The Development of Breast Cancer Screening in Qatar (January 2008-April 2015)
Received: 29-Feb-2016 / Accepted Date: 03-May-2016 / Published Date: 10-May-2016 DOI: 10.4172/2471-9919.1000107
Abstract
Qatar has one of the highest age-adjusted breast cancer incidences in the Arab world. Although this is much lower than the incidence in the West. Breast cancer incidence in Qatar was 45 per 100,000 in 2003-2007. 53 per 100,000 in 2008-2011. These higher incidence rates in Qatar are mainly due to the growing population. The prevalent age group, between both Qatari and non-Qatari patients, was 40-50 years old. This suggests that the age-specific incidence of breast cancer in Qatari women is shifting more to a pattern usually not seen in Western nations where median age at diagnosis is 61 years of age, moreover the diagnosis is often at advanced stages of breast cancer. These factors, together with reconfirmed evidence of mortality benefit from breast cancer screening trials, led to establishment the first hospital based mammographic breast cancer screening program in Qatar. It uses a distributed model of mammography service. The program accepts eligible asymptomatic women at age between 40-69 years and was launched in 2008. It adopted international standards of breast screening practice and breast cancer detection.
Keywords: Breast cancer; Controlled trials; Radiology; Breast imaging; Carcinoma; Screening program; Breast cancer; Mammography; High risk women
41793Abbreviations
HMC: Hamad Medical Corporation; OPD: Outpatient Department; RCTs: Randomized Controlled Trials; FNA: Fine Needle Aspirate; PPV: Positive Predictive Value
Introduction
Breast cancer continues to be the most common form of cancer that affects women and the second leading cause of cancer death, counting worldwide about 1.38 million of new cases and about 458,000 estimated deaths in 2008. Incidence rates are higher in developed countries (greater than 80 per 100,000) than in most of the developing countries (less than 40 per 100,000). On the other hand, the range of mortality rates in developed regions is much less (approximately 6–19 per 100,000) because of the more favorable survival of breast cancer. Observed improvements in breast cancer survival rates in more developed regions have been attributed to the introduction of population-based screening using mammography and the systemic use of adjuvant therapies and evolution of surgical management. According to 2004 studies the Arab population has an estimated size of 301,227,000 people, living in 22 countries cross North Africa and west Asia, including the Middle East. Breast cancer is the most common malignant disease in women from Arab populations, comprising 14-42% of all tumors,
Data from the Gulf Center for Cancer Registration show that Bahrain had 53.4 cases of breast cancer per 100 000 women per year, followed by Qatar (48.2 per 100 000 per year), Kuwait (46.6 per 100 000 per year), United Arab Emirates (22.8 per 100 000 per year), Oman (17.5 per 100 000 per year), and Saudi Arabia (14.8 per 100 000 per year). From 2000 to 2010 the population of Qatar has increased from 744,483 to 1,696,563 and, at the same time the incidence rates of breast cancer has increased from 45 per 100,000 in 2003-2007 to 56 per 100,000 in 2008-2011.
The incidence rate of breast cancer in Qatar is one of the highest (Bahrain, Kwuit, Qatar) among the Arab countries Figure 1 (CI5 X). Qatari patients accounted for 32% of all the diagnosed breast cancers in female Qatar, while non-Qatari patients (other Arab, Indian, Filipino, Nepali, Pakistani, Sri Lankan and others) represented the remaining 68%. The prevalent age group, between both Qatari and non-Qatari patients, was 40-50 years old (36% of all affected women) (Table 1).
| Bahran | Oman | Kuwait | Qatar | KSA | Egypt | Algeria | Libya | Tunisia | |
|---|---|---|---|---|---|---|---|---|---|
| 2003-2007 | 56 | - | 50.1 | 45.7 | 21.1 | 45.4 | 28.9 | 22.9 | 30.9 |
| 1998-2002 | 46.8 | 14.6 | 41.3 | - | - | 42.5 | 18.8 | - | 23.4 |
| 1993-1997 | - | 12.7 | 32 | - | - | - | 21.3 | - | - |
Table 1: ASR per 100,000 Breast Cancer in Arabian Countries C15.
The average age at presentation of breast cancer in Arab women is a decade earlier than in European and US individuals. In Arab populations, the median age at diagnosis is about 48 years, and about two-thirds of women with breast cancer are younger than 50 years. This age pattern differs from that reported in patients from the USA and Europe, where the median age at diagnosis is around 63 years and only 25–30% of patients are younger than 50 years. However, Arab populations generally have a younger median age than European and US residents. Furthermore, elderly Arab women are less likely to obtain mammograms than are their younger counterparts.
Screening tests represent useful tools to identify individuals affected by a specific disease within an asymptomatic population, at the time when treatment could result in improvement of prognosis. Detecting and treating breast cancer earlier in its natural history results in a reduction in mortality rate for the disease [1]. To date, several population-based randomized controlled trials (RCTs) of mammography screening provided strong support for the efficacy of breast cancer screening. Particularly, mammography represents the only test proven to reduce breast cancer-related mortality, remaining the sole imaging test recommended for breast cancer screening [2]. In the last decade, different interpretations of the results from the RCTs and observational studies have led to several screening guidelines according to age, personal history and familial risk. However, despite the indisputable benefits of introducing breast cancer screening programs, contentious debates over the potential harms from mammographic screening are emerging [3]. The potential harmful effects of mammographic screening are related to ‘‘over-diagnosis’’ and “over-treatment” of tumours that would not have progressed to cause symptomatic disease, the lack of specificity of mammography leading to recall for further tests for many healthy women, and the lead time bias for which the screening may detect some very slow-growing tumours, bringing forward the time of diagnosis without any effect on the overall survival of patients.
Mammography screening programs for general population vary across countries, with different recommendations related to the age of starting and the frequency of screening. Data in literature suggest that screening should be proposed at least every two years from 50 to 74 years of age. For women younger than 49 years, the pathological personal history and familial cancer risk should be taken into consideration. In women older than 75 years, information about the effectiveness of screening is lacking thus the decision should be individualized, considering patients’ life expectancy and goals of care. For women with a lifetime risk for breast cancer of more than 20% or who are BRCA mutation carriers, screening should begin before 30 years [4]. However, ultrasound represents the tool of reference for the screening in this category, since it is more sensitive than mammography in young breasts. Moreover, mammography in this young age group showed no evidence that the benefits exceed the risks. Screening with magnetic resonance imaging may be offered to high-risk women inside approved and audited services or as part of ethically approved research trials, since its impact on breast cancer mortality is still uncertain. Finally, breast self-examination is not recommended because it did not show to improve mortality [5].
Materials and Methods
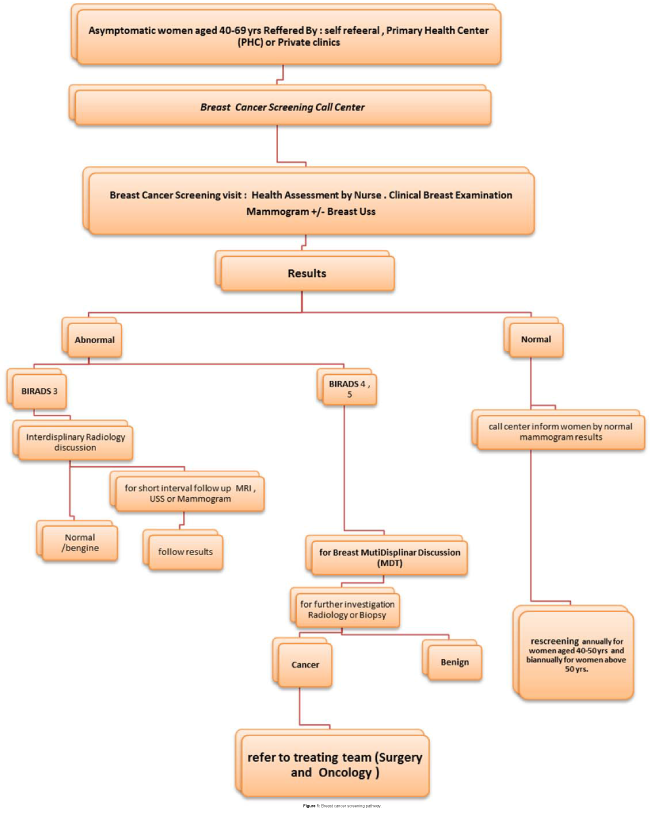
A retrospective study was conducted to describe the breast cancer screening program in Qatar and to overview the detection rates, positive predictive values and sensitivity and specificity of mammogram. Women satisfaction. The breast cancer screening program under Hamad Medical Corporation in Qatar was started on April 2008, accept eligible women from all areas including the provinces of Doha, Dukhan and Wakra for breast screening. The criteria for eligible to be accepted for the screening program as following: Qatari and other nationalities resident in state of Qatar, asymptomatic, All women at age between 40- 69 years old in the beginning of the screening program since we were providing the first breast cancer screening in our local community, we included some women of ages below 45 years with family history of breast cancer were accepted. Women are referred to screening clinic from PHCs, privet sector and by self-registration through the breast screening calling centre Frequency of screening biannually for women above 50 years and annually for women below 50 years due to breast densities. In the Breast Screening visit all women were assessed by: the breast cancer risk of each patient will be assessed by the nurses by using an international model called the “Risk Calculator Gail score (http://www.cancer.gov/bcrisktool/Default.aspx). Then breast clinical examination by physician followed by a screening mammographic examination in the same day Conventional 2 - view film/screen mammograms were provided and reviewed by radiologist. Further complementary breast USS for women with increased breast tissue densities or detection of any suspicious lesion by the mammogram. Mammograms were scored on a 5-point scale using the American College of Radiology Breast Imaging-Reporting and Data System (BI-RADS). The categories are shown in Table 2. Based on mammography results, if a woman needs further investigation where the abnormality is assessed by a multidisciplinary team. And according to the MDT recommendations women recalled to further assessment.
| Category | Diagnosis | Number of Criteria |
|---|---|---|
| 0 | Incomplete | mammogram or ultrasound didn't give the radiologist enough information to make a clear diagnosis; follow-up imaging is necessary |
| 1 | Negative | There is nothing to comment on; routine screening recommended |
| 2 | Benign | A definite benign finding; routine screening recommended |
| 3 | Probably Benign | Findings that have a high probability of being benign (>98%); six-month short interval follow-up |
| 4 | Suspicious Abnormality | Not characteristic of breast cancer, but reasonable probability of being malignant (3 to 94%); biopsy should be considered |
| 5 | Highly Suspicious of Malignancy | Lesion that has a high probability of being malignant (>=95%); take appropriate action |
| 6 | Known Biopsy Proven Malignancy | Lesions known to be malignant that are being imaged prior to definitive treatment; assure that treatment is completed |
Table 2: Touch the movements of care.
Women at increased risk of developing breast cancer by increase familial incidence of breast cancer at younger age group should follow specific recommendations for surveillance, screening, management and prevention. High risk breast cancer cases referred to high risk breast and ovarian cancer clinic for farther evaluation and assessment by genetic counsellor for genetic scoring assessment for genetic testing and to discus in MDT meeting depends on breast ovarian cancer high risk guide lines in Qatar.
Results
The prevalent age group of breast cancer in Qatar population 44- 48 years, much less than the median age in Western countries where it is about 61. The only inclusion criterion for the current study was being an asymptomatic woman of age ≥ 40 years; however, since we were providing the first breast cancer screening in our local community, we included some women with symptoms.
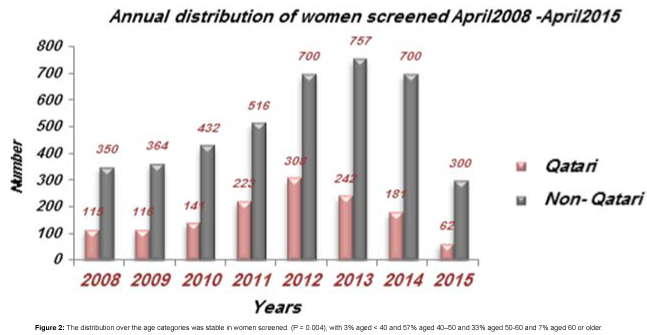
% change has been calculated using unrounded figures or use the annual percent change (APC) is often used to measure trends in disease and mortality rates, and a common estimator of linear model on the log of the age-standardized rates. Under the assumption of linearity on the log scale, But for this data uses this formula: ((y2-y1)/y1) * 100 (Figure 2).
From April 2008 to April 2015, in the Breast Cancer Screening Program, 5507 accesses have been registered with an increasing participation, year by year. Approximately, 465 women (115 Qatari and 350 non-Qatari) have been screened in 2008, 480 women (116 Qatari and 364 non-Qatari) in 2009, 573 women (141 Qatari and 432 non- Qatari) in 2010, 738 women (223 Qatari and 515 non-Qatari) in 2011 and 1008 women (308 Qatari and 700 non-Qatari) in 2012, 242 Qatri 757 non Qatri and on 2015 up to April 201562 Qatari and 300 non Qatari (Table 3).
| Number 2008-2013 initial and subsequent women | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Population | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Apr-15 | Total | % |
| Total number of women screened | 465 | 480 | 573 | 739 | 1008 | 999 | 881 | 362 | 5507 | |
| Qatari | 115 | 116 | 141 | 223 | 308 | 242 | 181 | 62 | 1388 | 25.3 |
| Non- Qatari | 350 | 364 | 432 | 516 | 700 | 757 | 700 | 300 | 4119 | 74.7 |
% change has been calculated using unrounded figures or use The annual percent change (APC) is often used to measure trends in disease and mortality rates, and a common estimator of linear model on the log of the age-standardized rates. Under the assumption of linearity on the log scale,But for this data uses this formula: ((y2 - y1) / y1)*100.
Table 3: Number 2008-2013 initial and subsequent women.
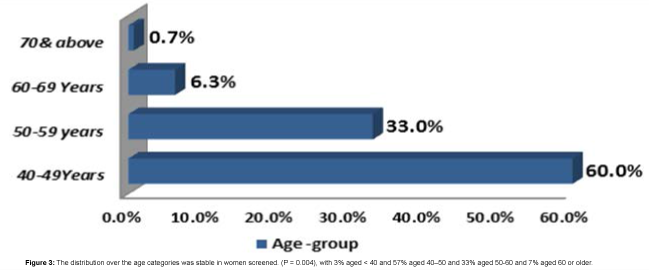
3331 accesses of women of 40-49 years (increasing from 332 in 2008 to 545 in 2014), 1805 of women of 50-59 years (increasing from 112 in 2008 to 282in 2014), 331 of women of 60-69 years (increasing from 19 in 2008 to 96 in 2013) and, 19 of women over 70 years of age (increasing from 2 in 2008 to 12 in 2013) (Figure 3).
During these Seven years of screening, 4072 mammograms, 2615 complementary ultrasounds and 205 MRI have been performed (Table 4).
| Radiology Test | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Apr-15 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Mamography | 421 | 440 | 540 | 706 | 977 | 988 | 871 | 343 | 4072 |
| U/S | 221 | 271 | 306 | 539 | 611 | 667 | 618 | 288 | 2615 |
| MRI | 8 | 33 | 27 | 23 | 53 | 61 | 40 | 9 | 205 |
FC=heart rate; FR=respiratory rate; PAS=Systolic blood pressure; PAD=diastolic blood pressure; N. Min=minimum number; N. Max=maximum number
Table 4: Radiology Test.
Diology
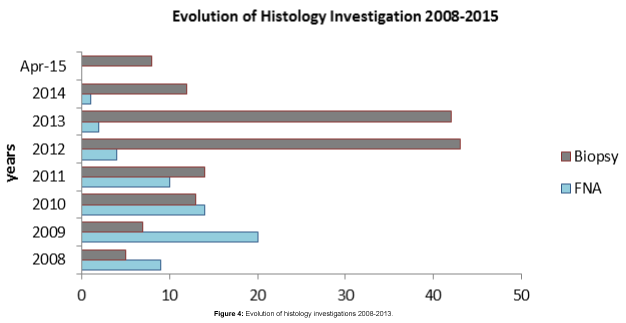
Of all mammograms performed Conventional 2-view film/screen mammograms were provided and reviewed by radiologists. Further complementary breast Uss were performed when judged to be necessary [san Antonio 2014]. Mammograms were scored on a 5-point scale using the American College of Radiology Breast Imaging- Reporting and Data System (BI-RADS). 9 were classified as incomplete assessments (BIRAD 0), 539 resulted (BIRAD 1), 3218 resulted benign findings (BIRAD 2), 1088 resulted probably benign (BIRAD 3), 215 resulted suspicious abnormalities (BIRAD 4), 58 resulted highly suggestive of malignancy (BIRAD 5) and 82 were unknown or not specific, the rate of BIRAD 4-5 in 2008 was 2.6%, in 2009 was 5.7%, in 2010 was 6.6%, in 2011 was 2.9%. In 2012 was 6.1%. 60 cases needed a fine needle aspirate (FNA) and 144 patients underwent a core-biopsy or stereotactic biopsy. Of these recalls, 51 resulted true-positive tests for malignancy (Table 5).
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Apr-15 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| FNA | 9 | 20 | 14 | 10 | 4 | 2 | 1 | 0 | 60 |
| Biopsies | 5 | 7 | 13 | 14 | 43 | 42 | 12 | 8 | 144 |
Table 5: Tests for malignancy.
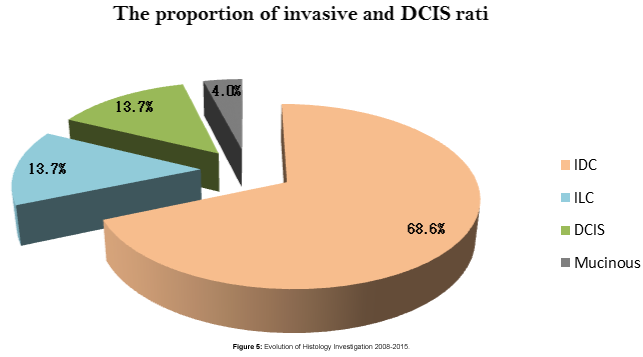
Out of 144 core- biopsied cases 51 were positive of breast carcinomas, (35) invasive ductal carcinoma, DCIS (7), ILC (7), mucinous ca (2) in age group between (42-51). Thus, cancer detection rate has been 10.07 per 1000 examinations (Figure 4).
Mammographic BIRAD evaluation for breast cancer positive cases BIRADS 5 in (13) case, BIRADS 4 in (25) cases BIRADS 3 IN (7) and BIRADS 2 in 1 case only, 26 cases recall for MRI evaluation after performing Mammographic screening out of these 13 came BIRADS 5. 8 BIRADS 4,2 BIRADS 3 and only one BIRADS 2, on Histological review of the breast cancer detected in breast cancer screening most of the histopathological type ( IDC ) in 44 of carcinomas detected, on immune - histochemistry staining ER, PR positive in 34, ER PR negative in (18), Her 2 positive in ( 40) and Her2 –ve in (11), tumour grad 2/3 in most of the detected cases, on staging stage 0 in (7), stage 1 in (9) stage 2 in (16) stage 3 in (7) stage 4 in (1) case. in correlation from our date the mammogram sensitivity reach 89% and specificity reach 98%, the specificity for breast MRI ranged from 59.4% to 95% and sensitivity of 89%.
On correlation with risk factors as age of menarche the mean age of menarche in the detected case (12) age at first pregnancy 28 years and 38 of these case used hormonal treatment in their life in form of OCP, progesterone or use ovulation induction protocols for infertility treatment.18 out of 51 of breast cancer detected cases have positive clinical finding as small palpable lump or palpable axillary lymph node most of them not aware by these findings (symptoms) (Figure 5).
In women aged 45-60 cancer detected cases, the proportion of invasive and micro-invasivecancers was 84% in prevalent screens, this compares with insitu cancer13.7% in the detected cases
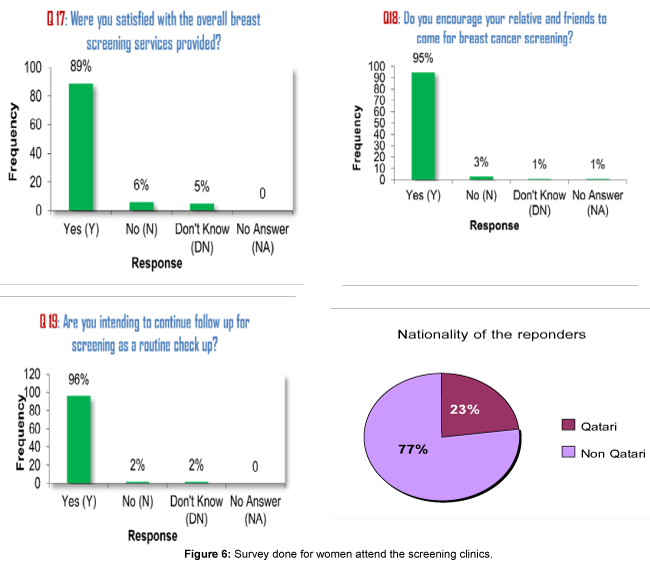
From April 2008 to April 2015, in women aged 40-69, the quality of screening has significantly improved over time. Firstly, the positive predictive value (PPV) has gradually decreased from 46% to 20%. Moreover, sensitivity value has improved from 51% in 2008 to 70% in 2012 as well as the specificity for mammography ranged from 80.2% to 95.5% public acceptance and satisfaction assessed by regular survey for women screened in our screening clinics showed high satisfaction with our services noticed in survey done for women attend the screening clinics (Figure 6).
Discussion
The aim of this study is to describe the results of the first breast cancer screening program in Qatar started from April 2008 up toApril 2015, to overview of the acceptance level, parcipitation rate, sensitevity of mammogram and the incidance of breast cancer in corrolation with age group. The main objective of this preliminary analysis was to assess the prevalence of breast cancer phenotypes in Qatar population. Additional objectives were to evaluate the association of a diagnosis of breast cancer with the BI-RADS score, the strong correlation between mammographic findings and breast cancer confirmation is an encouraging finding for our screening program. Mammography screening programs for general population vary across countries, with different recommendations related to the age of starting and the frequency of screening. Data in literature suggest that screening should be proposed at least every two years from 50 to 70 years of age. For women younger than 49 years, the pathological personal history, breast mammographic density and familial cancer risk should be taken into consideration as their risk of breast cancer may higher. In women older than 75 years, information about the effectiveness of screening is lacking thus the decision should be individualized, considering patients’ life expectancy and goals of care. For women with a lifetime risk for breast cancer of more than 25 percent or who are BRCA mutation carriers, screening should begin before 30 years these cases and high risk families refer to high risk breast ovarian clinic in NCCCR [6]. Moreover, mammography in this young age group showed no evidence that the benefits exceed the risks with the complementary Screening with magnetic resonance imaging may be offered to high-risk women inside approved and audited services or as part of high risk surveillance, since its impact on breast cancer mortality is still uncertain. Finally, breast self-examination is not recommended because it did not show to improve mortality and may increase anxiety [7]. In the year 2008, for the first time, a mammographic screening program was launched in Qatar for women aged 40 and older. The screening program enrolled self-referral women or women with a physician’s referral from all parts of Qatar, and in the first 5 years of work it has registered 5507 accesses. From 2008 to 2015, in women aged 40-670, the quality of screening has significantly improved over 5507 accesses have been registered with an increasing participation, year by year. Firstly, the positive predictive value has gradually decreased from 46% to 20%. Moreover, sensitivity value has improved from 51% in 2008 to 70% in 2012 as well as specificity value that has increased from 77% in 2008 to 83% in 2012. Out of 144 send for breast biopsies 51 appear positive of malignency, the age group of breast cancer detected cases from screening program (43-52 years), DCIS I (7), IDC (35) LCIS (7) moucinous ca (2) the diagnosic interval of breast cancer is the time from the initial screening mammogram to the time to be seen by treating physician was within 14 days for 32 of the BC detected cases and within 14-28 days for other BC detected cases.
Increase of the incidence of breast cancer and decrease in breast cancer mortility can be achieved with major efforts in screening and early detection as a high sensitivity of the mammogram in early detection of DCIS and IDC cases apart of LCIS witch not highly detected in mammographic imaging and LCIS has law incidence. Although several awareness campaigns have been undertaken in raising the awareness of early detection of breast cancer, on breast cancer screening program data analysis showed increase number of participants during and after each October national awareness month.
Conclusion
Public acceptance of the breast cancer screening program in Qatar gradually increased and women highly satisfied about the services. Detection rate reach 0.95% incidence rate higher in age group (43-52) years. invasive detection rates and stage of disease on detection were higher compare and advanced than the western counters, this indicate either aggressive behavior of the disease or women come forward to screening without knowing that they are symptomatic, in this part of the world. We have a unique population of multinationals that merits tailored screening tools and intensify the public awareness and early detection screening program. Finally this means that mammogram with complement breast USS is an effective tool in detecting breast cancer in our patient population, which is generally young and may have denser breast tissue compared to elderly women. Long-term follow-up is required to assess the actual benefit; however, Our main conclusion was the direct need for health education and constant awareness programs to raise up the awareness by breast cancer incidance, risk factors of brest cancer and brest cancer early detectrion.
Acknowledgement
The authors gratefully acknowledge breast cancer screening team for their valuable contributions in Data collection and data entry. We also appreciate their efforts in succession the screening program.
References
- Islam SR, Aziz SM (2012) Mammography is the most effective method of breast cancer screening. Mymensingh Med J 21: 366-371.
- Nelson HD (2011) GøtzschePC,Cochrane Database of Systematic Reviews 2009.Taba ´r L,Radiology 260:658–663
- Warner E (2011) Clinical practice. Breast-cancer screening. N Engl J Med 365: 1025-1032.
- Cardoso F, Loibl S, Pagani O, Graziottin A, Panizza P, et al. (2012) The European Society of Breast Cancer Specialists recommendations for the management of young women with breast cancer. Eur J Cancer 48: 3355-3377.
- Fergus J, Couch FJ, Michelle L, Deshano BS, et al. BRCA1 Mutations in women attending clinics that evaluate the risk of breast cancer. The New England Journal of Medicine 336; 1409-1415.
- Chouchane L, Boussen H, Sastry KS (2013) Breast cancer in Arab populations: molecular characteristics and disease management implications. Lancet Oncol 14: e417-424.
Citation: Al-Bader SB, Bugrein H, Elmistiri M, Alassam R (2016) The Development of Breast Cancer Screening in Qatar (January 2008 – April 2015). Evid Based Med Pract 1: 107. DOI: 10.4172/2471-9919.1000107
Copyright: ©2016 Al-Bader SB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5399
- [From(publication date): 0-2016 - Jul 13, 2025]
- Breakdown by view type
- HTML page views: 4424
- PDF downloads: 975