Case Report Open Access
Carcinoma Ex Pleomorphic Adenoma: Rare Malignant Salivary Gland Neoplasm
SandhyaTamgadge, AvinashTamgadge, Treville Pereira* and Simona Naik
Department of Oral & Maxillofacial Pathology and Microbiology Dr D Y Patil Dental College & Hospital, Maharashtra, India
- *Corresponding Author:
- Treville Pereira
Department of Oral & Maxillofacial Pathology
and Microbiology Dr D Y Patil Dental College & Hospital
Sector 7, Nerul, Navi Mumbai, Maharashtra, India
Tel: 919821281458
Fax: 912227709590
E-mail: trevillepereira@gmail. com
Received Date: March 10, 2014; Accepted Date: April 24, 2014; Published Date: May 02, 2014
Citation: Tamgadge S, Tamgadge A, Pereira T, Naik S (2014) Carcinoma Ex Pleomorphic Adenoma: Rare Malignant Salivary Gland Neoplasm. Oral Hyg Health 2: 133. (2014) Carcinoma Ex Pleomorphic Adenoma: Rare Malignant Salivary Gland Neoplasm. J Oral Hyg Health 2:132. doi: 10.4172/2332-0702.1000132
Copyright: © 2014 Sandhya T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
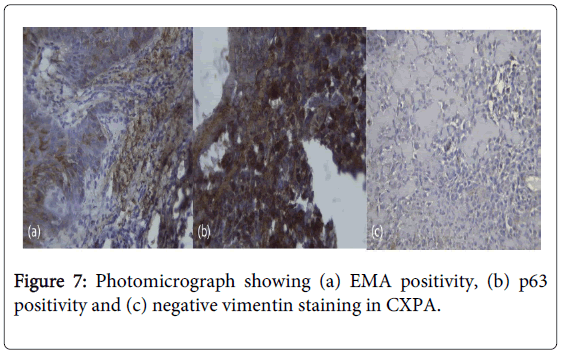
Carcinoma ex-pleomorphic adenoma (CXPA) is a rare, aggressive, poorly understood malignancy of the salivary gland. The clinical findings typical of this tumor include history of a slow growing, ulcerated, painless mass that enlarges rapidly. Histologically, CXPA is characterized by the presence of carcinomatous transformation in pleomorphic adenoma which includes abnormal nuclear changes with mitoses, dystrophic calcification, vascular or neural invasion or both by lesional cells along with local and distant metastasis. Immunohistochemical staining in the carcinoma areas revealed positive reaction for epithelial membrane antigen and p63 protein but negative for vimentin. We report a case of a CXPA in the hard palate and discuss its clinical and histopathological findings.
Keywords
Pleomorphic adenoma; Carcinoma ex pleomorphic adenoma; Malignancy; Mitosis; Invasion
Introduction
Pleomorphic adenoma (PA) is the most common neoplasm of salivary glandsand may sometimes undergo malignant transformation in its natural course. Carcinoma ex pleomorphic adenoma (CXPA) is considered to be a malignant transformation product of a pre-existing pleomorphic adenoma [1]. Carcinoma ex pleomorphic adenoma was first described by Beahrs et al. in 1957. It accounts for 3. 6% of all salivary gland neoplasms and for 11.7% of salivary malignancies. Less than 7% of the cases occur in the palatal minor salivary glands. About 30% of patients present signs and symptoms including pain, facial nerve palsy, enlarged lymph nodes, skin ulceration and dysphasia. CXPA usually occurs in the 6th-8th decades of life [2]. Surgery, radiotherapy, chemotherapyis the treatment of choice. We present here a case of CXPA affecting a 40-year-old female patient of short duration and poor prognosis.
Case Report
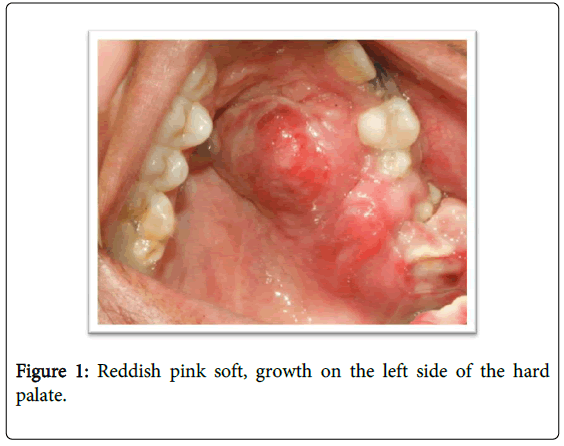
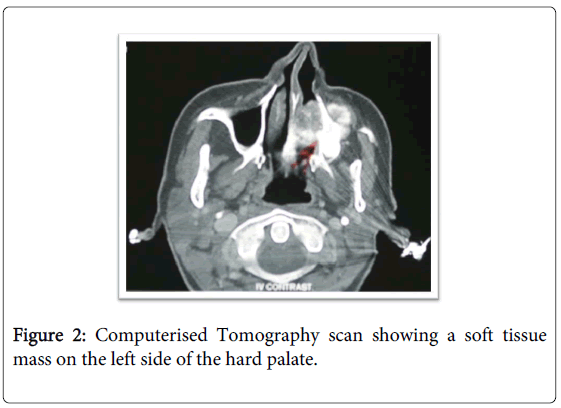
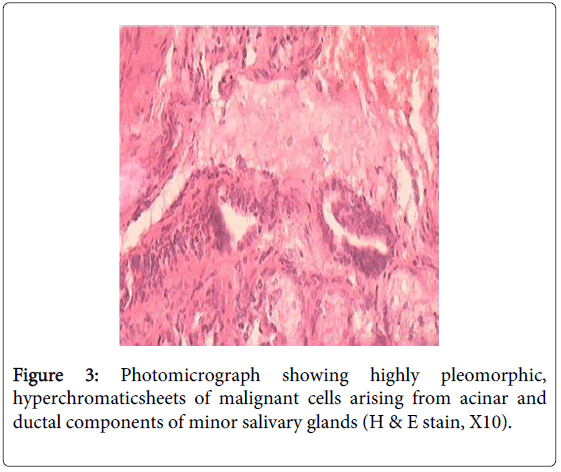
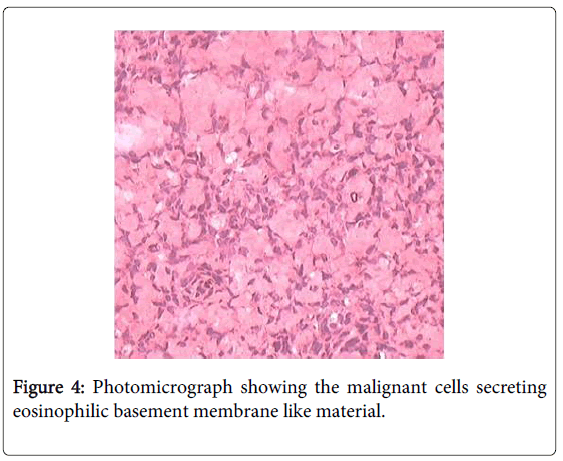
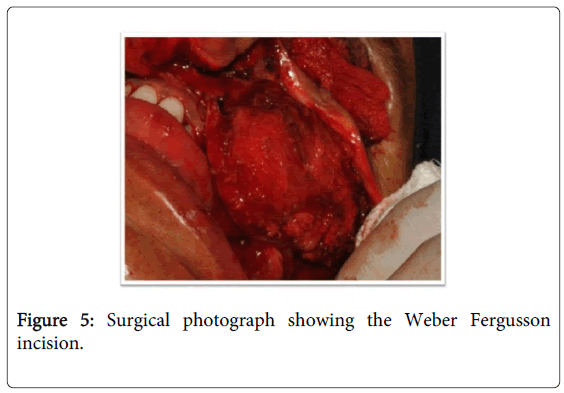
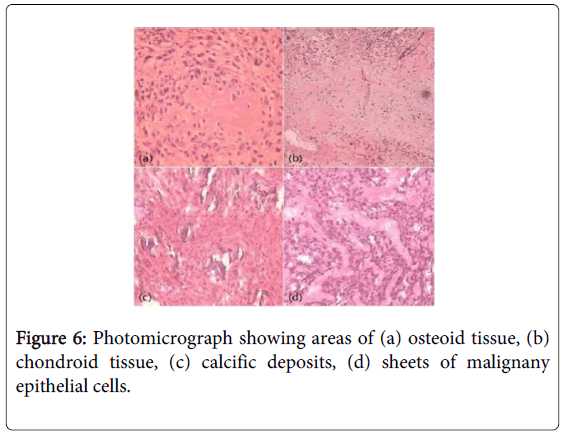
A 40-year-old female reported to our institute with a chief complaint of a swelling in the left maxillary region. Intraoral examination revealed reddish pink soft, growth in the palatal region since 2 months. It measured around 5×4 cm in size. It was a rapidly growing lesion with the patient complaining of difficulty in mastication and swallowing (Figure 1). Computerized tomography showed the presence of a soft tissue mass on the left side of the hard palate (Figure 2). Based on clinical and radiographic examination provisional diagnosis of an osteosarcoma or a neoplasm of minor salivary gland of the palate was hypothesized. An incisional biopsy was performed under local anesthesia. Histopathologically, the specimen demonstrated highly pleomorphic, hyperchromatic sheets of malignant cells arising from acinar and ductal components of minor salivary glands (Figure 3). These malignant cells were secreting eosinophilic basement membrane like material (Figure 4). These secretions were similar to the secretions by myoepithelial cells in a pleomorphic adenoma suggesting that these cells were malignant transformation of myoepithelal cells. As per traditional approach, maxillectomy was done. The Weber Fergusson incision was taken and a full thickness skin graft from left thigh was repositioned on the raw area (Figure 5). Excisional biopsy of the specimen showed areas of myxoid like material, condroid like and scanty osteoid like component surrounded by highly pleomorphic and hyperchromatic sheets of malignant cells (Figure 6). On higher magnification cells were showing abnormal mitotic figures indicating high proliferative growth. Few areas showing dystrophic calcifications and vascular invasion were also observed. Immunohistochemical staining was done using epithelial membrane antigen, p63 protein and vimentin. The tumor cells were positive for epithelial membrane antigen and p63 protein but were negative for vimentin (Figure 7). Based on these results, diagnosis of carcinoma ex-pleomorphic adenoma was given.
Discussion
Carcinomaex pleomorphic adenoma is a tumor in which the neoplasm develops from the epithelial component that fulfils the criteria for malignancy [3]. In most instances, 75% of the luminal epithelial cells undergo malignant change. In 19% of cases, a dual epithelial/myoepithelial differentiated carcinoma is seen. Pure myoepithelial malignant change is seen in only 6% of cases [2]. The scarcity of well documented cases and lack of generally accepted histopathologic criteria has led to poor understanding of this form of salivary gland cancer [3]. To satisfy the definition of CXPA, at least a focus of benign pleomorphic adenoma must be identified or a previous benign pleomorphic adenoma must have been excised from a site in which recurrent tumoris carcinomatous [4]. The proposed criteria for defining carcinoma ex pleomorphic adenoma by Nagao et al. were used to select and reclassify our case of carcinoma ex pleomorphic adenoma. The use of strict pathological criteria may underestimate the frequency of carcinoma ex pleomorphic adenoma because the malignant cells in some cases may obliterate the original pleomorphic adenoma [5].
CXPA usually presents clinically with a history of a slowly growing, painless mass that suddenly or over a short period enlarges rapidly. It presents with signs and symptoms suggesting malignancy (e. g. Fixation to surrounding structures, occasional pain, skin infiltration, trismus, facial nerve weakness, or palsy). Facial nerve weakness or palsy has been detected in approximately 23-40% of cases [6]. In the present case the patient complained of pain and difficult in mastication. These are clinically aggressive lesions often leading to metastasis and a tumor related death [5]. Beahrs et al. reported the predominance of males whereas Evans and Cruickshank showed that CXPA are more common in the females. Chen HH et al. showed that CXPA is the most common malignant change in PA. CXPA arising in the palate is rare. Waldron et al. reported only four cases of CXPA out of 181 palatal tumors. Da-Quan and Guangyan also reported 19 cases out of 160 cases, but Regezi et al. failed to report any case out of the 109 cases [3]. Nagao et al showed that 50% of the CXPA of the parotid gland were greater than 5 cm in size. On the other hand, Livilsi and Perzin stated that this tumor, arising in a minor salivary gland, is smaller than that arising in a major salivary gland. In the palate, the neoplasm tended to be more small (75% were 2 cm or less) [7]. However the tumor size in the present case was large measuring 4×5 cms in dimension and affecting a female patient.
According to the World Health Organization histological classification published in 2005, malignant changes in the pleomorphic adenoma include three different types: CXPA, carcinosarcoma, and metastasizing PA [2]. Among these types of adenoma, CXPA is the most commonly encountered [1]. In agreement with Cawson and Eveson’s concept, and according to the diagnostic criterias proposed by Gerughty et al. [3], we think that our case is a carcinomatous transformation in pleomorphic adenoma. Our case had all the features of carcinomatous transformation along with local metastasis. Immunohistochemistry was believed to be of potential assistance in the diagnosis of salivary gland tumors and in the prediction of histogenesis. In our case immunohistochemical staining in carcinoma areas showed positive reaction for epithelial membrane antigen and p63 and a negative reaction for vimentin.
Possible treatments of carcinoma ex pleomorphic adenoma include four different modalities; surgical therapy, radiotherapy, chemotherapy and combined therapy. According to Chen et al., surgery followed by postoperative radiation should be considered the standard of care for patients with CXPA [8]. Livolsi and Perzin, stated that lesions of the palate had better prognosis as compared to tumors of the major salivary glands, perhaps because of their relatively small size when discovered clinically [9]. Because the number of cases is very small, there is no distinct tendency as to the rate of recurrence and rate of formation of metastasis. Gerughtyet al. suggested that the histological evidence of an invasive growth pattern, neural or vascular invasion, necrosis and focal calcification implied a poor prognosis [9]. In the present case the tumor was surgically removed followed by radiotherapy.
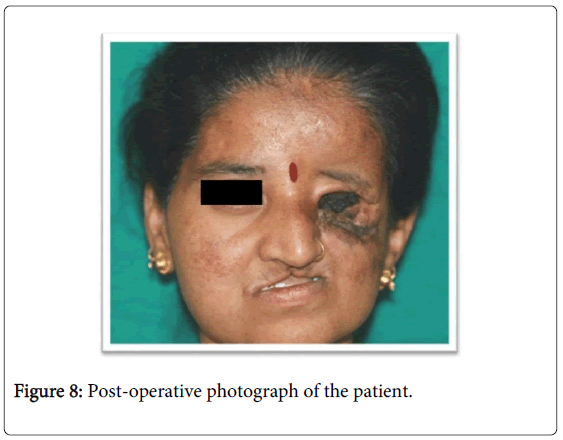
The present case had an aggressive clinical course (Figure 8). Disease control was achieved with surgery and postoperative radiotherapy. However the patient was lost to follow up due to its aggressive clinical course.
References
- Tarakji B, Kujan O, Nassani MZ (2010) Immunohistochemical Expression of p53 in Pleomorphic Adenoma and Carcinoma Ex Pleomorphic Adenoma. J Cancer Epidemiol 2010: 250606.
- Chen HH, Lee LY, Chin SC, Chen IH, Liao CT, et al. (2010) Carcinoma ex pleomorphic adenoma of soft palate with cavernous sinus invasion. World J SurgOncol 8: 24.
- Kim KM, Lee A, Yoon SH, Kang JH, Shim SI (1997) Carcinoma ex pleomorphic adenoma of the palate--a case report. J Korean Med Sci 12: 63-66.
- Etit D, Tan A, Bayol U, Altinel D, Cumurcu S, et al. (2010) Oncocytic carcinoma ex pleomorphic adenoma. Head Neck Pathol 4: 49-52.
- Tamiolakis D, Chimona TS, Georgiou G, Proimos E, Nikolaidou S, et al. (2009) Accessory parotid gland carcinoma ex pleomorphic adenoma. Case study diagnosed by fine needle aspiration, Stomatologija, Baltic Dental and Maxillofacial 11: 37-40.
- Ide F, Mishima K, Yamada H, Saito I (2009) Adenoid cystic carcinoma ex pleomorphic adenoma of the parotid gland. Head Neck Pathol 3: 159-162.
- Fowler MH, Fowler J, Ducatman B, Barnes L, Hunt JL (2006) Malignant mixed tumors of the salivary gland: a study of loss of heterozygosity in tumor suppressor genes. Mod Pathol 19: 350-355.
- Freitas LL, Araújo VC, Martins MT, Chone C, Crespo A, et al. (2005) Biomarker analysis in carcinoma ex pleomorphic adenoma at an early phase of carcinomatous transformation. Int J SurgPathol 13: 337-342.
- Hemplemann LH, Womack NA (1942) The Pathogenesis Of Mixed Tumors of the Salivary Gland Type. Ann Surg 116: 34-42.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 19886
- [From(publication date):
July-2014 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 14985
- PDF downloads : 4901