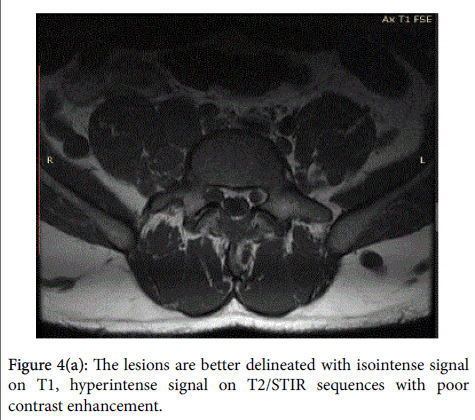
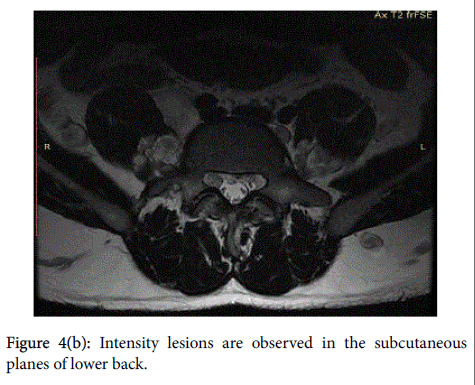
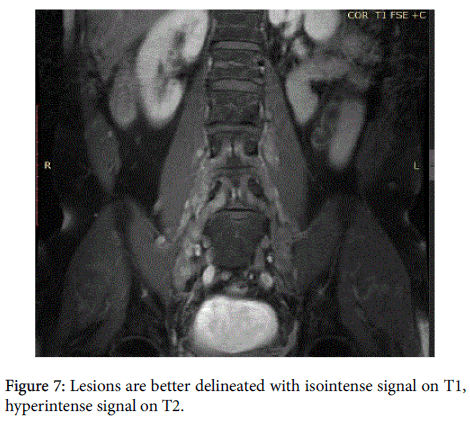
Contrast-Enhanced Magnetic Resonance Imaging (CEMRI) of the brain, whole abdomen and whole spine was accomplished for investigation. On CEMRI the lesions described in CT are better delineated with isointense signal on T1, hyperintense signal on T2/ STIR sequences with poor contrast enhancement (Figures 4(a) and 4(b) and 7).
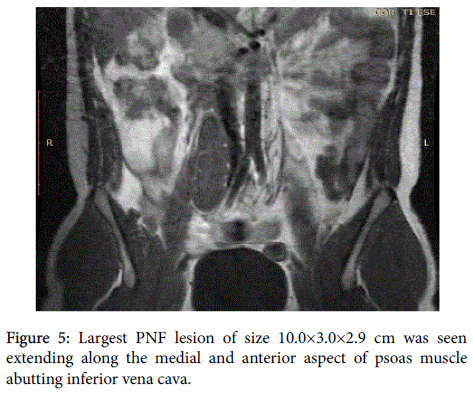
The largest PNF lesion of size 10.0×3.0×2.9 cm was seen extending along the medial and anterior aspect of psoas muscle abutting inferior vena cava (Figure 5).
Some of them were of dumbbell shape which could be traced into the neural foramina and communicating with spinal canal was identified with difficulty. Based on imaging findings spinal plexiform neurofibromas in right lumbar region and multiple neurofibromas of lumbosacral nerves was made. Biopsy was not advised due to fear of development of neurological deficits. Similar intensity lesions are observed in the subcutaneous planes of lower back figure 4(b). Degenerative disc changes at L4-5 level was an incidental finding. In addition all the hematological and biochemical parameters were within normal limits.
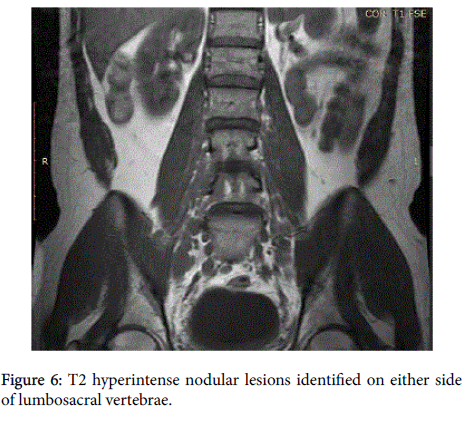
In addition, multiple poorly enhancing T2 hyperintense nodular lesions were also identified on either side of lumbosacral vertebrae (Figure 6).
On regular follow-up at subsequent intervals, except for feeling of lumps, there was no development of pain or neurological deficits. The patient was apprised to disclose symptoms particularly in relation to pain manifestation and sudden increase in size of the lumps, as they may suggest the possibility of malignant transformation and at this stage biopsy is mandatory.
Discussion
PNF in paraspinal and pelvic regions are often less common [5]. They are common in children and young adults with male to female ratio of 3:1. In cases of pelvic location, there is a risk of malignant transformation and regular clinical and radiological follow-up is advisable [6,7]. Clinical signs of malignant transformation include the onset of persistent pain and development of neurological deficits/ sudden increase in size of the lesion. MRI is the imaging modality of choice for identification of different types of neurofibromas and their malignant transformation [7-10]. The contrast-enhanced MRI and fat saturation techniques are helpful to distinguish between malignant and benign masses by asymmetrical growth and heterogeneous signal intensity suggestive of malignancy. The heterogeneous pattern may be due to hemorrhage, necrosis and inhomogeneous contrast uptake [7,8]. In relation to muscle signal the PNFs show iso to slightly hyperintense signal on T1WI and hyperintense signal on T2WI. Usually the CEMRI findings confirm the diagnosis of PNF thus makes biopsy unnecessary [10]. Biopsy is avoided in cases of PNF due to fear of development of neurological deficit, as functional axons also traverse within. Performing surgery is a complex procedure due to extension of PNF into unaccessible locations and innervations of nerves to vital structures. Surgery is reserved only in suspected cases of malignant transformation and the benefits of surgical resection outways the tumour recurrence [6].In addition, these lesions are not much sensitive for radiotherapy. In our case the patient presented with right iliac fossa lump which on investigation turned out as a rare pelvic PNF. So, pelvic PNF should be included in the differential diagnosis of pelvic soft tissue masses because they may mimic enlarged retroperitoneal lymph nodes, psoas abscesses, ovarian tumors, metastases or soft tissue sarcomas. Treatment of NF1 depends on the extent of disease, the symptoms and suspicion of malignant degeneration or increase in size of the mass [11]. The aim of the case report is to highlight the necessity of clinical/radiological follow-up, palliative treatment and avoiding biopsy (except for malignant transformation) in cases of plexiform neurofibromas considering development of neurological deficits and to keep extreme caution against malignant transformation.
References
- Stemmer-Rachamimov AO, Louis DN, Nielsen GP, Antonescu CR, Borowsky, et al.(2004) Comparative pathology of nerve sheath tumors in mouse models and humans. Cancer Res 64: 3718-3724.
- Wise JB, Cryer JE, Belasco JB, Jacobs I, Elden L (2005) Management of head and neck plexiform neurofibromas in pediatric patients with neurofibromatosis type 1. Arch Otolaryngol Head Neck Surg 131: 712-718.
- Mauda-Havakuk M, Shofty B, Ben-Sira L, Constantini S (2015) Spinal and para-spinal plexiform neurofibromas in NF1 patients, a clinical-radiological correlation study.
- National Institutes of Health Consensus Development Conference (1988) Neurofibromatosis.Arch Neurol Chicago 45: 575.
- Cabrera Castillo PM, Alonso y Gregorio S, Cansino Alcaide JR, Aguilera Basan A, Peña Barthel JJDL (2006) Neurofibroma de la vejiga: caso clínico y revisión de la literatura. Arch Esp Urol 59:899-901.
- Nunes TF, Costa RP, Navarro FC (2005) Von Recklinghausen’s diseasewith urogenital manifestation. IntBraz J Urol 31: 153-154.
- Ros PR, Eshaghi N (1991) Plexiformneurofibroma of the pelvis: CT and MRI findings Magn Reson Imaging 9: 463-465.
- Mautner VF, Friedrich RE, Von Deimling A, Hagel C, Korf B, et al. (2003) Malignant peripheral nerve sheath tumours in neurofibromatosis type 1: MRI supports the diagnosis of malignant plexiform neurofibroma. Neuroradiology 45: 618-625.
- Jana M, Gamanagatti S, Kumar R, Aggarwala S (2011) Pelvic neurofibroma arising from prostate in a case of neurofibromatosis-1. Indian J Urol 27: 415.
- Cançado DD, Leijoto CC, Carvalho CES, Bahia PRV (2005) Neurofibromatose plexiforme retroperitoneal e pélvica: aspectos na tomografia computadorizada e ressonância magnética-relato de caso e revisão da literatura. Radiol Bras 38: 239-242.
- Wilkinson LM, Manson D, Smith CR (2004) Best Cases from the AFIP: Plexiform Neurofibroma of the Bladder 1. Radiographics 24(suppl_1): S237-S242.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 12056
- [From(publication date):
October-2016 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 11155
- PDF downloads : 901