Research Article Open Access
Four Decades of Bariatric Surgery in a Community Hospital of Spain
Baltasar A*, Bou R, Bengochea M, Serra C, Pérez N, Arlandis F, Martínez R and Cipagauta LVirgen de los Lirios Hospital and San Jorge Clinic, Alcoy, Spain
- Corresponding Author:
- Aniceto Baltasar, MD
Virgen de los Lirios Hospital and San Jorge Clinic
Cid 61, 03803-Alcoy, Alicante. Spain
Tel: +34-965.332.536
E-mail: baltasarani@gmail.com
Received Date: January 06, 2017; Accepted Date: January 23, 2017; Published Date: January 27, 2017
Citation: Baltasar A, Bou R, Bengochea M, Serra C, Pérez N, et al. (2017) Four Decades of Bariatric Surgery in a Community Hospital of Spain. J Obes Weight Loss Ther 7:331. doi:10.4172/2165-7904.1000331
Copyright: © 2017 Baltasar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
Introduction: Bariatric surgical practice changes in the community setting may be under-reported. We present the developments in a Spanish bariatric surgical practice in the community setting of Alcoy from its origin in 1977 through the present.
Methods: Bariatric surgical techniques employed in a country community setting over the course of nearly four decades were reviewed retrospectively and qualitatively.
Results: Surgeons and medical professionals from Alcoy, Spain were involved in the evolution of bariatric surgery patient management and surgical technique from 1977s through 2017. During the last 40 years, 1,475 patients were treated in our clinics. Spanish bariatric surgeons contributed to advances in gastric bypass in the 1970s, vertical banded gastroplasty in the 1980s, bilio-pancreatic diversion/duodenal switch in the 1990s, and innovations associated with laparoscopy from the 1990s onward. Outcomes and approaches to prevention and treatment of bariatric surgical complications are reviewed from a community perspective. Contributions to the bariatric surgical nomenclature and weight-loss reporting are noted.
Conclusions: The practice of bariatric surgery in the community setting must be updated continuously, as in any human and surgical endeavor. Medical professionals in community bariatric practices should contribute their experiences to the field through all avenues of scientific interaction and publication.
Keywords
Obesity surgery; Bariatric surgery; Community setting; Trends
Abbreviation
1eu: 1st in Europe; 1sp: 1st in Spain; 1w: 1st in the world; AL: Alimentary Limb; ABS: Adolescent Bariatric Surgery; ASBS: American Society for Bariatric Surgery; ASMBS: American Society for Metabolic and Bariatric Surgery; BS: Bariatric Surgery; BMI: Body Mass Index=kg/m2; AEC: Asociación Española de Cirujanos; BOLD: Bariatric Outcomes Longitudinal Data; BPD: Biliopancreatic Diversion; BPD/DS: BPD/Duodenal Switch; BPL: Biliopancreatic Limb; CC: Common Channel; CPM: Caloric-Protein Malnutrition; DIA: Duodenoileal Anastomosis; DS: Duodenal Switch; ExBMI: Expected BMI; ECEP: European Centers of Excellence Program; EGJ: Esophago-Gastric Junction; FBMI: Final BMI; GBP: GASTRIC BYPASS; GERD: Gastroesophageal Reflux; GGF: Gastro-Gastric Fistula; GT: Gastric Tube; IFSO: International Federation for the Surgery of Obesity and Metabolic Disorders; IBMI: Initial BMI; JIB: Jejunum Ileal Bypass; JIA: Jejunum-Ileum Anastomosis; LDS: Laparoscopic Duodenal Switch; LGB: Laparoscopic Gastric Band; LGBP: Laparoscopic Gastric Bypass; MO: Morbidly Obese; ECEP: Eur. Centers of Excellence Program; PE: Pulmonary Embolus; REEADL: Revista Española de Enfermedades del Aparato Digestivo; RNY: Rouxen- Y; SADI: Single Anastomosis Duodeno-Ileum; SG: Sleeve Gastrectomy; SFG: Sleeve-Forming Gastrectomy; SECO: Sociedad Española de Cirugía Obesidad; VBG: Vertical Banded Gastroplasty; VLG: Vertical laparoscopic gastrectomy; WL: Weight loss; %BMIL: %BMI Loss; %EBMIL: %Excess BMI Loss; %EWL: %Excess Weight Loss
Introduction
Morbid obesity is a pandemic condition that affects humans of all countries, races and continents. The cause is multifactorial and one the most influential factors are changes in environment and lifestyle that support consumption by humans of more calories than they utilize. When BS is employed to treat the disease of obesity, the stomach and small bowel, organs of the digestive pathway are healthy, and not the direct cause of disease. The term, BS, comes from the Greek "baros," meaning “weight," and “iatrein," meaning “treatment”—treatment of the broad etiology of obesity through surgery. In order to influence the weight of a patient, a bariatric surgeon can operate on the stomach to reduce caloric intake (restriction), and/or on the small bowel, to cause malabsorption of nutrients by shortening the length of the intestine (without any bowel removal). In mixed techniques, restrictive and malabsorptive components are combined. The term, "metabolic surgery” (MS) represents an expansion of the concept of BS to reflect its management of metabolic conditions, such as hypercholesterolemia or diabetes.
1950s—origins of BS/MS
Henriksson [1] performed the first, isolated, JIB in Gothenburg, Sweden in 1952 but BS field was actually initiated in 1953 at the University of Minnesota by two groups, Varco and Buchwald and Kremen and Linner [2].
During the latter half of the 20th century, Payne [3] and other surgeons were performing malabsorptive operations. In 1964, Buchwald inaugurated MS by diverting the distal one-third of the small bowel to treat hypercholesterolemia [4,5]. Edward Mason initiated the technique of the GBP in 1965 [6].
Methods
This is a review article of the surgical changes made in a four decades period in the practice of bariatric surgery in a community hospital of Spain.
Setting
Alcoy County is located in the Alicante province of Southeastern Spain, close to the Mediterranean Sea. The population of the city is 60,000, and the county community, 140,000. Alcoy has a 300-bed National Health Service (NHS) state of the art facility, the Virgen de los Lirios district hospital, which includes an intensive care unit and operating room with three-dimensional camera laparoscopic facilities, computerized tomography and radio magnetic scans, a blood bank, standard and interventional radiology, an explant transplantation center, and a smaller private institution, the San Jorge Clinic. All patients referred to in the studies summarized were treated by the same primary surgical staff.
Results
Development of bariatric surgery in Alcoy, Spain
1970s—beginnings of BS in Alcoy
On June 19, 1977, we initiated the 1sp GBP in Spain, performed as recommended by Dr. Mason [6] in 18 patients, an experience not published until 1980 [7]. Much later, in 2013 [8], we learned that Prof. Garcia of Seville (already deceased) had performed the 1sp malabsorptive JIB [9-12] in 1973 as recommended by Scott [13].
1980s and 1990s —vertical banded gastroplasty
Mason [14], in 1982, published his paper on the 1w VBG. In 1986, we published our first experiences with VBG using staplers [15]. Dr. Andreo, our radiologist, published a description of the VBG "peanut deformity" [16]. Gastro-gastric fistula (GGF), a communication between the gastric pouch and the gastric fundus, was the main undesirable complication of the VBG. Five of our first 10 patients had this complication. While not life-threatening, the complication destroyed the intended restriction of the operation. Therefore, in 1988, our group devised the "vertical division with linear stapler and stapleline suture", separating both staple-lines with a continuous serosal suture [17]. The technique was presented in Milan, Italy in the 1st World 1988 Surgical Week that won the Best Poster Award. We operated on 130 patients with this technique without a single GGF. McLean et al. in 1993 published later the same technique [18].
We reported our high expectations of VBG [19] and reviewed the same patients 5 years later, commenting that “the VBG... was a frustrating experience" [20,21]. Less than 2 years later, VBG disappeared from the bariatric armamentarium.
On September 25, 1995, we assisted Dr. Favretti [22] of Italy in performing the 1sp LGB in Spain at the Hospital La Paz, in Madrid. However, early on we abandoned use of the technique. LGB became less and less popular, first in Europe and then in the world.
Baltasar et al. [23] published in 1987 the 1sp surgery for hypercholesterolemia done in Spain by diversion of the distal one-third of the small bowel, this is the 1sp Spanish publication on MS. The operation has been abandoned with the use of statins.
1990s—duodenal switch
On March 17, 1994, we performed the 1sp open DS in Spain. Our open DS series has 527 patients (5 deaths, 0.9% mortality) [24-26]. At the ASBS meeting in Seattle in June 1995, we presented a video depicting the full vertical gastrectomy division and suturing of the staple line. Dr. Hess [27], saw the video and began using the continuous suture, noting that, "after seeing a video of Baltasar at the annual meeting of the ASBS, we modified our procedure for the subsequent 188 cases and had only a leak". A continuous running serosal suture of the staple line prevents leaks that may occur after SG (the first part of the DS). Dr. Hess performed the 1w DS in 1988 and Dr. Marceau [28] started on June 1990 and made the 1w publication in 1993 and both ought to be considered the "fathers of DS”.
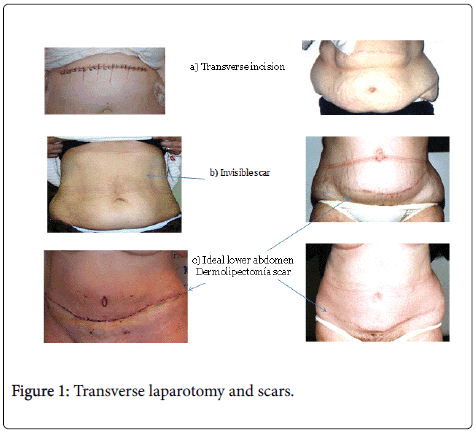
A second contribution of our DS video was the use of the transverse supraumbilical abdominal incision (Figure 1a). This approach resulted in fewer incisional hernias, 10%, compared with the midline laparotomy incision (hernia rates of 31% to 39%). The transverse incision has 2 other advantages. One is a cosmetic: When patients lose weight, the size of the abdominal scar is reduced to less than one-third of that achieved with the laparotomic approach (Figure 1b). The second benefit is that the transverse incision facilitates post-bariatric plastic surgery, as transpositions of the navel are readily performed with a single scar just above the pubis (Figure 1c). Our group later published an intermediate study on the DS [29] followed by comparative studies of VBG and DS [30].
In 1990, the ASBS started Obesity Surgery, as their official medium for reporting scholarly research and was included into the Index Medicus in 1995. This is a major accomplishment and recognition, and then became the journal of IFSO. AB entered into ASBS membership in 1997 and IFSO in 1998 and served on the ASBS Standards Committee under the chair of George Cown 1998-2004.
In addition to their contribution to BS by directing Obesity Surgery, Drs. Mervyn Deitel and George Cowan published three books and were very influential as surgeons and book publishers [31-34]. Deitel’s acclaimed 1989 book inspired AB to specialize in bariatric surgery field [31].
Mid-1990s—laparoscopic BS and SECO
Wittgrove and Clark [35-37] lead the transition from laparotomic to laparoscopic BS. We were impressed by their 1993 1w RNY LGBP experience. In early 1996, they published their second paper. In the summer of 1996, AB was asked to review their third paper for Obesity Surgery, which summarized outcomes in 75 patients [37]. AB visited them in San Diego and they told him that he was the 1w visiting surgeons to do so.
Our group in Alcoy performed the 1eu LGBP on January 14, 1997, and reported it in the second SECO meeting in December, 1998, and then published the results of 16 cases [38]. At the 1998-IFSO Bruges, Belgium meeting, there were only 2 surgical films on LGBP, one from Sweden by Gustavsson [39], and our own [40]; these perhaps represented the 1eu 2 reports on LGBP outside of the US. In them, we concluded somewhat presciently that it was “a beautifully designed operation, with a very difficult learning curve but that probably will become the gold standard of bariatric surgery.”
Serra [41], in 1999, reported the 1w case of internal hernia after LGBP, which was cited by Higa et al. [42]. Baltasar [43] reported the 1sp 27 LGBP cases and received the 2000 Spanish National Surgical Award.
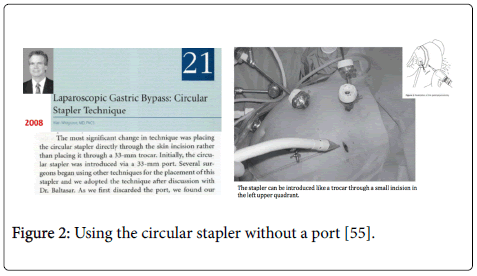
Whereas, in the initial Wittgrove technique, a #33 port was used to introduce the stem of the circular stapler, AB suggested using the stapler without a port (Figure 2).
Later, Dr. Wittgrove [44] acknowledged that this was a feasible and practical approach and became the accepted standard technique (Figure 3).
Spanish society for the surgery of obesity (SECO)
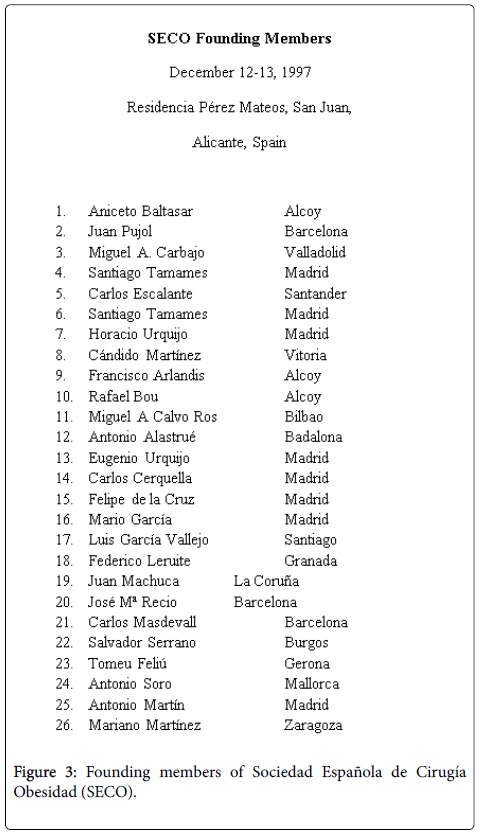
Our group founded SECO with 26 members in Alicante, Spain (Figure 3) in December 1997. During the inaugural meeting, AB became the 1sp President. The second meeting was held in Granada in 1998 with Drs. Capella and Álvarez Cordero as our first honorary members. In the following year, SECO became the 13th IFSO member society. SECO was accepted into the Spanish Surgical Society in 2002, and AB was made SECO Honorary President. While AB was President of IFSO and SECO, we organized the VIII World Congress of IFSO-2003 and the 1st Ibero-American meetings in Salamanca. By 2004, SECO had the second highest number of publications in Obesity Surgery after the US, and continued to hold that position in 2005, 2006, and 2007, and held the third position in 2009.
SECO has been proved to employ an effective operational structure. It has had 7 presidents, with that role changing every 2 years. SECO has created sub-brands, e.g., Fun-SECO, Campus-SECO, and Multidisciplinary-SECO. Each of these groups’ respective activities and information are readily accessed through its website (http://www.seco.org/). SECO now has 420 members and several honorary members who rank among the most distinguished bariatric surgeons in the world.
Our group’s members have operated as invited surgeons in Portugal (1997, 1st VBG; 2001, 1st DS; 2005, 1st SG); in Brazil (1998, Sao Paulo, 1er DS; 2004, Itajai, 2nd LDS); in Buenos Aires, Argentina (2002, 1st LGBP), in Ahmedabad, India (2005, 2nd LDS), in Jerusalem, Israel (2008, 1er LDS), and in Norway (2002, Forde, 1er LDS; 2002, Tonsberg, 2nd LSG). We have also been guest surgeons in several national hospitals and a guest speaker in 2003 at the 1st ACS Meeting, the 1st ASBS Meeting in New York, and the 1st Fall meeting of ACS-ASBS in Chicago. We have also had the privilege of hosting 71 visiting guest surgeons who have traveled to Alcoy, Spain to learn LDS and LSG.
IFSO has recently appointed Dr. Antonio Torres, a past President of SECO, as Organizer, and Dr. Baltasar, as Honorary President, of the upcoming Annual IFSO-2019 Congress in Madrid. Spain is the third country (after Austria and Brazil) to organize 2 world conferences, and the second country with 2 IFSO presidents.
Early 2000s—laparoscopic duodenal switch
Our group was present in 1999 when Gagner performed the 1sp LDS in Terrassa, Spain, even before he and Ren [45] described it in 2000 as the most complex BS technique. We performed our 1sp LDS on October 5, 2000 [46-49]; Weiner et al. [50] considered it to be the 1eu LDS performed in Europe. We have done 413 LDS cases (2 deaths, 0.48%). Our LDS is performed by 3 surgeons using 6 ports (one #12 single “working” in the right upper quadrant port, one #10 port for the camera, and 4 5-mm working ports). All bowel divisions are accomplished with staplers and all anastomosis are hand sewn.
In 2000, we published the 1sp book in Spanish on BS, “Obesidad y Cirugía” (Obesity and Surgery) with 2 editions [51]. The book was intended for the general public but was also widely read by Spanish medical professionals.
In 2005, SOARD, a journal on par with Obesity Surgery in the BS field, published its first volume. During these years, our publications described gastric emptying after DS [52], as well as pancreatocutaneous fistula [53], cardiac tamponade by central catheter [54], hepatic impairment [55,56], liver failure and transplant [57], total gastrectomy [58], and different types of DS reversal [59]. Thirty patients (3.2%) of the 923 DS patients studied underwent a bowel lengthening for malnutrition. We also described [60] the 1w occurrence of mucosal jejunum wall hernias through the thin muscular bowel wall of patients with malnutrition and suggested that, in malnutrition, laparotomy may be safer than laparoscopy. We performed laparoscopic conversions from RNY to BPD as a successful and fairly easy therapy [61].
Mid-2000s—laparoscopic sleeve gastrectomy and other innovations
We completed our 1sp LSG on December 12, 2002 and reported it 2005 [62]. Ahmad et al. [63] recently ranked this paper’s citation index 61st within BS. We published additional papers on LSG [64,65] and the performance of one of the 1w re-sleeves gastrectomies [66].
Prevention, detection, and management of LSG leaks and fistulas at the EGJ have been a main concern for our group. At the IFSO-2000 meeting in Genoa, Italy we presented our use of the 1w non-removable stent [67]. At that time removable-ones were not available, and so we used a non-removable Wall-stent that saved the patient's life and that lasted 6 months until esophageal hypertrophy of the mucosa caused obstruction of the esophagus requiring a total gastrectomy with intrathoracic anastomosis [58]. Serra et al. published our experience in selfexpanding stents [68].
We performed LSG on 342 patients. Three of them experienced bleeding, 3 required an emergency intra-operative tracheotomy due to impossible intubation [69], and there were 3 EGJ leaks, and 2 deaths (0.6%) (one due to bleeding on the abdominal port and the second for EGJ leak). The entire LSG group had 93% EWL at 2 years, probably due to the systematic use of the very narrow sleeves and antrectomy, and to beginning the gastric stapling right at the pylorus [70].
Salvage surgery for chronic EGJ fistulas
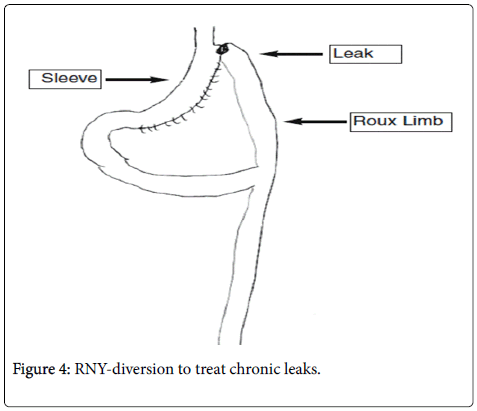
In 2007 we used the 1w RNY diversion to correct chronic EGJ fistulas [71-73] and presented it for discussion at the 2nd and 3rd world LSG summits organized by Gagner et al. and Deitel et al. [74,75]. This has become the standard management of this serious condition (Figure 4).
Diabetes surgery
On February 10, 2004 we performed [76] the 1sp diabetes surgery in Spain in a non-morbidly obese individual (BMI of 33 kg/m2) using the DS without gastrectomy; this technique was later reported in 2014 by Marceau et al. [77]. Bou et al. published our technique of SG with duodenal-jejunum diversion (SG+DJD) for diabetes [78].
In 2006, we published a report of our 1,000 bariatric operations [79], which won the Spanish National Surgical Award.
Adolescent BS
A 10 year-old wheelchair-bound boy with a BMI of 42 kg/m2, Blount´s disease, and knee fractures underwent LSG in 2008 [80]. The patient was the 1sp ABS done in Spain, and one of the world youngest BS patients at the time. He is doing very well nine years later, and has no impairment in his growth with a BMI of 25.7 kg/m2.
European centers of excellence program
In 2009, Drs. Scopinaro, Melissas, Fried, and Baltasar created the IFSO European Chapter of the Centers of Excellence (COE) Program [81]. Multiple European centers and surgeons utilize this program currently.
2010s—Publications and technical improvements
BMI-Latina (Bariatric and Metabolic Ibero-Americana) was founded by us in 2011 as online journal published in Spanish, English, and Portuguese. The magazine was adopted by SECO in 2015 as the Spanish society’s magazine and we believe it will play a valuable role in BS in the Spanish and Portuguese speaking societies since from 2015 only the abstracts of the English edition are published currently [82-85].
Recently, Serra et al. [86] recommended 2 new technical improvements in SG, including the “sliding self-locking stitch” and the Aberdeen knot. Also, in Baltasar et al., we have described our recommendation of antrectomy starting at the pylorus plus an omental patch to cover the staple line and prevent rotation of the sleeve [87]. We also called attention to the need to prevent stapling of the bougie [88] as well as a simple bariatric telemedicine solution to detect early complications after hospital discharge [89].
By 2013, Spain was the country with the fifth most publications in SOARD. Now, in 2017, our group has 119 total BS publications; we have reviewed >74 papers for Obesity Surgery, and >14 for SOARD, and several for other national and international journals. At the IFSO 2009 meeting in Paris, Dr. Baltasar was recognized with the IFSO Lifetime Membership Award. On June 2011, at the ASMBS meeting in Orlando, Florida, Dr. Baltasar was a finalist for the prestigious ASMBS Outstanding Achievement Award.
Discussion
In addition to participating in the aforementioned technical changes in the BS field, our Alcoy practice has contributed commentary on key concepts in the BS nomenclature and on reporting weight loss [90].
Nomenclature
BS is a relatively new specialty. We have long been interested in the development of BS nomenclature [91-93]; our group, under the direction of the Royal Spanish Academy of Medicine, agreed that the correct name in Spanish for the SG technique is "vertical laparoscopic gastrectomy" (VLG) [94], and also, that the end result of the SG/VLG should be termed the formation of a "gastric tube,” or “sleeve"—and so it was approved in the General Assembly of the 2010 SECO meeting in Valencia.
We also published that the English term, "sleeve gastrectomy" is an inappropriate term [95] as the meaning of “gastrectomy” is "amputation and elimination" of any part of the stomach. As right colectomy means the elimination of the right colon, not the left, and a left nephrectomy is the removal of the left and not the right kidney, the use of the term SG should more precisely mean "withdrawal of the sleeve," although, in fact, the sleeve is not removed, it is the sleeve portion of the stomach that remains. Therefore, we have suggested that the SG name is a misnomer [95] and the correct term might be “sleeveforming gastrectomy” (SFG), meaning more precisely a gastrectomy that forms a sleeve [96]. While recognizing that the term, “sleeve gastrectomy” is so ingrained in common usage that it will likely prevail. Surgeons, besides performing excellent procedures, should also aim to speak and write correctly.
Weight-loss reporting
Weight-loss reporting is also controversial in BS. We have suggested that BMI measurement is much better than using WL measurement since it takes into account a patient’s height [97,98]. We should not expect all patients with such different IBMIs to reach an FBMI close to the ideal BMI of 25 kg/m2. This is even more the case for high IBMI patients. Dr. Borrás, our group’s mathematician, devised a mathematical system to measure the “expected BMI”=ExBMI=goal BMI, by using 7,410 real patients from multiple centers [99]. The ExBMI mathematical formula for each patient is FBMI= IBMI × 0.4+12. By using the BOLD system with a large patient sample, it will be possible to apply a better final mathematical formula using the concept of ExBMI. Using the ideal %ExBMI of 100%, any FBMI above that may be considered a success, and that below, a failure. Grading of the results depends on the extent of the deviation. A preliminary report of WL in our DS cases shows that at 5, 10, and 15 years, BMIL of 85%, and an ExBMI of 96% suggest that almost all patients had an FBMI close to the goal results. Molina has recently confirmed these results [100].
Conclusion
For the past 4 decades, from our community practice setting, we have followed the changes in the practice of BS throughout the world and participated in the evolution of the field. It has been extremely important and satisfying to continuously share and discuss evidence with our peers through the scientific literature, and in person, in local, national, and international interactions and meetings. We believe that small institutions can provide high-quality bariatric surgical care to patients and make significant scientific contributions to the field.
Acknowledgments
We would like to thank the editors and all the cited colleagues in this paper for their enormous help, and for the pleasure we have received in meeting and coming to know them all, and also to learn from their excellent teachings.
Ethical Approval
All procedures involving human participants were performed in the studies cited herein in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration and amendments.
Informed Consent
Informed consent was obtained from all individual participants included in the studies cited.
Conflict of Interest
None of the authors has any conflicts of interest to disclose. J. N. Buchwald, Medwrite Medical Communications, WI, USA, received a fee for substantive manuscript revision.
References
- Henrikson V (1952) Is small bowel resection justified as treatment for obesity? Nordisk Medicin 47: 744.
- Linner JH (1987) Overview of surgical techniques for the treatment of morbid obesity. Gastroenterol Clin North Am 16: 253-272.
- Payne JH, Dewind LT, Commons RR (1963) Metabolic observations in patients with jejunocolic shunts. Am J Surg 106: 273-289.
- Buchwald H (1964) Lowering of the cholesterol absorption and blood levels by ileal exclusion. Experimental basis and preliminary clinical report. Circulation. 29: 711-750.
- Shikora SS (2016) Biography: Henry Buchwald. Obes Surg 26: 3-4.
- Mason EE, Ito C (1967) Gastric bypass in obesity. Surg Clin North Am 47: 1345-1352.
- Baltasar A, Río JD, Bengochea M (1980) Gastric bypass in morbid obesity. Rev Clín Española 157: 395-399.
- Baltasar A, Adame ED (2013) Beginnings of bariatric and metabolic surgery in Spain. Cir Esp 91: 413-416.
- Diaz SG, Fernandez SG (1981) Medical and surgical indications for treatment of morbid obesity. World J Surg 5: 795-799.
- García S, Pera C, Loscertales J, Arévalo E (1977) Current state of obesity surgery. REEAD 51: 1-25.
- García S, Pera C, Loscertales J, Arévalo JE (1979) Obesity Surgery. Advances Cirugía 2: 209-224.
- Diaz SG, Fernandez SG (1981) Medical and surgical indications for treatment of morbid obesity. World J Surg 5: 795-799.
- Scott H, Dean R, Skull J (1973) New considerations in use of yeyuno-ileal by-pass in morbid obesity. Ann Surg 177: 723.
- Mason EE (1982) Vertical banded gastroplasty for obesity. Arch Surg 117: 701-706.
- Baltasar A (1982) Mechanical sutures in obesity surgery. Rev Soc Andaluza Patología Digestiva 10: 555-556.
- Andreo L, Lasierra R, Baltasar A (1988) Radiological evaluation of vertical banded gastroplasty. Radiología 30: 303-308.
- Baltasar A (1989) Modified vertical gastroplasty: Technique with vertical division and serosal patch. Acta Chir Scand 155: 107-112.
- McLean LD, Rhode BM, Sampalis J, Forse RA (1993) Results of the surgical treatment of obesity. Am J Surg 165: 155-162.
- Baltasar A, Tomás J, Marcote E (1991) Bariatric surgery: Experience with 100 cases operated. Cir Esp 50: 271-277.
- Baltasar A, Bou R, del Río J (1997) Bariatric surgery: long-term results of vertical banded gastroplasty. A frustrated hope? Cir Esp 62: 175-179.
- Baltasar A, Bou R, Arlandis F, Martínez R, Serra C, et al. (1998) Vertical banded gastroplasty at more than five years. Obes Surg. 8: 29-34
- Favretti F, Cadière GB, Sega G (2002) Laparoscopic banding: selection and technique in 830 patients. Obesity Surgery 12: 385-339.
- Baltasar A, Marcote E, Bou R, Bengochea M, Arlandis F (1991) Exclusión ileal parcial en la hipercolesterinemia. Notas Clinicas 49: 475-478.
- Baltasar A, Bou R, Cipagauta LA, Marcote E, Herrera GR, et al. (1995) Hybrid bariatric surgery: biliopancreatic diversion and duodenal switch. Obes Surg.5: 419-423.
- Martínez RM, Baltasar A (1997) Study of gastric emptying in patients with morbid obesity treated with duodenal crossover. Rev Esp Enf Digest 89: 413-414.
- Baltasar A, Rio JD, Escrivá C, Arlandis F, Martínez R (1997) Preliminary results of the duodenal switch. Obes Surg. 7: 500-504.
- Hess DS, Hess DW (1998) Biliopancreatic diversion with a duodenal switch. Obes Surg 8: 267–282.
- Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, et al (1993) Biliopancreatic Diversion with a New Type of Gastrectomy. Obesity Surgery 3: 29-35.
- Baltasar A, Bou R, Bengochea M, Arlandis F, Escrivá C, et al. (2001) Duodenal switch: an effective treatment for morbid obesity--Intermediate results. Obes Surg 11: 54-59.
- Pérez N, Baltasar A, Serra C, Ferri L, Bou R, et al. (2005) Comparative analysis of vertical banded gastroplasty and duodenal switch at five years follow-up. Obes Surg 15: 1061-1065.
- Deitel M (1989) Surgery for the morbidly obese patient. Lea and Febiger, London.
- Deitel M, Shikora S (2016) Mervyn Deitel-Biography. Obes Surg 26: 707-708.
- Deitel M, Gagner M, Dixon J, Himpens J, Madan A (2016) Handbook of Obesity Surgery. Toronto.
- Balsiger BM, Büchler MW (2001) Update: Surgery for the Morbidly Obese Patient 2000. Bjs 88: 1020.
- Wittgrove A, Clark W, Tremblay L (1994) Laparoscopic gastric bypass, Roux-en-Y: preliminary report. Obes Surg 4: 353-357.
- Wittgrove A, Clark GW (1996) Laparoscopic gastric bypass. Roux-en Y. Experience with 27 cases with 3-18 months follow up. Obes Surg 6: 54-57.
- Wittgrove A, Clark W, Schubert K, Schubert KR (1996) Laparoscopic gastric bypass. Roux-en Y. Technique and results in 75 patients with 3-30 months follow up. Obes Surg 6: 500-504.
- Baltasar A, Bou R, Miró J, Serra C (2000) Gastric bypass by laparoscopy. Cir Esp 67: 556-559.
- Gusfavsson S, Westling A (1998) Laparoscopic Roux-en-Y gastric bypass. Uppsala, Sweden. Obes Surg 8: 392.
- Baltasar A, Bou R, Bengochea M, Miró J, Arlandis F (1998) Lap Roux-Y gastric bypass. Alcoy. Spain. Obes Surg 8: 393.
- Serra C, Baltasar A, Bou R, Miró J, Cipagauta LA (1999) Internal hernias and gastric perforation after laparoscopic gastric bypass. Obes Surg 9: 546-549.
- Higa KD, Ho T, Boone KB (2003) Internal hernias after laparoscopic Roux-en-Y gastric bypass: Incidence, treatment and prevention. Obes Surg 13: 350-354.
- Baltasar A, Bou R, Miró J (2000) Laparoscopic gastric bypass. Bypass gástrico laparoscópico. Rev Esp Enferm Ap Dig 10: 661-664.
- Wittgrove A (2007) Chapter 21: Laparoscopic gastric bypass. Circular stapler technique. Obesity Surgery: Principles and Practice Albany. McGraw Hill Medical, New York. pp: 221-224.
- Ren CJ, Patterson E, Gagner M (2000) Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg 10: 514-523.
- Baltasar A, Bou R, Miro J, Bengochea M, Serra C, et al. (2002) Laparoscopic duodenal switch. Technique and initial experience. Obes Surg 12: 245-248.
- Baltasar A (2007) Hand-sewn laparoscopic duodenal switch. Surg Obes Relat Dis 3: 94-96.
- Baltasar A (2007) Chapter 29: Laparoscopic biliopancreatic diversion. The duodenal switch. Obesity Surgery: Principles and Practice Albany, McGraw Hill Medical, New York, pp: 241-243.
- Baltasar A (2007) The duodenal crossing: Clinical guide of Spanish surgery obesity. Arán Ediciones, Spain.
- Weiner RA, Engert RB, Weiner S, Pomhoff I, Schramm M (2004) Laparoscopic biliopancreatic diversion with duodenal switch: three different duodeno-ileal anastomotic techniques and initial experience. Obes Surg 14: 334-340
- Baltasar A (2000) Obesity and surgery. how to stop being obese. Aran Ediciones, Spain.
- Martínez R, Baltasar A, Vidal V (1997) Study of gastric emptying in patients with morbid obesity operated by duodenal crossover. REED 89: 413-414.
- Bueno J, Pérez N, Serra C, Bou R, Miró J, et al. (2004) Pancreato-cutaneous fistula secondary to postoperative pancreatitis after laparoscopic duodenal crossing. Cir Esp 76: 184-186.
- Serra C, Baltasar A, Losa JL (1999) Cardiac tamponade caused by perforation of central venous catheter. Cir Esp 65: 470-471.
- Baltasar A, Serra C, Pérez N (2004) Clinical hepatic impairment after the Duodenal Switch. Obes Surg 14: 77-83.
- Baltasar A (2006) Liver cirrhosis and bariatric operations. Surg Obes Relat Dis 2: 580-581.
- Baltasar A (2014) Liver failure and transplantation after duodenal switch. Surg Obes Relat Dis 10: e93-e96.
- Serra C, Baltasar A, Pérez N (2006) Total gastrectomy for complications of the duodenal switch. Obes Surg 16: 1082-1086.
- Baltasar A, Bou R, Bengochea M, Serra C (2011) Protein caloric malnutrition. Three types of bowel lengthening. BMI–Latina 1.2.5: 96-97.
- Baltasar A, Bou R, Bengochea M (2010) Fatal perforations in laparoscopic bowel lengthening operations for malnutrition. Surg Obes Relat Dis 20: 140-147.
- Baltasar A (2008) Letter to the editor: Roux-en-Y to duodenal switch. Surg Obes Relat Dis 4: 208-211.
- Baltasar A, Serra C, Pérez N (2005) Laparoscopic sleeve gastrectomy. A multi-purpose operation. Obes Surg 15: 1124-1128.
- Ahmad SS, Ahmad SS, Kohl S (2015) The hundred most cited articles in bariatric surgery. Obes Surg 25: 900-909.
- Serra C, Pérez N, Bou R, Bengochea M, Martínez R, et al. (2006) Gastrectomía tubular laparoscópica. A bariatric operation with different indications. Cir Esp 79: 289-292.
- Sánchez-Santos R, Masdevall C, Baltasar A (2009) Short- and mid-term outcomes of sleeve gastrectomy for morbid obesity: The experience of the Spanish National Registry. Obes Surg 19: 2019-2023.
- Baltasar A, Serra C, Pérez N (2006) Re-sleeve gastrectomy. Obes Surg 16: 1535-1538.
- Baltasar A, Pérez N, Bou R, Miro J, Bengochea M, et al. (2000) Wall-stent prosthesis for severe leak and obstruction of the duodenal switch Gastric tube. Obes Surg 10: 309.
- Serra C, Baltasar A, Andreo L (2007) Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy. Obes Surg 17: 866-872.
- Baltasar A, Bou R, Bengochea M, Serra C, Pérez N (2013) Difficult intubation and tracheotomy in the morbidly obese. BMI-Latina 3: 4-7.
- Baltasar A, Bou R, Bengochea M, Serra C, Pérez N (2015) Laparoscopic gastric sleeve, subtotal antrectomy and omentoplasty. Obes Surg 25: 195-196.
- Baltasar A, Bou R, Bengochea M (2007) Use of a Roux limb to correct esophagogastric junction fistulas after sleeve gastrectomy. Obes Surg 17: 1409-1410.
- Baltasar A, Serra C, Bengochea M, Bou R (2008) The use of a Roux-en-Y loop for sleeve gastrectomy fistulas. Bariátrica Metabólica 3: 20-23.
- Baltasar A, Serra C, Bengochea R (2009) Use of Roux limb as remedial surgery for sleeve gastrectomy fistulas. Surg Obes Relat Dis 4: 759-763.
- Gagner M, Deitel M, Traci L (2009) The second international consensus summit for sleeve gastrectomy, March 19–21. Surg Obes Relat Dis 5: 476-485.
- Deitel M, Gagner M, Erickson A (2011) Third international summit: current status of sleeve gastrectomy. Surg Obes Relat Dis 7: 749-759.
- Baltasar A (2015) Historical note: First diabetes metabolic operation in Spain. Int Obes Dia 25: 180-182.
- Marceau R, Biron S, Marceau S (2014) Biliopancreatic diversion-duodenal switch: Independent contributions of sleeve resection and duodenal exclusion. Obes Surg 24: 1843-1849.
- Bou R, Baltasar A, Pérez N (2012) Diabetes Surgery: Vertical gastrectomy and duodenal deviation. BMI-Latina 2: 400-403.
- Baltasar A, Bou R, Bengochea M, Serra C, Pérez N, et al. (2006) One thousand bariatric operations. Cir Esp 79: 349-355.
- Baltasar A, Serra C, Bou R (2008) Sleeve gastrectomy in a 10-year-old child. Obes Surg 18: 733-736.
- Scopinaro N, Melissas J, Fried M, Baltasar A (2016) European chapter of centers of excellence program.
- Baltasar A (2011) Editorial. BMI-Latina 1: 5-9.
- Baltasar A, Serra C, Bou R (2011) Complications of bariatric Surgery. BMI-Latina 1: 238-242.
- Baltasar A, Bou R, Bengochea M (2011) Open duodenal switch. BMI-Latina 1: 357-360.
- Baltasar A, Bou R, Bengochea M (2012) Laparoscopic hand-sewn duodenal switch. BMI-Latina 2: 387-389.
- Serra C, Pérez N, Bou R, Baltasar A (2014) Sliding self-locking first stitch and Aberdeen Knot in suture reinforcement with omentoplasty of the laparoscopic gastric sleeve staple line. Obes Surg 24: 1739-1740.
- Baltasar A, Bou R, Serra C, Bengochea M, Pérez N (2015) Use of self-locking knots in running intestinal bariatric sutures. Global Surg 2: 100-101.
- Baltasar A, Bou R, Serra C (2016) Stapling of the bougie in the sleeve gastrectomy. Surg Obes Relat Dis 12: 1136-1138.
- Baltasar A (2016) Simple bariatric telemedicine. BMI-Latina 5: 900-901.
- Shikora S, Torres A (2016) Biography: Aniceto Baltasar. Obes Surg 26: 477-478.
- Baltasar A (2008) Nomenclature used in bariatric surgery. Cir Esp 83: 220-221.
- Baltasar A (2009) Gastroplastia o gastrectomía, gastroplasty versus gastrectomy. Cir Esp 85: 325-326.
- Baltasar A (2011) Nomenclature of bariatric terms. BMI-Latina 1: 278.
- Baltasar A (2012) The Royal National Academy of Medicine of Spain says. Vertical gastrectomy is the right term. BMI-Latina 2: 381-383.
- Baltasar A (2012) Laparoscopic sleeve gastrectomy is a misnomer. Surg Obes Relat Dis 8: 127-131.
- Baltasar A (2015) Sleeve-forming gastrectomy is the right terminology. Obes Surg 25: 935-937.
- Baltasar A, Deitel M, Greenstein R (2008) Weight loss reporting. Obes Surg 18: 761-762.
- Baltasar A, Serra C, Bou R, Bengochea M, Pérez N, et al. (2009) Expected BMI after bariatric operations. Cir Esp 86: 308-312.
- Baltasar A, Pérez N, Serra C, Bou R, Bengochea M, et al. (2011) Weight loss reporting: Predicted BMI after bariatric surgery. Obes Surg 212: 367-372.
- Molina A, Fàtima F, Vives M (2016) Usefulness of Baltasar’s expected body mass index as an indicator of bariatric weight loss surgery. Obes Surg.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 4971
- [From(publication date):
February-2017 - Aug 17, 2025] - Breakdown by view type
- HTML page views : 4092
- PDF downloads : 879