Research Article Open Access
The Effect of Mouth Care with Aloe Vera Solution on Mucositis: Treatment in Patients with Chronic Obstructive Pulmonary Disease (Copd)
Seval Agaçdiken1* and Magfiret Kara2
1Fundamentals of Nursing Department, Samsun School of Health, Ondokuz Mayis University, 55250, Samsun, Turkey
2Fundamentals of Nursing Department, Faculty of Health Sciences, 25240, Erzurum, Turkey
- *Corresponding Author:
- Seval Agaçdiken
Ondokuz Mayis University
Samsun School of Health
Department of Nursing
55250, Samsun, Turkey
Tel: +90 442 231 23 15
E-mail: seval_mavice@hotmail.com
Received Date: September 26, 2014; Accepted Date: November 16, 2014; Published Date: November 21, 2014
Citation: Agaçdiken S, Kara M (2014) The Effect of Mouth Care with Aloe Vera Solution on Mucositis: Treatment in Patients with Chronic Obstructive Pulmonary Disease (Copd). J Oral Hyg Health 2:168. doi:10.4172/2332-0702.1000168
Copyright: ©2014 Agaçdiken S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Study Background:The responsibility of nurses is to provide and maintain oral health in healthy/unhealthy individuals, to help those without this habit to achieve oral health habits, to prevent the complications caused by drug treatment and to provide patient counseling services and education. The aim of this research was to evaluate the effect(s) of regular oral care which made use of a solution that contained aloe vera in the treatment of patients with COPD suffering from mucositis.
Methods: This study is an experimental research consisting of an experiment and a control group. The study was planned as an experimental research and was conducted between March and July, 2009. The research was conducted in a tertiary, education and research hospital in Erzurum, Turkey. Patients in the research group (experimental group) were provided with regular oral care with a solution of 0.5 % “aloe vera” for 15 days, three times a day (3x1). Oral changes of both groups were examined by the researcher using visual inspection, and oral mucositis scores were registered in the “Researcher’s Mucositis Index” on the 1st day (Day 1) and 15th day (Day 15). The patients in both groups were asked to write their complaints in the “Patient Complaint Index” (PCI) on a daily basis. Percentages, chi-square, mean, Wilcoxon and Mann-Whitney U tests were used to evaluate the data.
Results and Conclusion: On completion of the research both the complaint scores and oral mucositis levels decreased notably in the experimental group as a result of the oral care which made use of the aloe vera solution.
Keywords
Oral mucositis; Oral care; Aloe vera; Nursing
Introduction
The oral cavity is a central part of the body for most people [1]. Verbal and nonverbal communication occurs through the oral cavity. Food intake and functions that are crucial for living also depend indirectly on the adequate functioning of the oral cavity. The anatomy of the oral cavity also affects the images we have of people [1].
In a study of elder people, MacEntee et al. stated that oral health comprised three independent components: (a) comfort: including pain and nutrition; (b) oral hygiene: emphasizing the significance of a clean mouth from individual and social perspectives; (c) general health: reflecting the interaction between the mouth and all other parts of the body [2].
Evidence shows that oral health has a significantly direct impact on systemic heal [1] and thus, to meet the oral care needs of patients, we should evaluate oral care products. Scientific findings have shown that oral health has an effect on general health and the development of systemic diseases [3].
There are a number of factors that facilitate common oral problems [4], including:
• Drugs
- Cytotoxic drugs
- Corticosteroids
- Antibiotics
- Antihistamines
- Diuretics
- Morphines
• Treatments
• Psychological and physical health problems
Oral care is accepted as one of the basic elements of nursing care by many researchers [3,4]. Oral care is a nursing initiative that should be taken into consideration in order to provide for a patient’s comfort [4]. In addition, oral care becomes an essential initiative to ensure a patient’s comfort in cases of chronic diseases such as COPD, which affects general health. Oral mucositis formation that occurs in response to inhaled corticosteroid treatment particularly in COPD patients - causes oral complications such as oral dryness, candidiasis and dental changes (these are the most common effects) [5,6]. Corticosteroids constitute the most commonly used drug group within the treatment protocols of COPD patients [7,8] . The effects of corticosteroids used in the third degree stage of COPD have not been explained yet. Although corticosteroids are not used primarily in COPD, they are used in combination with bronchodilator drugs in hypoxemia, and in cases where symptoms are severe and other drugs do not serve. Glucocorticosteroids are powerful anti-inflammatory and immunosuppressive drugs. Systemic corticosteroids have many side effects. Oral or parenteral corticosteroids are used for acute COPD attacks, and they generally work quite effectively [7-9] . Side effects of systemic corticosteroid use include obesity, myopathy, hypertension, psychiatric problems, diabetes mellitus, osteoporosis, thinning of the skin and ecchymosis. Yet inhaled corticosteroids have fewer side effects, and these are due to the accumulation in the oropharyngeal area. The most commonly seen side effects are dysphonia (an impairment in the ability to produce voice sounds), oropharyngeal candidiasis and coughing. Mucositis formation is one of the side effects of these drugs. Correct use of the drug and proper oral care protocols minimize these side effects [4] .
The oral mucosa contains epithelium and connective tissues; it is also the first site for the body’s immune system. The oral mucosa harbors generally harmless micro-organisms. These micro-organisms become harmful and result in infections due to viral, fungal or bacterial activities when the immune system is suppressed (especially when corticosteroids are used). Oral problems that develop due to corticosteroid use, and cause mucositis formation are oral dryness, dental plaque and candida infections [10].
Oral Mucositis
Oral mucositis is described as the inflammation and ulceration of oral mucosa. Typically, it involves erythematous, focal or diffuse ulcerative lesions similar to a bruise. Mucositis becomes severe within seven days, and worsens due to the treatment used [10]. In the oral cavity, it is mostly seen in the moving parts of the mucosa of the cheek such as the lips, soft palate and both sides of the tongue. Generally, factors that affect the frequency and severity of mucositis are age, body structure, bone marrow suppression and decrease in cells that produce blood, dental prostheses, smoking and alcohol use, decayed teeth, decreased liquid consumption, diarrhea, vomiting and drugs such as corticosteroids and chemoterapics [10,11].
Protective function of the epithelium depends mostly on keratin formation and squamatization and desquamation of the epithelium cells [12,13]. As a result of the dysfunction of this mechanism, oral mucositis occurs. Normal renewal of the mucosal layer is adversely affected by the action of drugs such as antineoplastics and corticosteroids. The mucosa gets thinner due to the cells that do not renew and desquamation starts, and mucosa becomes atrophied. Thus, food and drink consumption becomes traumatic and, as a result, the damage in the mucosa gets more severe and ulceration starts. The size of the ulceration expands due to the surface damage that is not treated [14].
Oral mucositis occurs due to the direct toxic effects of the drugs or as an indirect effect of the myelosuppression [13]. New findings from studies conducted on mucositis formation show that it occurs within 2–3 weeks with five major phases: (1) onset, (2) upregulation and response, (3) diffusion and signal, (4) ulceration, and (5) healing [13,14]. After oral mucositis formation, various changes occur within the oral cavity. Color changes can include white areas in the mouth, mouth redness, colorless lesions and ulcers. Oral moisture changes relate to changes in the saliva, such as an increase or decrease in the secretion amount. Hygienic changes arise from mouth odor and color changes of teeth, and general changes in mucosal integrity include mucosal breaks, ulcers and cuts [15-17].
Mucositis associated with acute and chronic symptoms causes anorexia, cachexia, dehydration and malnutrition to the extent that parenteral nutrition may be required [13,15]. Mucositis causes difficulty in chewing, swallowing and speaking, inflammation, edema and lesions. Pain associated with mucositis is the most reported complaint by patients [17]. Mucositis formation impedes a patient’s motivation to continue with his/her treatment. Mucositis has a major impact on the quality of life, and causes serious clinical complications [13,14].
Oral mucositis and nursing care
Teeth and gum diseases and the presence of mucositis affect basic functions like communication, nutrition, sense of taste and breathing [18,19]. First of all, it is essential to provide a proper diagnosis in order to prevent and treat mucositis. Oral examination should be continued in order to make an early detection of oral lesions throughout the treatment. It is recommended that an oral examination follows a series of guidelines that include:
• Learning about the patient’s history
•Conducting a physical examination
• Undertaking diagnostic tests
• Reviewing the effect on the quality of life [20].
Oral complications cause an increase in the pathogens that come from the lungs or are blood-borne and life-threatening. Regular, continuous oral care that includes patient education is needed in order to prevent these complications [3,20]. Oral care prevents infection and decreases pain and bleeding by assisting the maintenance of healthy microbial flora. Continuation of oral health decreases the risks for dental complications [20,21].
There are many agents used for the treatment of oral mucositis among nursing initiatives, yet nearly all of these agents are chemical substances. Today, there is an increasing tendency for alternative agents because they support treatments and can decrease the complications of medical treatments. Therefore, the use of aloe vera is thought to be an alternative to oral care agents for the treatment of oral mucositis that can be clinically severe [19,22 ]. The fact that “aloe vera” has promising preclinical activities, low price and popularity among patients makes it an ideal alternative drug. When we analyze the data obtained, “aloe vera”, in contrast to all the other known agents, is a totally natural product [18]. The most well-known effects of aloe vera include its role as an antifungal, anti irritant, infection preventive, pain decreasing, detoxification and stimulant for cell growth [23]. Therefore, the use of aloe vera may be helpful for oral care and mucositis treatment. It may be used topically three times a day for many types of injuries thanks to its analgesic effect, except for sporting injuries. Fresh juice made of “aloe vera” leaves is an effective anesthetic for insect-bite in adults. “Aloe vera”, used orally or topically, is effective against many bacteria [23].
Clorhexidine, ethyl alcohol-free antibacterial mouthwash, sodium bicarbonate, isotonic serum commonly used now for oral care and expected to show side effects as antibiotic resistance, bad taste and discoloration [24,25]. Also mentioned chemicals frequently studied but aloe vera solutions, as an oral care solution, have not studied to the same extend. Aloe vera may be used easily for oral care because its topical use is more common than other types of use and have certain amounts of nutrient content. There are no serious complaints about aloe vera in the published research, except retrospective complaints, and this makes aloe vera’s use more widespread [18,24].
Materials and Methods
Ethical issues
Throughout the study, the ethical role for research described in the Helsinki Declaration was followed. The study was approved by Atatürk University Institute of Health Sciences Ethical Council and the headquarters of Yakutiye Research and Education Hospital. Written and verbal consent was gained for every subject, and the participation of these subjects in the study was voluntary. Subjects were explicitly informed about the intervention, and that they had the right to withdraw at any point without giving any reason.
Study population
An experimental design was used in order to evaluate the effect of aloe vera solution on the treatment of mucositis. A university hospital located in Erzurum was the setting for this study. It’s an education and research hospital and 50% of its patients receive medical care/ are treated in this institution. Convenience sampling was used to recruit a sample of 102 patients: Patients who were diagnosed as COPD medically, according to the GOLD criteria, had mucositis formation due to corticosteroid use for a period of six-months or earlier, and who had visited and received medical care at the Department of Pulmonary Diseases of Aziziye Research Hospital between March and July 2009 were included in the research. Of these patients, 42 were excluded from the research because they did not complete the physical examination and practice period of 15 days: 30 patients were discharged, 3 patients died, 4 patients were transferred to another health institution and the treatment protocols of 5 patients were changed. The research was completed with 60 patients who were diagnosed with COPD at the clinics of the hospital, had mucositis due to corticosteroid use, were open to communication and mutual aid, and agreed to participate in the research. Of these patients, 30 were randomly selected into an experimental group and the other 30/the rest made up a/the control group.
Data collection
5 weeks were spent (3 weeks in March 2009 and 2 weeks in April) at the Department of Oral Diagnosis and Radiology of the Faculty of Dentistry of Atatürk University, in order to gain skills in oral mucositis examination before the research commenced. During this time, the researcher observed 10 patients, conducted intra oral examinations together with the dentist, and developed skills in oral pathology by scoring mouth conditions according to the “Mucositis Index of Researcher”.
Instruments
Data collection form: A Patient Diagnosis Form was developed, informed by the literature, and contained characteristic features such as age, sex and educational status of the patient. Personal information such as diagnosis, systemic diseases, intraoral prostheses, smokingalcohol use, decayed teeth, periodontal diseases, habit of regular tooth brushing, habit of regular oral examination, oral dryness and sense of taste, oral hygiene and amount of daily liquid consumption of the patient was also sought [26,27].
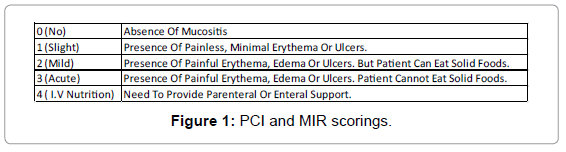
Mucositis scaling index: The “Patient Complaint Index (PCI)” and “Mucositis Index of Researcher (MIR)” were originally developed by Mahood et al. [27] in the USA in 1991, and based on the Mucositis Assessment Index of the World Health Organization. In Turkey, it was used by Sener [28] (Sener 1995) in a study to evaluate the role of oral hygiene and the effect of mouth wash (3x1) with chlorhexidine on mucositis incidence and its severity in 1995 with patients who were undergoing chemotherapy. The PCI and MIR assess the same components when evaluated by patients it is known as PCI; when evaluated by nurses/researchers it is known as MIR [28].
The PCI was used by the patient or a family member from the first day of the medical examination (Day 1) and continued for 15 days with complaints scored according to his/her intra oral pain, and these were marked on the index daily. The MIR was completed by the researcher on the 1st (Day 1) and 15th (Day 15) observational day following a physical examination and determining the severity of oral mucositis. Both indexes were rated on a score from 0 to 4 points. The rating is shown in Figure 1.
The data for the research study were collected between March and July 2009 at the abovementioned clinics of the hospital. The data of the experimental group were obtained after they had undertaken daily oral care with aloe vera solution of 0.5% every 8 hours (3x1) for 15 days. Data were collected from the control group after they had made their standard oral care protocol (mouth wash with abundant water or mouthwash with isotonic serum for painful conditions and tooth brushing). The observational period was determined as 15 days because the time of hospitalization and discharge was shorter at the abovementioned clinics. This period of 15 days is consistent with the healing period of mucositisnoted in the literature [29,30].
The PCI was distributed to the patients of both groups who were literate and had no difficulty understanding what they read, and they were trained about how to evaluate oral mucositis on the first day of the oral care period of the 15-day trial. The use of PCI was taught to the relatives of those who were illiterate and who had difficulty understanding, and they were asked to keep a diary about the patient’s complaints. The researcher performed the tasks below using MIR:
- Patients of both groups were examined on Day 1 and Day 15 of the observational period, and their oral mucositis scores were registered.
- PCI was distributed to the patients/relatives of the patients, and they were instructed about PCI and asked to record their oral complaints daily.
- Intra oral examination was macroscopically carried out by the researcher using a light and examining the floor of the mouth, tongue, palate, cheeks and lips.
Aloe vera gel, made of 97% pure aloe vera and 3% protein and carbohydrate and patented by the American Food and Drug Community, was used in the research. The concentrate was prepared in a liquid bottle of 1000 cc containing 995 cc distilled water and 5cc aloe vera gel, and was made up for patients’ use in a sample bottle of 100 cc. The patients in the experimental group were given special oral care with the prepared concentrate every 8 hours (3x1) for 15 days. The first practice was carried out by the researcher, and the method of special oral care was instructed to the patients who were self-sufficient, and they were watched until they carried out all the steps of the oral care procedure correctly. The practice was taught to the relatives of the patients who were not self-sufficient. Similarly, they were watched until they also carried out all the steps of the oral care procedure correctly. The patients or the relatives that participated in the research were monitored every two days whether they used the concentrate regularly or not. The concentrates that were consumed were prepared again by the researcher. Those solutions that were not consumed within 2 days were prepared again, and thus we enabled the patients to use aloe vera concentration of 100 cc for 2 days. During this time, the concentrates were kept refrigeratated at a temperature between +2 and +4 C0. When a practice was skipped it was repeated, and days in which a practice was skipped were not evaluated.
Statistical analysis
After gathering data, a quantitative analysis was performed using SPSS software, version 11.5. The statistical methods used were the Chisquare test or Fisher’s exact test and two independent samples t-tests to determine the significance of the characteristics for subjects between the control group and the experimental group. Student’s t-test was used to determine the differences between the control and experiment group on gained scores of RMI and PCI. Also Mann-Whitney-U test and Wilcoxon test were used to determine the differences of RMI and PCI scores between the control and experimental group.
Limitations
The short period of hospitalization at the clinics, extensive patient circulation, limited number of subjects and unicentral conduction were the limitations of the study.
Results
Demographic and oral characteristics of participants
The characteristic features of the patients and the distributions according to the groups are shown in Table 1. Experimental and control groups were compared and no significant correlation was found between the groups in terms of sex and educational status (sex x2 = 0,258; p > 0.05, educational status x2 = 0.097; p > 0.05).
| Experiment Group (n=30) | Control Group (n=30) | Total (n=60) | x2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| Age | X= 67.30 | X= 61.20 | ||||||
| Sex | S | % | S | % | S | % | ||
| Male | 23 | 76.7 | 19 | 63.3 | 42 | 70 | 0.258 | p>0.05 |
| Female | 7 | 23.3 | 11 | 36.7 | 18 | 30 | ||
| Education Status | ||||||||
| None writing-reading | 15 | 50 | 13 | 43.3 | 28 | 46.7 | 0.097 | p>0.05 |
| Writing-Reading | 11 | 36.6 | 5 | 16.7 | 16 | 26.7 | ||
| Primary School Graduation | 2 | 6.7 | 9 | 30 | 11 | 18.2 | ||
| Secondary School Graduation | 2 | 6.7 | 2 | 6.7 | 2 | 6.7 | ||
| High school graduation | 0 | 0 | 1 | 3.3 | 3 | 1.7 | ||
| University Graduation | 0 | 0 | 0 | 0 | 0 | 0 | ||
Table 1: Demographic characteristics and statistical comparison of the experiment and control groups.
Distribution of the factors that affected mucositis formation between groups
Significant correlation was noted only between having decayed teeth (53.3% of the experimental group had decayed teeth, whereas, 26.7% of the control group had decayed teeth), oral dryness (96.7% of the experimental group had oral dryness, whereas, 100% of the control group had oral dryness) and teeth brushing twice a day (100% of the experimental group had no teeth brushing habit twice a day, whereas, 86.7 % of the control group had no teeth brushing habit twice a day) (Table 2).
| Characteristics | Experiment Group (n=30) | Control Group (n=30) | Total (n=60) | x2 | p | |||
|---|---|---|---|---|---|---|---|---|
| Systemic Illness | S | % | S | % | S | % | ||
| Yes | 13 | 43.3 | 17 | 56.7 | 30 | 50 | 0.302 | p>0.05 |
| No | 17 | 56.7 | 13 | 43.3 | 30 | 50 | ||
| Oral Prothesis | ||||||||
| Yes | 16 | 53.3 | 16 | 53.3 | 32 | 53.3 | 1 | p>0.05 |
| No | 14 | 46.7 | 14 | 46.7 | 28 | 46.7 | ||
| Regular Oral Examination | ||||||||
| Yes | 0 | 0 | 1 | 3.3 | 1 | 1.7 | 0.313 | p>0.05 |
| No | 30 | 100 | 29 | 96.7 | 59 | 98.3 | ||
| Periodontal Illness | ||||||||
| Yes | 8 | 26.7 | 13 | 43.3 | 21 | 35 | 0.176 | p>0.05 |
| No | 22 | 73.3 | 17 | 56.7 | 39 | 65 | ||
| Smoking | ||||||||
| Yes | 0 | 0 | 1 | 3.3 | 1 | 3.3 | ||
| No | 13 | 43.3 | 12 | 40 | 25 | 41.7 | 0.595 | p>0.05 |
| Give up | 17 | 56.7 | 17 | 56.7 | 34 | 56.7 | ||
| Tooth Decay | ||||||||
| Yes | 16 | 53.3 | 8 | 26.7 | 24 | 40 | 0.035 | p<0.05 |
| No | 14 | 46.7 | 22 | 73.3 | 36 | 60 | ||
| Teeth Brushing | ||||||||
| Yes | 0 | 0 | 4 | 13.3 | 4 | 6.7 | 0.038 | p<0.05 |
| No | 30 | 100 | 26 | 86.7 | 56 | 93.3 | ||
| Oral Dryness | ||||||||
| Yes | 29 | 96.7 | 30 | 100 | 59 | 98.3 | 0.313 | p>0.05 |
| No | 1 | 3.3 | 0 | 0 | 1 | 1.7 | ||
| Taste Changes | ||||||||
| Yes | 30 | 100 | 28 | 93.3 | 58 | 96.7 | 0.15 | p>0.05 |
| No | 0 | 0 | 2 | 6.7 | 2 | 3.3 | ||
| Oral Hygiene | ||||||||
| Good | 0 | 0 | 0 | 0 | 0 | 0 | 0.063 | p>0.05 |
| Bad | 15 | 50 | 22 | 73.3 | 37 | 61.7 | ||
| Worse | 15 | 50 | 8 | 26.7 | 23 | 38.3 | ||
| Daily Liquid Intake | ||||||||
| Under 500 ml | 6 | 20 | 7 | 23.3 | 13 | 21.7 | 0.159 | p>0.05 |
| 501-1000 ml | 12 | 40 | 16 | 53.3 | 28 | 46.7 | ||
| 1001-1500 ml | 3 | 10 | 5 | 16.7 | 8 | 13.3 | ||
| 1501-2000 ml | 8 | 26.7 | 1 | 3.3 | 9 | 15 | ||
| Above 2001 | 1 | 3.3 | 1 | 3.3 | 2 | 3.3 | ||
Table 2: Comparison of factors which effect oral mucositis in the experiment and control groups. Distribution of PCI and MRI scores.
There was a statistically significant correlation between the scores found on Day 1 and Day 15 of the experimental group (z = -4.536, p = .000; p<0.001). As a result of the analysis, there was no statistical difference between the scores on the Day 1 and Day 15 of the control group (z = -0.257, p = 0.789; p>0.05) (Table 3).
| “PCI” Score | |||||||
|---|---|---|---|---|---|---|---|
| Experiment Group | Control Group | ||||||
| Z* | p | Significance | Z* | p | Significance | ||
| 1st-15th Day | -4.536 | 0 | p<0.001 | 1st-15th Day | -0.257 | 0.789 | p>0.05 |
Table 3: Comparision of “Patient Complaint Index” Scores.
Statistical correlation between mean MIR scores on Day 1 and Day 15 of both the experimental and control groups is shown in Table 4. A significant correlation was noted between the scores on Day 1 and Day 15 of the experimental group (z = -4.536, p = .000; p<0.001).
| “RMI” Score | |||||
|---|---|---|---|---|---|
| Experiment group 1st day - Control group 1st day |
Experiment group 15th day - Control group 15th day |
||||
| Z* | p | Significance | Z* | p | Significance |
| -0.204 | 0.838 | p>0.05 | -2.778 | 0.05 | p<0.05 |
Table 4: Comparision of experiment and control groups’ 1st and 15th day “RMI” score.
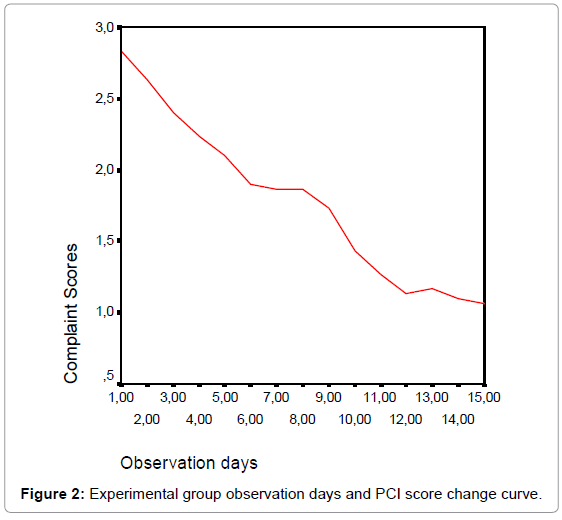
As the change curve of complaint degree of the experimental group according to the observational days indicates, we found a decrease in the complaint degree as the practice days commenced (Figure 2).
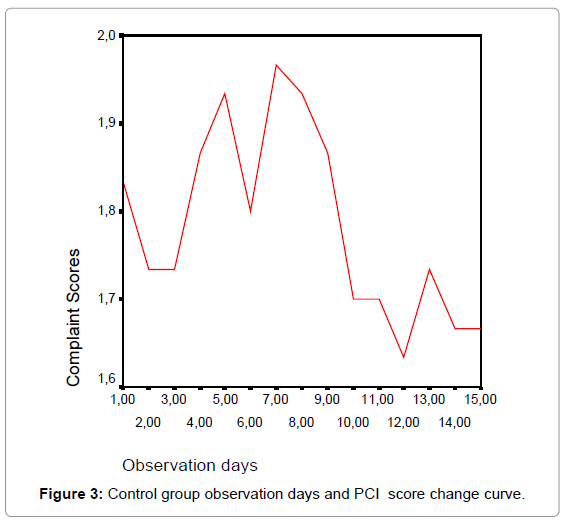
As the change curve of complaint degree of the control group according to the observational days indicates, we did not find a regular decrease in the complaint degree; to the contrary, an increase during certain periods was observed (Figure 3).
According to the Table 4, no statistically significant difference was found between the comparison of the scores of the experimental and control group on Day 1, whereas, there was a statistically significant difference between scores of the groups on Day 15.
Discussion
This experimental trial with the control group provided data to assess the effectiveness of an oral care intervention which made use of aloe vera solutions to heal oral mucositis in COPD patients. Existing evidence demonstrates that oral care which is regular and maintained with a care agent is preventive for oral mucositis [13,29]. The results of this study have provided initial support for the benefits of using an oral careprotocol to reduce the severity of oral mucositis in COPD patients.
The factors that support the oral mucocitis occurence (oral dryness, bad oral hygiene, etc.) were present in most of the participants in this study. These are the complications that are most complaint by the patients with mucositis. Saadeh and Sonis et al. found oral dryness was one of the factors associated with mucositis occurrence. Oral dryness has symptoms that impact an individual’s communicational skills and body image due to the difficulty it brings about in swallowing and speaking and a sense of sticking of the tongue. It also becomes easier for the dry mucous membrane to have a deteriorated integrity [27,28]. These complaints and the severity of oral mucositis can be reduced with the regular oral care protocol [13,31,32].
How good oral health is is related to the overall health and wellness; it is integral to the prevention and treatment of mucositis. Although there have not been large randomized controlled trials to test the benefit of basic oral care, few experts in the field would question its foundational importance [31,32]. Frequently, studies have included basic oral care as a comparison with new therapies. Interestingly, these studies often fail to show the desired significant difference, contributing support for the importance of basic oral hygiene [33-35]. This trial can be added to those examples because of the comparision of the aloe vera solution with routine oral care.
This trial provides evidence that oral care with aloe vera as an intervention could be effective in reducing the oral mucisitis level and be supportive for healing. Study findings also revealed that paticipants in the experimental group had significantly less mucositis-related complaints. Salvador et al. (2012) found that oral care protocol+ cryotheraphy reduced the pain related with mucositis. Also Cheng et al. reported that preventive oral care (tooth brushing+ 0.9% sodium chloride+ 0.2% chlorhexidine mouth rinse) reduced the severity of mucositis [14,31].
The limited number of subjects and unicentral conduction may be the limitations of the trial. Thus, the results cannot be generalized. This trial needs to be replicated with wider samples and multicenter studies. The agent needs to be used in different oral care patient groups.
Conclusion
Findings obtained showed that the oral care with aloe vera reduced patients’ oral complaints and allowed an evident decrease in oral mucositis levels. The decrease in general pain may be attributed to the analgesic effect of aloe vera, whereas, the evident decrease in mucositis levels could be attributed to its antibacterial, healing and cell-stimulant effect. The findings obtained are important in that they can be used for clinical practices based on evidence. Therefore, a systemic oral diagnosis based on evidence for all patient groups — mainly those suffering from chronic disorders is essential in order to provide oral hygiene. Nurses should have sufficient knowledge about oral care so that they can make this diagnosis. Oral hygiene is a self-care practice, so patient training should be emphasized during nursing care.
Acknowledgement
The research was funded by the Council of Scientific Research Projects of Atatürk University with the project number of 2009/154. We would like to express our appreciation to all the patients who participated in this study and to the medical personnel of the Chest Diseases Clinic of Yakutiye Research and Education Hospital for their assistance in collecting data.
References
- Ohrn KE, Wahlin YB, Sjödén PO (2000) Oral care in cancer nursing. Eur J Cancer Care (Engl) 9: 22-29.
- MacEntee MI, Hole R, Stolar E (1997) The significance of the mouth in old age. Soc Sci Med 45: 1449-1458.
- Scully C, Porter S (2000) ABC of oral health. Oral cancer. BMJ 321: 97-100.
- Akça Ay F (2008) Fundamentals of Nursing: Daily self care interventions. Istanbul Medical Publication Istanbul.
- Mendieta C, Reeve CM (1993) Periodontal manifestations of systemic disease and management of patients with systemic disease. Curr Opin Periodontol .
- Youngblood M, Williams PD, Eyles H, Waring J, Runyon S (1994) A comparison of two methods of assessing cancer therapy-related symptoms. Cancer Nurs 17: 37-44.
- Kunter E, Piran G (1999) Chronic obstructive lung cancer, bronchiolitis cystic fibrosis. J Act Med 4: 124-137.
- Lenfant C, Khaltaev N (2008) Global Initiative for Chronic obstructive pulmonary disease. Global enterprises against chronic Obstructive Lung Cancer. Translation: Kocabas A, Turgut Broadcasting Trade Corporation, Istanbul.
- Erdinç E, Erk M, Kocabas A (2000) Tukish Thorax Society Researh Group Diagnosis and Treatment Guide of Chronic Obstructive Pulmonary Disease.
- Institute for Clinical Systems Improvement (2003) Chronic obstructive pulmonary disease: Institute for Clinical Systems Improvement Health Care guideline. Chronic Obstructive Lung Cancer. Syndrom II 2: 1-25.
- Wilkes JD (1998) Prevention and treatment of oral mucositis following cancer chemotherapy. Semin Oncol 25: 538-551.
- Holmes S (1998) Xerostomia: aetiology and management in cancer patients. Support Care Cancer 6: 348-355.
- Sonis ST (2004) Pathobiology of mucositis. Semin Oncol Nurs 20: 11-15.
- Cheng KK, Molassiotis A, Chang AM (2002) An oral care protocol intervention to prevent chemotherapy-induced oral mucositis in paediatric cancer patients: a pilot study. Eur J Oncol Nurs 6: 66-73.
- Hermiz O, Comino E, Marks G, Daffurn K, Wilson S, et al. (2002) Randomised controlled trial of home based care of patients with chronic obstructive pulmonary disease. BMJ 325: 938.
- Grap MJ, Munro CL, Ashtiani B, Bryant S (2003) Oral care interventions in critical care: frequency and documentation. Am J Crit Care 12: 113-118.
- Majorana A, Schubert MM, Porta F, Ugazio AG, Sapelli PL (2000) Oral complications of pediatric hematopoietic cell transplantation: diagnosis and management. Support Care Cancer 8: 353-365.
- World Health Organization (2002) WHO Monographs on selected medicanal plants, Volume 2. Geneva: World Health Organization
- Rubenstein EB, Peterson DE, Schubert M, Keefe D, McGuire D, et al. (2004) Clinical practice guidelines for the prevention and treatment of cancer therapy-induced oral and gastrointestinal mucositis. Cancer 100: 2026-2046.
- In PY, Hyung JT (2006) New perspectives on aloe: Perspective of industrial application of Aloe vera. Springer, US.
- Reynolds T, Dweck AC (1999) Aloe vera leaf gel: a review update. J Ethnopharmacol 68: 3-37.
- Ross, IA (1999) Medicinal Plants of the World (2nd edn) Chemical Constituents, Traditional and Modern Medicinal Uses. Totowa: Humana Press 1: 103-122.
- Mahood DJ, Dose AM, Loprinzi CL, Veeder MH, Athmann LM, et al. (1991) Inhibition of fluorouracil-induced stomatitis by oral cryotherapy. J Clin Oncol 9: 449-452.
- Binkley C, Furr LA, Carrico R, McCurren C (2004) Survey of oral care practices in US intensive care units. Am J Infect Control 32: 161-169.
- Özden D, Türk G, Düger C, Güler EK, Tok F, et al. (2014) Effects of oral care solutions on mucous membrane integrity and bacterial colonization. Nurs Crit Care 19: 78-86.
- Sener BC (1995) The role of methotrexate area of 0.2% chlorhexidine rinse and oral hygiene on oral complication occurance in patients with methotrexate+5 Fluorouracil combination. Hacettepe University Health Sciences Institute, Unpublished Doctorate Thesis, Ankara.
- Rennard SI, Fogarty C, Kelsen S, Long W, Ramsdell J, et al. (2007) The safety and efficacy of infliximab in moderate to severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med 175: 926-934.
- Anthony L, Bowen J, Garden A, Hewson I, Sonis S (2006) New thoughts on the pathobiology of regimen-related mucosal injury. Support Care Cancer 14: 516-518.
- Karag ÃzoÄŸlu S, Filiz Ulusoy M (2005) Chemotherapy: the effect of oral cryotherapy on the development of mucositis. J Clin Nurs 14: 754-765.
- Ohrn KE, Wahlin YB, Sjödén PO (2001) Oral status during radiotherapy and chemotherapy: a descriptive study of patient experiences and the occurrence of oral complications. Support Care Cancer 9: 247-257.
- Salvador P, Azusano C, Wang L, Howell D (2012) A pilot randomized controlled trial of an oral care intervention to reduce mucositis severity in stem cell transplant patients. J Pain Symptom Manage 44: 64-73.
- Eilers J, Million R (2011) Clinical update: prevention and management of oral mucositis in patients with cancer. Semin Oncol Nurs 27: e1-16.
- McGuire DB, Correa ME, Johnson J, Wienandts P (2006) The role of basic oral care and good clinical practice principles in the management of oral mucositis. Support Care Cancer 14: 541-547.
- Eilers J, Epstein JB (2004) Assessment and measurement of oral mucositis. Semin Oncol Nurs 20: 22-29.
- Dodd MJ, Facione NC, Dibble SL, MacPhail L (1996) Comparison of methods to determine the prevalence and nature of oral mucositis. Cancer Pract 4: 312-318.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 18089
- [From(publication date):
December-2014 - Sep 04, 2025] - Breakdown by view type
- HTML page views : 13269
- PDF downloads : 4820