Case Report Open Access
The Isolated Rectal Neurofibroma: A Rare Case Report
Parmar ZB*Department of Radiodiagnosis, Gujarat Cancer and Research Institute, Vejalpur, Ahmedabad, Gujarat, India
- Corresponding Author:
- Zankhana Bipinbhai Parmar
Department of Radiodiagnosis,
Gujarat Cancer and Research Institute,
Vejalpur, Ahmedabad, Gujarat, India
Tel: 9714410058
E-mail: zankhanabparmar@gmail.com
Received Date: October 04, 2016; Accepted Date: November 07, 2016; Published Date: November 11, 2016
Citation: Parmar ZB (2016) The Isolated Rectal Neurofibroma: A Rare Case Report. OMICS J Radiol 5:238. doi: 10.4172/2167-7964.1000238
Copyright: © 2016 Parmar ZB. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Gastrointestinal involvement is noted in up to 25% of patients with neurofibromatosis. Most neurofibromas of the gastrointestinal tract are noted in the stomach and duodenum, the colon can be involved rarely. Most of these occur as a part of colonic involvement in NF1. Solitary neurofibroma of the colon is extremely rare. We present the case of a 13-year-old female having an isolated rectal neurofibroma without any systemic signs and family history of neurofibromatosis; very few numbers of such cases have been reported. The clinical significance of detecting these cases lies in the need of follow-up of these patients as it can be associated with or it can be the initial presentation of neurofibromatosis and there lies a risk of malignant transformation.
Keywords
Neurofibromatosis; Intestinal; Rectal lesion; Neurofibroma
Introduction
Solitary gastrointestinal neurofibroma is a very rare presentation. The clinical manifestations of gastrointestinal neurofibroma vary, being completely asymptomatic to massive lower gastrointestinal bleeding requiring aggressive management. The final diagnosis completely relies on histopathological examination following either surgical resection of the involved bowel or colonoscopic removal of the polyps.
Case Report
A 13-year-old female presented with rectal bleeding. Her medical history was not significant. The patient did not have any significant family history of neurofibromatosis or gastrointestinal malignancies. On physical examination the patient had an average built. There was no tenderness or palpable masses present on abdominal examination. Head, neck, lung, skin, abdominal and neurological examinations were unremarkable. Laboratory data showed a hemoglobin level of 9.3 g/dL, a white blood cell count of 10600/μL, a platelet count of 8,19,000/μL and a serum creatinine of 0.9 mg/dL. Basic metabolic profile, liver function tests, and coagulation profile within normal limits. Hepatitis and HIV serology was negative. MRI pelvis was performed which showed lobulated mass arising from posterior wall of rectum. On colonoscopy up to the caecum, there was a large noduloproliferative mass from 2 cm to 10 cm from anal verge was noted. Biopsy was taken. Microscopically, section shows spindle cell proliferation. Immunohistochemical stains were performed and were suggestive of neurofibroma.
The patient was operated, when a low anterior resection was done. The patient continued to be followed up in our outpatient clinic and has not developed any systemic signs of neurofibromatosis even after 15 months of follow-up.
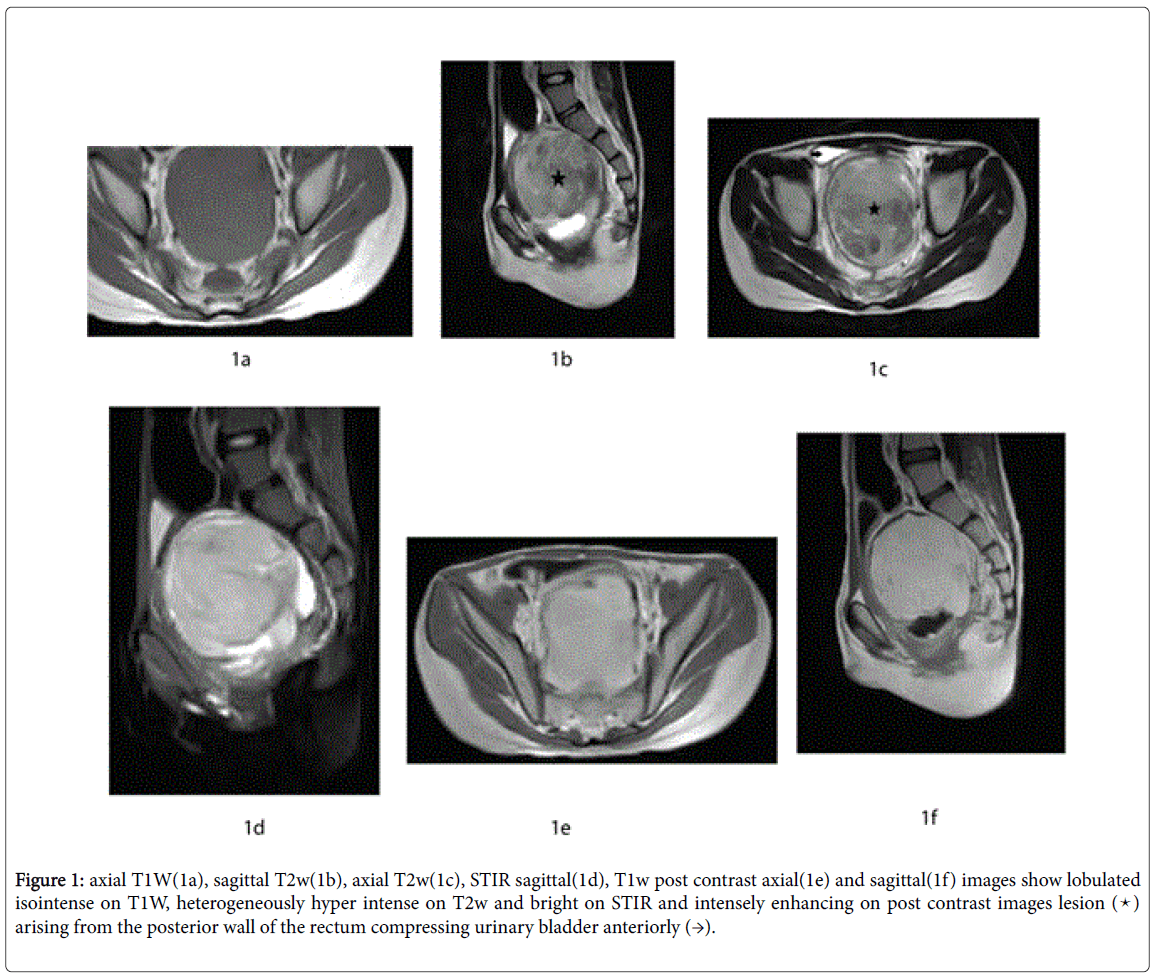
MRI pelvis was suggestive of 72 × 58 × 73 mm sized lobulated altered signal intensity lesion arising from the posterior wall of rectum. The lesion appeared iso intense on T1w, heterogeneously hyper intense on T2w, does not suppress on STIR and showing intense post contrast enhancement. Urinary bladder was compressed anteriorly due to mass effect (Figures 1a–1f).
Figure 1: axial T1W(1a), sagittal T2w(1b), axial T2w(1c), STIR sagittal(1d), T1w post contrast axial(1e) and sagittal(1f) images show lobulated isointense on T1W, heterogeneously hyper intense on T2w and bright on STIR and intensely enhancing on post contrast images lesion (â??) arising from the posterior wall of the rectum compressing urinary bladder anteriorly (→).
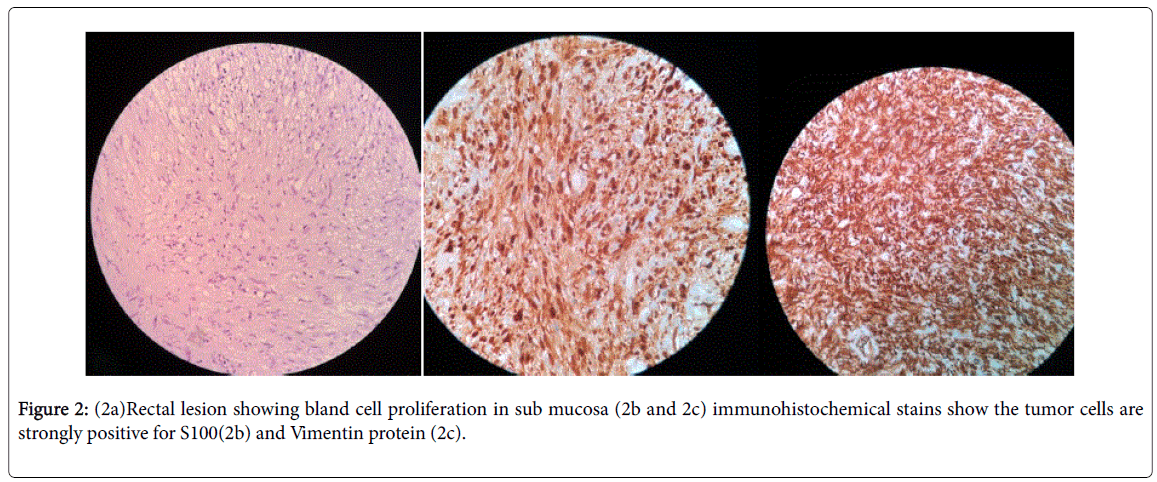
Histopathologically, the noduloproliferative lesion showed bland spindle cell proliferation in the submucosa. Immunohistochemical stains stated that the tumor cells were immunoreactive to S100 and vimentin protein (Figures 2a-2c) and were non-reactive to CD117 and desmin antibodies. These findings were consistent with a diagnosis of rectal submucosal neurofibroma.
Discussion
Neurofibromas are benign neoplasms characterized by the proliferation of neural and connective tissue components of peripheral nerves like Schwann and perineural cells and myofibroblasts. S100 protein immunostaining confirms neurofibromas [1]. The differential diagnosis of neural lesions of the colon comprises of neurofibromas, ganglioneuromas, schwannomas, perineuriomas and granular cell tumors [2]. Neurofibromas can be solitary, multiple or plexiform. They are usually multiple upon presentation and are part of an autosomal dominant hereditary disorder with two clinical entities: neurofibromatosis type 1 (von Recklinghausen neurofibromatosis or peripheral neurofibromatosis; NF1) and neurofibromatosis type 2 (central neurofibromatosis or bilateral acoustic neurofibromatosis; NF2). These disorders have a wide range of clinical manifestations involving the skin, nervous system, eyes, bones, gastrointestinal tract other body parts. Gastrointestinal involvement is uncommon with only 25% of patients with NF1 reported to have gastrointestinal involvement, mostly involving the stomach or small bowel [3].
There are two pathological types of gastrointestinal involvement present; one is ganglioneuromatosis in which hyperplasia and hypertrophy of the nerve plexuses and ganglionic cells in the mucosa, other is neurofibromatosis in which hyperplasia of neuronal cells in the submucosa, muscularis propria or even from the serosa. Gastrointestinal stromal tumors with different degrees of neuronal and smooth muscle differentiation and carcinoid tumors of the periampullary region can be present as associated findings [4-6]. Intestinal neurofibromas generally involve sub mucosa but may extend to the serosa. Diffuse involvement in the form of plexiform neurofibromatosis of the mesentery or retroperitoneal space may cause arterial compression or nerve injury. Although clinical manifestations are non-specific with gastrointestinal neurofibromatosis, some patients may have abdominal pain, constipation, anemia, blood in stool and an abdominal mass. Intestinal or biliary obstruction, ischemic bowel, perforation, intussusception, and mega colon are some serious complications reported. Neurofibromas of the colon are extremely rare and usually, occur in association with NF1. Isolated neurofibromas without any other systemic signs of neurofibromatosis are even rare. There are approximately 10 cases of isolated colon neurofibromas were reported. Most of these cases were female. The age range at diagnosis was 45–70 years. There is a slight predilection for the rectal involvement. Our patient is an example of the same but presents at the age of 13 which is very rare [7]. Sometimes, solitary gastrointestinal neurofibromas may be the initial sign of NF1 in patients without any other clinical manifestations of the disease.
Solitary neurofibromas have also been reported in mesentery [8], the ileum [9], retroperitoneum, the anal canal [10], the oesophagus [11], the soft palate [12], the gallbladder [13] and the common bile duct [14]. These lesions are typically benign, but have an increased risk of malignant transformation, particularly when association with NF1 and in larger, plexiform lesions [15]. Very few cases of isolated colon neurofibroma have been reported. However, close clinical follow-up of these patients is needed as isolated bowel neurofibroma could be the initial sign of neurofibromatosis and its associated risk of malignant transformation.
References
- Korf BR (2013) Neurofibromatosis. Handb Clin Neurol 111: 333-340.
- Gibson JA, Hornick JL (2009) Mucosal Schwann cell ‘hamartoma': a clinicopathologic study of 26 neural colorectal polyps distinct from neurofibromas and mucosal neuromas. Am J Surg Pathol33:781-787.
- Hochberg FH, Dasilva AB, Galdabini J, Richardson EP (1974) Gastrointestinal involvement in von Recklinghausen’s neurofibromatosis. Neurology 24:1144.
- Kim HR, Kim YJ (1998) Neurofibromatosis of the colon and rectum combined with other manifestations of von Recklinghausen’s disease. Dis Colon Rectum41:1187-1192.
- Fuller CE, Williams GT (1991) Gastrointestinal manifestations of type 1 neurofibromatosis. Histopathology19:1-12.
- Gogus S, Sarikayalar F, Akcoren Z, Yalnizoglu D, Hicsonmez A (1997) Intestinal involvement and vasculopathy in von Recklinghausen’s neurofibromatosis. Turk J Pediatr 39: 117-122.
- Chelimilla H, Chandrala CK, Niazi M, Kumbum K ((2013) Incidental finding of isolated colonic neurofibroma. Case Rep Gastroentral 7: 369-375.
- Magro G, Piana M, Venti C, Lacagnina A, Ruggieri M (2000) Solitary neurofibroma of the mesentery: report of a case and review of the literature. Pathol Res Pract196:713-718.
- Watanuki F, Ohwada S, Hosomura Y, Okamura S, Kawashima Y, et al. (1995) Small ileal neurofibroma causing intussusception in a non-neurofibromatosis patient. J Gastroenterol 30: 113-116.
- Frick EJ Jr, Lapos L, Vargas HD (2000) Solitary neurofibroma of the anal canal. Dis Colon Rectum 43:109-112.
- Saitoh K, Nasu M, Kamiyama R, Hatakeyama S, Maruyama M, et al.(1985) Solitary neurofibroma of the esophagus. Pathol Int 35: 527-531.
- Sinha R, Paul R, Sen I, Sikdar B (2002) A solitary huge neurofibroma of the soft palate. J Laryngol Otol 116: 637-638.
- Acebo E, Fernandez FA, Val-Bernal JF (1998) Solitary neurofibroma of the gallbladder-A case report and review of the literature. Gen Diagn Pathol 143: 337-340.
- Carbia S, Pagola J, Flaster N, Guida A, Jufe L, et al. (1994) Isolated neurofibroma of the common bile duct. Medicina 55: 689-692.
- Riddle ND, Gorden L, Rojiani MV, Hakam A, Rojiani AM (2010) CD44 and p53 immunoexpression patterns in NF1 neoplasms - indicators of malignancy and infiltration. Int J Clin Exp Pathol3: 515-521.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 12165
- [From(publication date):
December-2016 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 11288
- PDF downloads : 877