The Effectiveness of Polypropylene Mesh in the Open and Laparoscopic Repair of Divarication of the Recti
Received: 28-Mar-2016 / Accepted Date: 09-May-2016 / Published Date: 04-Feb-2016
Abstract
Background and objectives: There are no current guidelines for the optimal treatmentof divarication of the recti. Few papers addressed the clinical utilization of polypropylene mesh in the management of divarication of the recti, but none investigated the effectiveness regarding the functional and cosmetic outcome. Therefore, in this article, we aim to evaluate the effectiveness of polypropylene mesh implant in the surgical management of divarication of the recti. Materials and methods: A retrospective cohort database analysis of the treatment outcome of 216 patients who were treated surgically, open and laparoscopic, for divarication of the recti between January 2004 and December 2013 was done. Results: 31 (14.4%) patients were males and 185 (85.6%) were females. The mean age was 40.9 ± 2.7 years. The mean body mass index was 26.39 ± 2.8 kg/m2. The mean preoperative inter-recti distance was 10 cm. Polypropylene mesh reinforcement repair was done through open method to 179 (82.9%) and laparoscopic to 37 (17.1%). The mean decrease in abdominal girth for the laparoscopic method patients was 11 ± 1.27 cm, and for the open method patients was 12.5 ± 1.53 cm. In both groups, 197 (91.2%) reported a good abdominal muscle tone. The recurrence rate was 0% in both groups after 24 months follow-up. Conclusion: Polypropylene prosthetic mesh repair for divarication of the recti, open or laparoscopic, is an effective, safe and durable modality. It is associated with a favourable outcome and minor complications, although it requires a meticulous dissection and skillful, well-conducted implantation of the mesh.
Keywords: Polypropylene prosthetic mesh, Divarication of the recti, Diastasis recti, Surgical repair
78920Introduction
Divarication of the recti (Diastasis recti) is the separation of the rectus abdominis muscle into right and left halves (a gap of roughly 2.7 cm or greater), usually due to thinning and stretching of the linea alba resulting from various reasons. Typically, the two sides of the muscle are joined at the linea alba at the body midline. Divarication of the recti would appear as a long ridge extending down the abdominal midline from the xiphoid process to the umbilicus. It will become more prominent with straining and may disappear when the abdominal muscles are relaxed. It is reported to be more common in multiparous women (about 66%) due to the repeated episodes of stretching [1,2].
The most common reported etiologic factors include chronic or intermittent abdominal distension, advancing age, or familial weakness of the abdominal musculofascial tissues. Women over the age of 35, the high birth weight of the child, multiple birth pregnancy, multiple pregnancies, and excessive abdominal exercises after the first trimester of gestationare particular to the female gender. Genetic predisposition, ascites, chronic obstructive pulmonary disease, were also reported [3,4].
Whatever the cause or type, divarication occurs mainly due to a widening of the linea alba, and can be measured as the inter-recti distance (IRD). However, because the two recti muscles are attached in the middle by the linea alba, the widening occurs as a result of stretching and thinning of the linea alba. Therefore, rectus abdominis divarication should be considered as a widening in the IRD rather than a true separation [5]. The literature conflicted in that regard. It had been defined as the separation of the recti bellies at the linea alba when the IRD is >1.5 cm >2 cm >2.5 cm and >2 finger widths during a partial sit-up [6].
Divarication of the recti reduces the integrity and functional strength of the abdominal wall and can aggravate lower back pain and pelvic instability, but there is no associated mortality with this condition. It is by itself not a true hernia and not considered a risk of strangulation. The repair in most cases is donefor cosmetic reasons only. The condition could not necessitate a surgical repair where the conservative management is accepted as an alternative. In fact, the protrusion of the abdomen, rather than the divarication itself should influence the decision of repair [7].
To date, there are no current guidelines for the optimal treatment of divarication of the recti. The surgical repair is not very popular because of the associated morbidity and cosmetically unacceptable results. Recently there were many attempts by different surgeons to reduce the morbidity and length of scar associated with conventional open procedures [8].
Laparoscopic repair of divarication of the recti has seldom been described in the literature. Clinical reports on the laparoscopic repair are still rare. The open procedures were reported to have many complications such as hematoma, seroma formation, increased infection rate, contour abnormalities that may be permanent, hypertrophic scars, and flap necrosis. However, the laparoscopic repair was reported in a few articles to be cosmetically more acceptable without significantly associated morbidities and is a promising future technique for repair of divarication of the recti [9].
The development and introduction of polypropylene prosthetics revolutionized surgery for the repair of abdominal wall defects and divarication. A tension-free mesh method has drastically reduced the recurrence rates for all hernias compared to tissue repairs. It has made it possible to reconstruct many large ventral defects that were previously tough to correct. The repair of defects of the abdominal wall is one of the most commonly performed general surgical procedures worldwide, with over 1 million polypropylene implants inserted each year. Unfortunately, little research has been conducted to investigate factors like the effect of abdominal wall forces interaction on a ventral hernia repair and the required amount or necessary strength of the foreign-body material needed for a proper hernia repair. The long-term consequences of the implanted polypropylene prosthetics should be in concern. The human body generates an intense inflammatory response to the prosthetic which could result in a scar plate formation, an increased stiffness of the abdominal wall, and the shrinkage of the biomaterial. By reducing the density of polypropylene and creating a ''light weight'' mesh theoretically induces aless foreign-body response, causes less contraction or shrinkage of the mesh, results in improved abdominal wall compliance, and allows for better tissue incorporation [10].
Many mesh materials were clinically tested. The most commonly used in the surgical practice are polypropylene (Marlex, Prolene), polyestermesh (Dacron, Mersilene), and expanded polytetrafluoroethylene (PTFE) [11]. Scientific studies showed that the tissue fluid should not physically modify the ideal prosthetic mesh material, biochemically inert, non-inflammable, not causing foreign body reaction, non-carcinogenic, non-allergenic or inducing hypersensitivity reactions, capable of resisting mechanical strains, capable of being fabricated in the form required, and capable of being sterilized [12]. Soft polypropylene mesh demonstrates an acceptable low complication and hernia recurrence rates when utilized as a reinforcement of ventral hernia closureof the midline in conjunction with components separation [13].
The reported properties of polypropylene mesh that made it more acceptable than other types of mesh included its readability for insertion into any size without fragmentation, causing no discomfort when used in the groin. It is less affected by infection, having high tensile strength, resistant to most chemicals, softening temperature 260°F (127°C), and accepts sterilization by boiling, high burst strength and tensile strength for a strong repair, and the bidirectional elastic property which allows adaptation to various stresses encountered in the body [14].
It is the primary option to apply prosthesis materials. It has a high tension and displosion resistance between thickness values of 0, 30 mm and 0, 60 mm and accelerates tissue healing thanks to its braided texture. It is biologically compliant, flexible, robust, and lucid. It provides ideal pore interval for tissue healing and high power and displosion resistance for sustainable support. It does not cluster and stays strong for long periods of time [15].
A thorough literature review revealed few papers addressing the clinical utilization of polypropylene mesh in the management of divarication of the recti, but none was found to investigate the effectiveness regarding the functional and cosmetic outcome. Therefore, in this article, we aim to evaluate the effectiveness of polypropylene mesh implant in the surgical management of divarication of the recti among Saudi Arabian patients regarding the functional and cosmetic outcome.
Materials and Methods
A retrospective cohort database analysis of the treatment outcome of 216 Saudi Arabian patients who were treated surgically for divarication of the recti between January 2004 and December 2013 in Al Ansar public health general hospital in Medina, Saudi Arabia was done. The analysis was approved by the quality care subcommittee for management guidelines and clinical pathway (as part of our quality care program) and the clinical research committee of the department of surgery at Al Ansar hospital.
All the patients had the same preoperative workup (complete blood count- coagulation profile- blood chemistry- chest X-ray electrocardiogram- abdominal ultrasound, and computed tomography scan). The procedure and postoperative care were carefully discussed with the patients. All the patients were admitted to the surgical floor one day before surgery and were discharged home on the second postoperative day. All the patients had a single preoperative antibiotics dose (cefazolin and metronidazole), and three doses of the same antibiotics postoperatively (once every 8 hours).
Our standard procedure in all the patients in the open method was done as follows: under general anesthesia, supine position, the skin incision was performed through a vertical incision from the xiphoid process to the umbilicus, the skin is then elevated to expose the linea alba and 4-6 cm of the anterior rectus fascia bilaterally. The retrorectus space was created by incising the anterior rectus fascia along the medial muscle border, freeing the muscle from the underlying posterior rectus sheath with blunt dissection. The anterior rectus sheath was left attached to the rectus muscle to maintain its vascularity. Low weight macroporous polypropylene uncoated mesh, 7 cm in transverse dimension, is anchored with 30-40 interrupted transrectus 0-polypropylene sutures with a 4 cm distance from the incised edge of the anterior rectus fascia, placed approximately 2 to 3 cm apart. The mesh becomes flat and tight across the midline at the end tying down the sutures, creating a high tension closure, but the force is distributed across many individual sutures, thus avoiding suture pullthrough. The rectus muscles and the overlying anterior rectus fascia are approximated in the midline with interrupted 0-polypropylene sutures to achieve a directly supported repair.
The laparoscopic procedure was done as follows: supine (trendelenburg) position. Pneumoperitoneum through Verres needle (12 mmHg). Three laparoscopic ports approach, a camera port (10 mm) in the epigastrium 2 cm below the xiphoid process to the right of the falciform ligament, two working ports (5 mm) in the right and left hypochondrium along the anterior axillary line. The linea alba was plicated in the midline with continuous horizontal sutures (0-proline double loop sutures) 2-3 cm on each side of the midline through the separated rectus sheath all along the defect from the suprapubic area until 2 cm above the umbilicus. While tightening, the intraperitoneal pressure was reduced to 8 mmHg, and manual compression from outside over the abdominal wall was applied to create there formed linea alba. A polypropylene mesh was implanted to reinforce the plication placed along the length and fixed with 1-polypropylene sutures, 3 cm apart, and circumferentially around the mesh.
Postoperative pain was controlled with intravenous paracetamol 1g every 8 hours for one day, followed by oral analgesics on the second day for one week. 68 (38%) required intramuscular meperidine 75 mg for severe pain in the first 12 hours postoperatively. Postoperatively, for patients in both the open and the laparoscopic methods, we applied an adhesive compression surgical bandage over the abdomen for the first 24 hours. The patients were advised to wear an abdominal binder (corset) for the following four weeks. All the patients were scheduled for follow-up in the outpatient clinic once every week for one month, then once every one month for six months, and once every six months for a total of 24 months.
Results
216 Saudi Arabian patients who were treated surgically for divarication of the recti were included in the study. 31 (14.4%) patients were males and 185 (85.6%) were females. Male to female ratio (1:5.96). The mean age was 40.9 ± 2.7 years (range, 36–49). The mean body mass index (BMI) was 26.39 ± 2.8 kg/m2 (range, 24.7–33.6). The mean preoperative IRD, measured by computed tomography scan, was 10 cm, range 7-13 (Table 1).
| Patients group | Patients Number Male Female |
The mean age | The mean BMI | The mean preoperative IRD | The mean decreases in abdominal girth | |
|---|---|---|---|---|---|---|
| Open with mesh | 179 (82.9%) 159 (88.2%) | 40.9 ± 2.7 years | 26.39 ± 2.8 kg/m2 | 10 cm | 12.5 ± 1.53 cm | |
| 20 (11.2%) | 159 (88.2%) | |||||
| Laparoscopic with mesh | 37 (17.1%) | 40.9 ± 2.7 | 26.39 ± 2.8 kg/m2 | 10 cm | 11 ± 1.27 cm | |
| 11 (29.7%) | 26 (70.3%) | years | ||||
Table 1: The data of divarication of the recti patients.
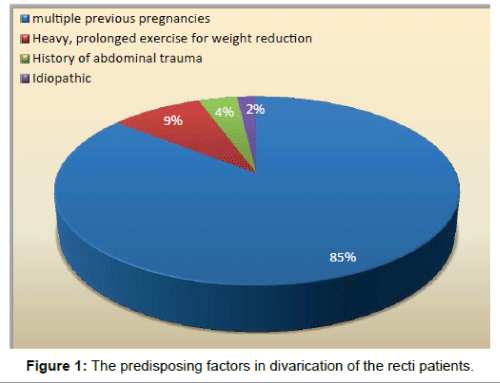
The most common predisposing factor was multiple previous pregnancies in 185 (85.6%) patients, all (100%) were females. Heavy, prolonged exercise for weight reduction, in previously obese patients, in 19 (8.8%) patients. History of abdominal trauma in 8 (3.7%) patients. Idiopathic in 4 (1.9%) patients (Figure 1).
The most common reason for requesting surgical management was cosmetic in 137 (63.4%) patients among which 116 (84.7%) were females and 21 (15.3%) were males. Abdominal protrusion and pain were reported by 52 (24.1%). Back pain and postural changes were reported by 27 (12.5%). Open repair with polypropylene mesh reinforcement was done to 179 (82.9%), among which 159 (88.2%) were females, and 20 (11.2%) were males. Laparoscopic repair with polypropylene mesh reinforcement was done to 37 (17.1%) of which 26 (70.3%) were females, and 11 (29.7%) were males. The mean operative time for the open method was 92.06 ± 25 minutes, range 78–107. The mean operative time for the laparoscopic method was 127.1 minutes, range 118 – 137.
Postoperative complications in the open method group were recordedas tightness in the abdomen in 37 (20.7%) patients, wound infection in 11 (6.1%), seroma in 9 (5%), hematoma in 5 (2.8%), and foreign body sensation in 3 (1.7%). Postoperative complications in the laparoscopic method group were recorded as tightness in the abdomen in 9 (24.3%), abdominal pain in 4 (10.8%) and foreign body sensation in 3 (8.1%). The recurrence rate was 0% in both groups after 6, 12, 18, and 24 months follow-up. The mortality rate was 0% in both groups.
The mean decrease in abdominal girth for the open method patients was 12.5 ± 1.53 cm (range: 9–16 cm).The mean decrease in abdominal girth for the laparoscopic method patients was 11 ± 1.27 cm (range: 8–14 cm). A computed tomography scan was done to all the patients four weeks postoperatively which showed complete obliteration of IRD in all patients (100%). The cosmetic outcome in the open method group, from the patient perspective, was reported as excellent in 124 (90.5%), good in 7 (5.1%), unsatisfactory in 6 (4.4%). The cosmetic outcome in the laparoscopic method group, from the patient perspective, was reported as excellent in 28 (75.7%), good in 6 (16.2%), unsatisfactory in 3 (8.1%). In both groups, 197 (91.2%) reported a good abdominal muscle tone that enabled them to perform regular activities while 19 (8.8%) reported moderate muscle tone, but not limiting their activities.
Discussion
The mean age in our study patients was 40.9 ± 2.7 years (range, 36–49) with the male to female ratio (1:5.96, female predominance). It corresponds to the most common predisposing factor for divarication of the recti in our series, multiple previous pregnancies in 185 (85.6%) patients. The mean BMI was 26.39 ± 2.8 kg/m2 (range, 24.7–33.6) which reflect the fact that most of our patients had a good body built, not obese, an observation that might have contributed positively to the good result. We used a 15 × 15 cm polypropylene mesh in all the patients given that the mean preoperative IRD, measured by computed tomography scan, was 10 cm, range 7-13. Despite the large size, implanting the mesh was smooth and proper, thanks to the superb flexibility and biosynthetic characteristics of the mesh.
Most surgeons believe that abdominal wall defects are best repaired using prosthetic mesh compared to simple suturing while such agreement does not exist for the repair of divarication of the recti. The reported factor of the return of muscle laxity in certain patient populations was as high as 100 percent with the method of the plication technique alone [16]. Therefore, many surgeons and authors have recommended a mesh overlay to support the midline plication in patients presenting with significant musculoaponeurotic laxity [17,18]. Our approach of implanting a polypropylene mesh, in both the open and laparoscopic methods, had a good outcome regarding the abdominal muscle tone and decrease in abdominal girth. We believe that the polypropylene mesh reinforcement of the abdominal wall, rather than the plication, played a crucial role in the excellent results achieved.
Some surgeons have recommended a posterior rectus sheath plication, rectus advancement, and anterior rectus aponeurosis fixation to the posterior rectus sheath [19]. Laparoscopic general surgeons have recommended a laparoscopic mesh-reinforced method and considered divarication of the rectiasa hernia without a defect that should be treated similarly to hernia repair techniques [20]. Still others do not believe that divarication of the recti repair will last in the setting of extensive intra-abdominal fat volume or male pattern rectus diastasis and, therefore, recommend against repair [21]. Many authors express concern that rectus plication could introduce the risk of ventral hernia development [22]. Given the results of our study, we recommend the standardization of plication and mesh reinforcement for repair of divarication of the recti.
The previous concerns have prevented many surgeons from attempting repair of significant divarication of the recti, mostly in men. As the use of mesh was introduced, an entire industry of bioprosthetic meshes developed to avoid the fear of prosthetic mesh complications in abdominal wall reconstruction. Surgical wound occurrences are quoted in the 14 to 43 percent range for clean or clean-contaminated abdominal wall reconstruction, a number not compatible with aesthetic procedures [23]. In our series, postoperative complications were in the small range and were managed safely without asignificant adverse outcome. It is our belief that the implantation of the polypropylene mesh was safe, effective, and did not contribute to the postoperative complication which, in fact, was related to the whole procedure and the late advanced presentation.
Many published clinical reports showed that the open method for divarication of the rectihas many complications such as seroma and hematoma formation, development of hypertrophic scars, an increased infection rate, individual contour abnormalities which may become permanent. On the other hand, the laparoscopic repair was found to be cosmetically more acceptable without significantly associated morbidities and is a promising future technique for repair of divarication of the recti [24,25]. In our study, despite that postoperative complications were more in the open group compared to the laparoscopic, both methods showed good results in the long term regarding the functional and cosmetic outcome.
A zero recurrence after 24 months follow-up, a real decrease in abdominal girth, a satisfactory cosmetic outcome, and the achievement of good abdominal muscle tone represent useful predictors of the effectiveness of polypropylene mesh in the repair of divarication of the recti.
Conclusions
Polypropylene prosthetic mesh repair for divarication of the recti, open or laparoscopic, is an effective, safe and durable modality. It is associated with a favourable outcome and minor complications, although it requires a meticulous dissection and skillful, wellconducted implantation of the mesh.
Authors’ contributions
All authors have substantially contributed to the paper. HAS conducted the clinical part of the study. BHS wrote, edited the manuscript, and analyzed the data. Both authors read and approved the final manuscript.
References
- Brauman D (2008) Diastasis Recti: Clinical Anatomy. PlastReconstrSurg 122: 1564-9.
- Benjamin DR, Van de water AT, Peiris CL (2014) Effects Of Exercise on Diastasis of the Rectus Abdominis Muscle in the Antenatal and Postnatal Periods: A Systematic Review. Physiotherapy 100: 1-8.
- Akram J, Matzen SH (2014) Rectus Abdominis Diastasis. J PlastSurg Hand Surg 48: 163-9.
- Hickey F, Finch JG, Khanna A (2011) A Systematic Review on the outcomes of Correction of Diastasis of the Recti. Hernia 15: 607-14.
- Nahas FX, Ferreira LM, Augusto SM, Ghelfond C (2005) Long-term follow-up of correction of rectus diastasis. PlastReconstrSurg 115: 1736-41.
- Coldron Y, Stokes MJ, Newham DJ, Cook K (2008) Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther 13: 112-21.
- Sahoo MR, Kumar AT (2014) Laparoscopic plication and mesh repair for diastasis recti: A case series. Int J Case Rep Images 5: 610–613.
- Palanivelu C, Rangarajan M, Jategaonkar PA, Amar V, Gokul KS, et al. (2009) Laparoscopic repair of diastasis recti using the 'Venetian blinds' technique of plication with prosthetic reinforcement: a retrospective study. Hernia 13: 287-92.
- De'ath HD, Lovegrove RE, Javid M, Peter N, Magee TR, et al. (2010) An assessment of between-recti distance and divarication in patients with and without abdominal aortic aneurysm. Ann R CollSurgEngl 92: 591-4.
- Ko JH, Salvay DM, Paul BC, Wang EC, Dumanian GA (2009) Soft polypropylene mesh, but not cadaveric dermis, significantly improves outcomes in midline hernia repairs using the components separation technique. Plast Reconstr Surg 124: 836-47.
- Agarwal BB, Agarwal KA, Mahajan KC (2009) Prospective double-blind randomized controlled study comparing heavy- and lightweight polypropylene mesh in totally extraperitoneal repair of inguinal hernia: early results. SurgEndosc 23: 242-7.
- Aufenacker TJ, Koelemay MJ, Gouma DJ, Simons MP (2006) Systematic review and meta-analysis of the effectiveness of antibiotic prophylaxis in prevention of wound infection after mesh repair of abdominal wall hernia. Br J Surg 93: 5-10.
- Vrijland WW, Van den Tol MP, Luijendijk RW, Hop WC, Busschbach JJ, et al. (2002) Randomized clinical trial of non-mesh versus mesh repair of primary inguinal hernia. Br J Surg 89: 293-7.
- Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. SurgInnov 12: 63-9.
- Holste JL (2005) Are meshes with lightweight construction strong enough? IntSurg 90:S10-2.
- Al-qattan MM (1997) Abdominoplasty in multiparous women with severe musculoaponeurotic laxity. Br J Plast Surg 50: 450-5.
- Marques A, Brenda E, Pereira MD, De castro M, Abramo AC (1995) Plicature of abdominoplasties with Marlex mesh. Ann PlastSurg 34: 117-22.
- Prado A, Andrades PR, Benitez S (2004) Abdominoplasty: the use of polypropylene mesh to correct myoaponeurotic-layer deformity. Aesthetic Plast Surg 28: 144-7.
- Nahas FX (2001) An aesthetic classification of the abdomen based on the myoaponeurotic layer. PlastReconstrSurg 108: 1787-95.
- Lockwood T (1998) Rectus muscle diastasis in males: primary indication for endoscopically assisted abdominoplasty. Plast Reconstr Surg 101: 1685-91.
- Montgomery A (2013) The battle between biological and synthetic meshes in ventral hernia repair. Hernia 17: 3-11.
- Nahas FX, Ferreira LM, Mendes Jde A (2004) An efficient way to correct recurrent rectus diastasis. Aesthetic Plast Surg 28: 189-96.
- Chaouat M, Levan P, Lalanne B, Buisson T, Nicolau P, et al. (2000) Abdominaldermolipectomies: early postoperative complications and long-term unfavorable results. PlastReconstrSurg 106: 1614-8.
- Vastine VL, Morgan RF, Williams GS, Gampper TJ, Drake DB,et al. (1999) Wound complications of abdominoplasty in obese patients. Ann Plast Surg 42: 34-9.
Citation: Shirah BH, Shirah HA (2016) The Effectiveness of Polypropylene Mesh in the Open and Laparoscopic Repair of Divarication of the Recti. J Med Imp Surg 1:105.
Copyright: © 2016 Shirah BH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 14487
- [From(publication date): 5-2016 - Aug 29, 2025]
- Breakdown by view type
- HTML page views: 13472
- PDF downloads: 1015